|
|
|
Indian Pediatr 2009;46: 72-74 |
 |
Measles with Acute Disseminated
Encephalomyelitis (ADEM) |
|
J Chowdhary, SM Ashraf and K Khajuria
From the Department of Pediatrics, G.B. Pant Hospital,
Govt. Medical College, Srinagar, India.
Correspondence to: Dr Javed Chowdhary Prof. & Head,
Department of Pediatrics, G B Pant General Hospital, B B,
Cant Sonwar, Srinagar, 190 001, J & K, India.
E-mail:[email protected]
Manuscript received: June 25, 2007;
Initial review completed:December 10, 2007;
Revision accepted: March 18, 2008. |
|
Abstract
We report a seven year old male with measles
associated acute disseminated encephalomyelitis (ADEM) despite
having received measles vaccination in infancy. The diagnosis was based
on serum antimeasles antibodies and MRI brain. The patient was managed
with high dose corticosteroids along with supportive measures. There was
a complete neurologically and physica recovery.
Keywords: Demyelination, Inflammatory encephalomyelitis, Measles,
Post infectious encephalomyelitis.
|
|
A cute
disseminated encephalomyelitis is an inflammtory demyelinating illness
distinguished by monophasic course frequently associated with infections
(post infectious) or antecedent immunization (post vaccination)(1, 2). Due
to control of most vaccine- preventable diseases, most cases of ADEM occur
in developing countries and are seen secondary to non-specific upper
respiratory tract infections(3). We present a case of measles associated
ADEM despite the child having received single-dose measles vaccine during
infancy.
Case Report
A 7 year old male was brought with complaints of fever
for 4 days and generalized rash, bodyache and drowsiness on day 5 of
illness. The child had received all the vaccines from our hospital
including the single-dose of measles vaccine at the age of 9 months. On
examination, the patient was febrile with non-pruritic erythmatous
maculopapular rash with ‘Kopliks’ spots, no lymph nodes, mild pallor, and
no icterus. The Glasgow coma scale was 12/15. There were no signs of
meningeal irritation. Fundoscopy, cranial nerves and higher functions were
normal. There was hypertonia, hyperreflexia, and right upper motor neuron
hemiperesis. Other systems were normal. The child progressively
deteriorated in the first 2 days, was comatosed (GCS 5/15) and remained in
this condition for 4 days, he also had convulsion and decerebrate
rigidity. Routine hematological and biochemical investigations including
renal and liver function tests were normal.
Arterial blood gas analysis, stool examination for pH
and reducing substances, urine for reducing sugars and ketone bodies were
normal. Electrolytes, X-ray skull, bones and chest, USG abdomen were also
normal. CSF was grossly clear with 11-15 WBC/dL of which 80% were
lymphocytes with normal protein and sugar values. CSF sent for bacterial
culture was sterile. IgM antibodies for measles were positive in blood
(156mg/dL), however, CSF antigen or antibodies could not be measured. EEG
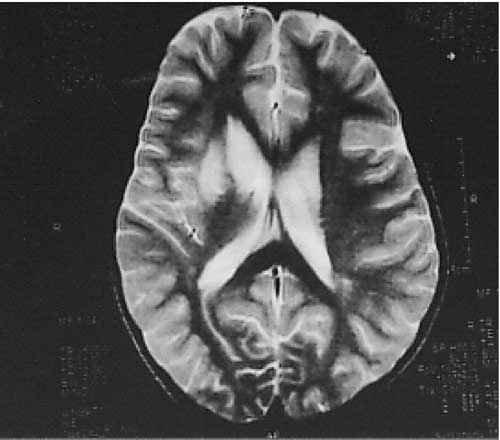
findings were non specific. MRI revealed hyperintense signals on T 2
weighted sequence over bilateral subcortical areas and cerebral cortices
with involvement of midbrain, cerebellar puduncles, thalamus and basal
ganglion, suggestive of ADEM (Fig 1).
 |
|
Fig 1. MRI Brain showing FLAIR
sequence hyperintensities of cortical and subcortical structures. |
Patient was isolated and treated on routine protocol
for measles and intravenous methyl-prednisolone 30mg/kg/day was given for
3 days. Subsequently, intravenous dexamethasone was administered
for next 10 days followed by oral prednisolone for another 7 days. The
child remained aphasic for first twenty five days but recovered slowly
over next six months. Six months later the child recovered completely
neurologically and physically, the repeat MRI scan was also normal.
Discussion
Clinical features including fever, rash, koplik spots,
drowsiness, rapid neurological deterioration, presence of serum IgM
antimeasles antibodies, MRI findings and subsequent improvement with high
dose corticosteriods led us to the diagnosis of measles associated ADEM.
However, it is difficult to differentiate it from SSPE presenting as ADEM
but presence of myoclonic convulsions, typical EEG findings, latent period
and no improvement with steroids and raised CSF/serum measles antibody
titers can differentiate it from SSPE(4). There was no partial or complete
paraplegia or quadriplegia, diminished or loss of reflexes as occurs in
myelitic form of ADEM(5).
Post infectious encephalomyelitis is associated with
concomitant or antecedent infection, usually viral. Most notoriously,
measles virus infection is followed by ADEM in approximately 1 in 1000
unvaccinated children and tends to produce more serious phenotype(6).
Bilateral optic neuritis, ataxia, transverse myelitis, cranial nerve
involvement and rarity of seizures are suggestive of ADEM(7), is contrary
to our case who had a florid, monophasic and polysymtomatic presentation
despite already vaccinated and did not have any residual effect in spite
of such explosive illness.
Because of contagiousness of measles, even sustained
high coverage with single-dose strategy does not prevent large out breaks
of measles with significant morbidity and mortality. So a second
opportunity for measles immunization is essential for effective measles
control, as is done in England and Wales, Albania, Romania, Oman, Shondong
and Heman provinces of China and USA(8), our case report also favours that
a single-dose vaccination is not sufficient for good control of measles
and its neurological complications.
Contributors: Manuscript and the report was
designed and prepared by SMA, revised by KK, and supervised and guided by
JC.
Funding: None.
Contributors credits: None stated.
References
1. Tenembaum S, Chitins T, Ness T, Hahn JS. Acute
disseminated encephalomyelits, Neurology 2007; 68: S 23-26.
2. Kesselring J, Miller DH, Robb SA. ADEM MRI findings
and distinction from multiple sclerosis. Brain 1990; 113: 291-302.
3. Samile N, Hassem T. ADEM in children a descriptive
study in Tehran Iran. Saudi Med J 2007; 3: 396-399.
4. Comert S, Vitrinel A, Gursu HA, Deniz NC, Akin Y.
Subacute sclerosing panencephalitis presenting as acute disseminated
encephalomyelitis. Indian J Pediatr 2006; 73: 1119-1121.
5. Ropper AH, Brown RH. In Adams and Victors Principles
of Neurology. 8th ed. New York: Medical Publishing Division, McGraw-Hills;
2005. 790-792.
6. Bennetto L, Scolding N. Inflammatory/post-infectious
encephalomyelitis. Journal Neurol, Neurosurg Psychiatry 2004; 75: 122.
7. Dale RC. Acute disseminated encephalomyelitis. Semin
Pediatr Infect Dis 2003; 14: 90-95.
8. Strebel P, Cochi S, Grawbosky M, Bilous J, Hersh BS,
Okwo-Bele JM, et al. The unfinished measles immunization agenda. Infect
Dis 2003; 187: S1 – S7. |
|
|
 |
|

