Mala Bhalla,
Rashmi Sarkar
Priti Arun
Amrinder J. Kanwar
From
the Departments of Dermatology and Venereology &
*Psychiatry, Government Medical College & Hospital, Sector
32, Chandigarh 160 047, India.
Correspondence
to: Dr. Rashmi Sarkar, C/o. Mrs. C. Sarkar, Teachers’ Flats
No. 9, Sector 12, P.G.I. Campus, Chandigarh 160 012,
India. Email: [email protected]
Manuscript
Received: October 31, 2001;
Initial review completed: November 28, 2001;
Revision Accepted: September 27, 2002,
Trichotillomania,
though uncommon, is one of the causes of unexplained hair loss,
especially in children. Three girls in the age group of 4-6 years
were observed in our pediatric dermatology clinic to have
trichotillomania. In one child, there was co-existent alopecia
areata. All were referred to the child guidance clinic and they
all showed improvement with behavior therapy. A close liasion
between the dermatologist, psychiatrist and parents would go a
long way in preventing this alopecia.
Key words:
Children, trichotillomania.
Trichotillomania is
a disorder of compulsive hair pulling that results in
alopecia(1,2). While in dermatology, trichotillomania is
classified as a self-inflicted dermatosis, in psychiatry, it is
classified as an impulse-control disorder(3) along with conditions
such as compulsive gambling and kleptomania. Trichotillomania in
children is commonly associated with nail biting, thumb sucking,
anxiety and learning disability while adult patients show more
diverse psychopathology with depression, anxiety,
obsessive-compulsive disorder and panic attacks. Hair pulling and
plucking is commonest from the frontoparietal and temporal regions
of the scalp, often on the non-dominant side of the scalp although
occasionally the eyelash, eyebrow, pubic and hair on other body
sites may be involved(2). We describe three girls with
trichotillomania who presented with loss of hair over scalp and
other parts of the body; one of the patients had co-existing
alopecia areata.
Case Reports
Case 1:
A 4-year-old girl presented with loss of hair over the scalp of 6
months duration, since the time she had started going to school.
Examination revealed an irregular, coarse patch of hair loss over
the left frontal region of the scalp (Fig. 1). Short,
broken hairs of variable length were present, palpable as a
stubble. There was no evidence of scaling or inflammation, the
hair at the margin were not easily pluckable and the hair over the
rest of scalp was normal in texture and strength. There was no
history of loss of appetite, abdominal pain, diarrhea or
constipation. Examination of the mucous membranes, nails, oral
cavity and abdomen was normal. On questioning, the mother revealed
that this child was constantly fighting with her brother, was
obstinate and quick to take offense. Child was the youngest of
three siblings and pampered a lot by the grandparents. The mother
used to hit her often on undesirable behavior e.g. hair
pulling with her fingers when sitting idle and fighting. This
would often result in the child becoming angry and pulling out
more hair.
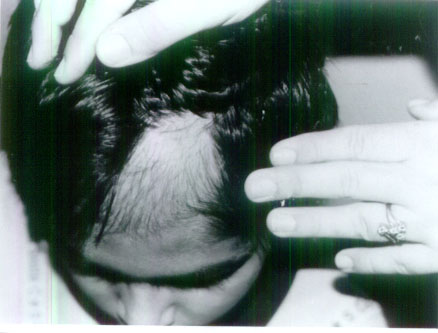 |
| Fig.1. A coarse patch of
loss of hair over left frontal area scalp with short broken
hairs. |
Case 2:
A 4-year-old girl presented with loss of hair over the vertex of
the scalp of 1-year duration. She had developed a small, bald
patch over the vertex of the scalp, which gradually increased in
size. There was no scaling but short exclamation mark hairs were
present which were confirmed on light microscopy of the hair; the
hair over the rest of the scalp was normal in texture and
strength. The rest of the cutaneous and systemic examination was
normal. Potassium hydroxide (KOH) examination of the hair was
negative. She was diagnosed as alopecia areata and was initially
treated with topical steroids for 4 weeks and later oral steroids
(prednisolone 10 mg OD) were given for 8 weeks. There was some
improvement in the form of hair regrowth but after a while the
baldness started extending on one side. On examination, coarse
irregular patches of hair loss with few short broken hair of
varying lengths palpable as a stubble were present on the left
temporal region of the scalp. No exclamation mark hair were seen.
The parents, on questioning, revealed that they had noticed the
child pulling out her hair from the sides of the scalp which was
not related to any activity. She was willful, frequently threw
temper tantrums, had the habit of thumb sucking and was the only
child of her parents.
Case 3:
A 6-year-old girl presented with loss of hair over the scalp of 4
years duration. The mother gave the history that the child
initially used to pluck out hair from the left parietal region of
the scalp, but since the last 6 months the child had started
pulling hair from the right parietal and temporal areas. Six
months back, the school of the child had been changed. She had the
habit of thumb sucking. The rest of the history, cutaneous and
systemic examination were similar as in case 1.
A potassium
hydroxide examination and light microscopic examination of the
hair was done in all cases which did not reveal any abnormalities.
A diagnosis of trichotillomania was considered in all three cases
though the second patient also had co-existing alopecia areata.
The parents were advised to shave the affected area and watch for
hair regrowth. The children were referred to the child guidance
clinic for behavior therapy where they were seen by a
psychiatrist, who also ruled out other psychiatric ailments. All
three girls had normal IQ. Parental counseling was dne for nature
of illness, to stop using physical punishment and to bring
consistency in discipline. The patients received several sessions
of play therapy, which were aimed at conflict identification, and
suggestion. Distraction was taught, to be used by parents.
Differential reinforcement was used where good behavior was
rewarded and rewards were withdrawn whenever there was undesirable
behavior. Along with these the first and the second child were
asked to make star charts and were rewarded with play sessions.
The first two patients benefited from therapy and their hair
showed re-growth on the shaved area and they stopped pulling out
the hair. The re-growing hair was of fairly uniform length though
thinner; and light microscopy revealed the hair ends to be
fractured. In the case of the third patient, after the counselling
and two sessions with the psychiatrist, the mother reported that
the child had stopped pulling hair from the scalp but had started
doing the same from the legs, as a consequence of which, patches
of hair loss were present over the legs. So, she was referred once
again to the child guidance clinic. However, subsequently the
child was lost to follow-up.
Discussion
Trichotillomania is
a term coined by Hallopeau, a French dermatologist, in 1889(4). It
literally means a morbid craving to pull out hair. It may have a
multifaceted etiology, including alteration in brain metabolism, a
positive family history, a disturbed social setting and possibly
maternal deprivation(5). It occurs worldwide including in Indian
setup, and may prove to be a serious condition, if accompanied by
trichophagy and trichobezoar(6,7). Trichotillomania occurs more
than twice as frequently in females as in males in the adult age
groups, but below the age of 6 years boys outnumber girls by 3:2
ratio, although others have found the male to female ratio in
children to be 1:1(5). In clinical setting, the disorder
predominantly affects females(3), as also observed in the present
cases.
In psychiatry,
trichotillomania is classified under impulse control disorders(3).
Features of trichotillomania that fit this description include the
inability to resist urges to pull one’s hair which was present
in these cases and mounting tension before pulling and feeling of
relief afterwards which may not always be forthcoming especially
in a small child(8). However, in the present cases, the parents
had noticed the children pulling out the hair unconsciously or
deliberately. Moreover, the disturbance could not be accounted for
by another mental disorder or any dermatological condition and the
condition caused significant clinical distress, both of which were
other features, which supported the diagnosis. The child develops
the habit of twisting hair around his fingers and pulling it,
which is only partially conscious and may replace the habit of
thumb sucking(9) as observed in two patients. Other associated
clinical features include nail biting and temper tantrums. Hair
pulling and twirling is a normal aspect of behavior in children
and young adults and assumes clinical importance only when
significant alopecia develops(9).
It is usual for
trichotillomania to occur in a rather disturbed social setting.
Young girls may utilize this condition to avoid being sent to
school and to induce the parents to give in to their demands(9) as
noted in two of our patients. In early childhood, the factors
contributing to the emotional strain, which leads to
trichotillomania, are almost always found in a conflicting
mother-child relationship whereas, at the school-going age, it
usually results from the pressure on a child to achieve more or
sibling rivalry, which could be the case in the first patient.
From the psychodynamic point of view, hair may be regarded as a
‘transitional object’, which acts as a comforter to the child
who is distanced by the mother from the breast(9).
Alopecia areata and
trichotillomania present the most frequent causes of circumscribed
hair loss in children and can occur together in childhood(10), as
observed in the second patient. The connection between the two is
not very clear but it has been proposed that trichotillomania may
result from scratching at the site of alopecia areata that is
symptomatic with pruritus, initiating a habit-forming behavior, or
patients with a mental predisoposition may artificially prolong
the disfigurement as the hair on the bald patches of alopecia
areata regrows(10). Skin biopsy is useful for documenting the two
conditions (but was refused by the parents), although these can be
diagnosed easily by the dermatologist.
Early onset
trichotillomania, beginning before the age of six years is usually
self-limiting and responds to simple interventions involving
suggestion, reassurance and simple behavioral treatment
approaches(11), as was done in the present cases as well. In
children, the drug therapy which includes selective serotonin
reuptake inhibitors, tricyclic antidepressants, neuroleptics and
lithium carbonate is rarely used(5). Trichotillomania may be
uncommon but must be thought of in cases where there is ambiguous
loss of hair in childhood with no apparent underlying cause and
where the scalp is normal or where almost no hair is lost by
combing or gentle pulling. Trichotillomania is best overcome by an
interdisciplinary approach to treatment and a liaison between the
dermatologists, psychiatrist and the parents is needed for the
effective management of this condition.
Contributors:
MB worked up the patients clinically, reviewed the literature and
drafted the manuscript. RS was the consultant-in-charge, provided
the concept, co-drafted the manuscript and revised it critically.
PA was the psychiatrist who treated the patients, co-drafted the
manuscript and revised it critically. AJK has overall critically
revised and approved of the manuscript in its final version. RS
shall act as the guarantor.
Funding:
None.
Competing interests:
None stated.
1. Cotterill JA,
Millard LG. Psychocutaneous Disorders. In: Champion RH,
Burton JL, Burns DA, Breathnach SM, eds. Textbook of
Dermatology. 6th ed. Oxford, England: Blackwell Scientific
Publication 1998; pp 2785-2814.
2. Minichiello
WE, O’ Sullivan Rl, Osgood-Hynes D, Baer L. Trichotillomania:
clinical aspects and treatment strategies. Harv Rev Psychiatry
1994; 1: 336-344.
3. Christenson
GA, Crow SJ. The characterization and treatment of
trichotillomania. J Clin Psychiatry 1996; 57 (Suppl 8): 42-47.
4. Hallpeau H.
Alopecie par grattage (trichomanie ou trichotillomanie). Ann
Dermatol Syphiligr 1889; 10: 440-446.
5. Jefferson JW,
Greist JH. Trichotillomania - A Guide. 1st ed. Madisson
Institute of Medicine: Obsessie Compulsive Information Centre,
1998.
6. Sood AK, Behl
L, Kaushal RK, Sharma VK, Grover N. Childhood trichobezoar.
Indian J Pediatr 2000; 67: 390-391.
7. Sharma NL,
Sharma RC, Mahajan VK, Sharma RC, Chauhan D, Sharma AK.
Trichotillomania and trichophagia leading to trichobezoar. J
Dermatol 2000; 27: 24-26.
8. Burt VK.
Impulse-control disorders not elsewhere classified. In:
Kaplan HI, Sadock BJ, eds. Textbook of Psychiatry. 6th edn.
Baltimore, Williams and Wilkins, 1995; 1412-1415.
9. Cotteril JA.
Trichotillomania: a manipulative alopecia. Int J Dermatol 1993;
32: 182-183.
10. Trueb RM,
Cavegan B. Trichotillomania in connection with alopecia areata.
Cutis 1996; 58: 67-70.
11. International Classification
of Diseases. The ICD-10 Classification of Mental and Behavioural
disorders; Clinical description and diagnostic guidelines. 10th
edition. World Health Organization 1992.
|
