The study was approved by ethics committee of the
Regional Medical Research Centre for Tribals (RMRCT), Jabalpur. Informed
consent was obtained from the parents/guardian of all children included in
the survey.
Results
A total of 1112 children aged 1-9 years were
registered. Of these, 1075 (96.67%) were subjected to tuberculin testing
and the test was read in 1056 children (98.23%), giving a test-read
coverage of 94.96%. Of these 1056 children, 774 (73.3 %) had no BCG scar.
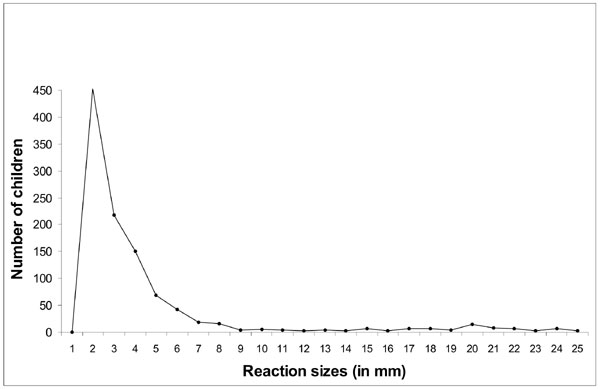
The mode was located at 20 mm in the right hand side of the frequency
distribution of reaction sizes of children (Fig. 1). Using
mirror-image method(9), 66 children were found to be infected and the
prevalence of infection in children was estimated as 6.3% (95% CI:
4.8-7.7). The ARTI was computed as 1.2 % (95% CI: 0.9-1.5). There was no
difference in risk of infection between male and female children (1.1%;
95% CI:0.7-1.5 vs 1.2%; 95% C.I: 0.8-1.6). The prevalence of
infection was significantly higher among children aged 5-9 years compared
to those aged 1-4 years (2.1%; 95% CI: 0.7-3.4 vs 9.2%; 95% CI:
6.9-11.5) (P<0.001).
 |
|
Fig. 1 Frequency distribution of reaction
sizes among children irrespective of BCG scar. |
The anti-mode was visible at 9-10 mm. in the frequency
distribution of reaction sizes (Fig. 1). Using the anti-mode
at 10 mm, 87 children were found to be infected and the prevalence of
infection was estimated as 8.2% (95% CI: 6.6-9.9). The ARTI was computed
as 1.6% (95% CI: 1.2-1.9). The difference in the prevalence of infection
estimated by the anti-mode method using the cut-off at 10mm and
mirror-image method using the mode at 20 mm was statistically not
significant (P>0.05).
Discussion
The results of the study throw light on the current TB
situation amongst the tribal communities of Jhabua district and will serve
as a baseline data for evaluating the impact of disease control measures
and epidemiological trends in the coming years. The ARTI of 1.6% is much
higher than the rates of <0.1% seen in most developed countries [10]. In
India, in a Nation-wide survey conducted during 2000-03, the ARTI rates
ranged from 1.0 to 1.9% in the different zones of the country [11].
A limitation of the study was that the prevalence was
estimated based on a small population and may not be as precise as that
would have been obtained from a larger population.
Information available on the ARTI among tribal
communities in the country shows a varied picture. A previous survey in
the tribal population of North Arcot district in southern India showed a
prevalence of infection of 5% and an ARTI of 1.1% [2]. An earlier survey
in the tribal community of the Car Nicobar islands however showed a much
higher prevalence of infection (16.4%) and ARTI (2.4%) [4]. A recent
survey among the Saharia tribal community of Madhya Pradesh also found
high rates of prevalence of infection at 20.4% and an ARTI of 3.9% [5].
The reasons for this varied picture amongst the different tribal
populations need to be studied further for better understanding of the
situation.
The study findings suggest that the TB situation
amongst the Bhils and Bhilalas of Jhabua district, Madhya Pradesh, is
similar to that amongst the non-tribal population in India. The Revised
National TB Control Programme (RNTCP) was implemented in this district
only in 2003 and is expected to have an impact on the TB situation.
However, there is a need to strengthen and further intensify TB control
measures in the area.
|
What This Study Adds?
• The study provides a baseline data on
prevalence of tuberculosis infection and ARTI amongst tribal
communities of Jhabua district of Madhya Pradesh.
|
References
1. World Health Organization (WHO).
Global Tuberculosis Control 2008: Surveillance, Planning, Financing. WHO/HTM/TB/2008.393.
Geneva: WHO. 2008.
2. Datta M, Radhamani M P, Sadacharam K, Selvaraj R,
Rao DL, Rao RS, et al. Survey for tuberculosis in a tribal
population in North Arcot District. Int J Tuberc Lung Dis. 2001;5:240-9.
3. Chakma T, Vinay Rao P, Pall S, Kaushal LS, Datta M,
Tiwary RS. Survey of pulmonary tuberculosis in a primitive tribe of Madhya
Pradesh. Indian J Tuberc. 1996;43:85-9.
4. Murhekar MV, Kolappan C, Gopi PG, Chakraborty AK,
Sehgal SC. Tuberculosis situation among tri-bal population of Car Nicobar,
India, 15 years after intensive tuberculosis control project and
implementation of a national tuberculosis programme. Bull World Health
Organ. 2004; 82:836-43.
5. Rao VG, Gopi PG, Yadav R, Sadacharam K, Bhat J,
Subramani R, et al. Tuberculosis infection in Saharia, a primitive
tribal community of Central India. Trans R Soc Trop Med Hyg.
2008;102:898-904.
6. World Health Organization (WHO). Generic Guideline
for the estimation of Annual Risk of Tuberculosis Infection. SEA-TB-286
Regional Office for South-East Asia, New Delhi: WHO. 2006.
7. Chadha V K, Vaidyanathan P S, Jagannatha P S,
Unnikrishnan K P, Savanur S J, Mini P A. Annual risk of tuberculosis
infection in the western zone of India. Int J Tuberc Lung
Dis.2003;7:536-42.
8. Bleiker MA, Sutherland I, Styblo K, Ten am HG,
Misljenovie O. Guidelines for estimating the risk of tuberculous infection
from tuberculin test results in a representative sample of children. Bull
Int Union Tuberc Lung Dis.1989; 64:7-12.
9. Arnadottir T, Rieder HL, Trebucq C, Waaler HT.
Guidelines for conducting tuberculin skin test surveys in high prevalence
countries. Tubercle Lung Dis 1996; 77 (Suppl): 1-20.
10. Murray CJL, Styblo K, Rouillon A. Tuberculosis in
developing countries: burden, intervention and cost. Bull Int Union Tuberc
Lung Dis. 1990;65;6-26.
11. Chadha VK, Agarwal S P, Kumar P, Chauhan LS,
Kolappan C, Jagnath PS, et al. Annual risk of tuberculous infection
in four defined zones of India: a comparative picture. Int J Tuberc Lung
Dis.2005;9:569-75.
12. Rao VG, Gopi PG, Yadav R, Subramani R, Bhat J,
Anvikar AR, et al. Annual risk of tuberculosis infection among
tribal population of central India. Trop Med Int Health.2008;13:1372-7.

