P. Kusuma Kumary, T. Priyakumari, V.G. Chell am, Francis V. James and M. Krishnan Nair
From the Division of Pediatric Oncology and Radiation Oncology, Regional Cancer Center, Trivandrum, Kerala, India and Department of Pathology, Medical College, Trivandrum, Kerala, India.
Reprint requests. Dr. P. Kusuma Kumary. Associate Professor of Pediatric Oncology, Regional Cancer Centre, Post Box No. 2417, Medical College, Trivandrum,
Kerala - 695 011, India. Fax: 0471-447454.
Manuscript received: March 20,1998; Initial review completed: May 13,1998;
Revision accepted: August 3, 1998
Abstract:
Objective: To study the clinical profile and outcome of Langerhans cell histiocytosis in children upto 2 years of life; Design: Retrospective analysis.
Methods: Medical records of children upto 2 years of age with a diagnosis of Langerhans Cell Histiocytosis (LCH) were analyzed. Their clinical pattern, treatment modalities and outcome were studied. The patients were categorized
into
2 groups according to' their clinical presentation: (i) Subjects without organ dysfunction;
and (ii) cases with organ dysfunction. Treatment consisted of surgical intervention radiotherapy, chemotherapy or combination of all these modalities depending upto the extent of disease. Results: There were 20
children upto 2 years of age with histiocytosis during the 12)ear period (January 1983
-
December 1994). The median age at diagnosis was 18 months (range 52 days
-
24 months). Of the twenty patients, 13 patients didn't have organ dysfunction and 7 had organ dysfunction. Out of the "13 children without organ dysfunction eleven patients received treQ1ment and all of them are alive free of disease with a median follow up of 62 months. But all children with organ dysfunction succumbed to diseases within a few weeks. Conclusion: Children under 2 years of age with localised and or multifocal LCH without organ dysfunction have a good prognosis and they should not be exposed to aggressive form of treatment. All
children with organ dysfunction require multi-agent chemotherapy.
Key words: Chemotherapy, Langerhans cell histiocytosis.
LANGERHANS cell histiocytosis (LCH) is a proliferative disorder of histiocyte
and is characterized by heterogenous clinical manifestations and unpredictable clinical course. The cause of LCH remains unknown; immunologic and clonal proliferation etiologies have been suggested. Patients can experience spontaenous remissions and exacerbations. Subjects with localised disease have a
good prognosis with 100% survival in man} of the reported series(1-4). Disseminated disease has been associated with a' chronic course, high rate of morbidity and late consequences and possible mortality. There is uniform
agreement that the best prognostic parameters currently available are age, extent of disease and presence organ dysfunction as defined by Lahey in 1975(5). Many studies
confirm that children under 2 years of age with organ dysfunction form the poorest prognostic group. A variety of therapeutic agents have been used singly and in combination with varying degree Of success in these children(6). This communication describes the clinical picture, response to therapy, complications and outcome in LCH
in children below 2 years
-
of age at 04r
center.
Subjects and Methods
From January 1983 to December 1994, 57 children with a diagnosis of LCH were registered in our center of which 20 children were below the age of 2 years and these were analysed. In all of these children, diagnosis was based on clinical and histopathologic data. Laboratory studies included complete blood count, urinalysis, chest X-ray, skeletal survey, liver function tests and renal function tests. Bone marrow studies were also done when abnormalities were detected in peripheral blood examination. Diagnosis was established by biopsy of the lesion (skin/lymph node) in all cases. A presumptive diagnosis of LCH
was made based on the light microscopic features.
The following parameters were evaluated: age at diagnosis extent of disease, absence or presence of organ dysfunction, treatment utilized, response to therapy and out- come. Lahey's criteria for organ dysfunction was used to identify patients with hepatic, hematopoietic. and pulmonary dysfunction. Liver dysfunction was considered present when there was one or more of the following abnormalities: Hypoproteinemia
(total protein <55 g/dl or albumin <2.5 g/dl), edema, ascites and or hyper biliru-binemia (total bilirubin> 1.5 mg/dl, not attributable to hemolysis).
Liver enlargement alone was not considered indicative of liver dysfunction in
the absence of liver function abnormalities. Hematopoietic dysfunction was defined as anemia (Hb <10 g/dl not due to iron deficiency or super imposed infection) and or leukopenia (leukocyte count
<4000
cells/ cumm) and/or neutropenia (neutrophil count <1500 cells/.cumm) and/or thrombocytopenia (platelet count. <100,000 platelet/cumm).
Pulmonary dysfunction was defined by presence of tachypnea and/Dr dyspnea, cyanosis, cough with pulmonary infiltrate, pneumothorax and pleural effusion, not attributable to superimposed infection.
Treatment consisted of surgical intervention (biopsy, curettage or excision), radiotherapy, chemotherapy or combination of all these modalities. Patients with localized disease were treated with surgery with or with- out radiotherapy. Chemotherapy was used in patients with multiple lesions at
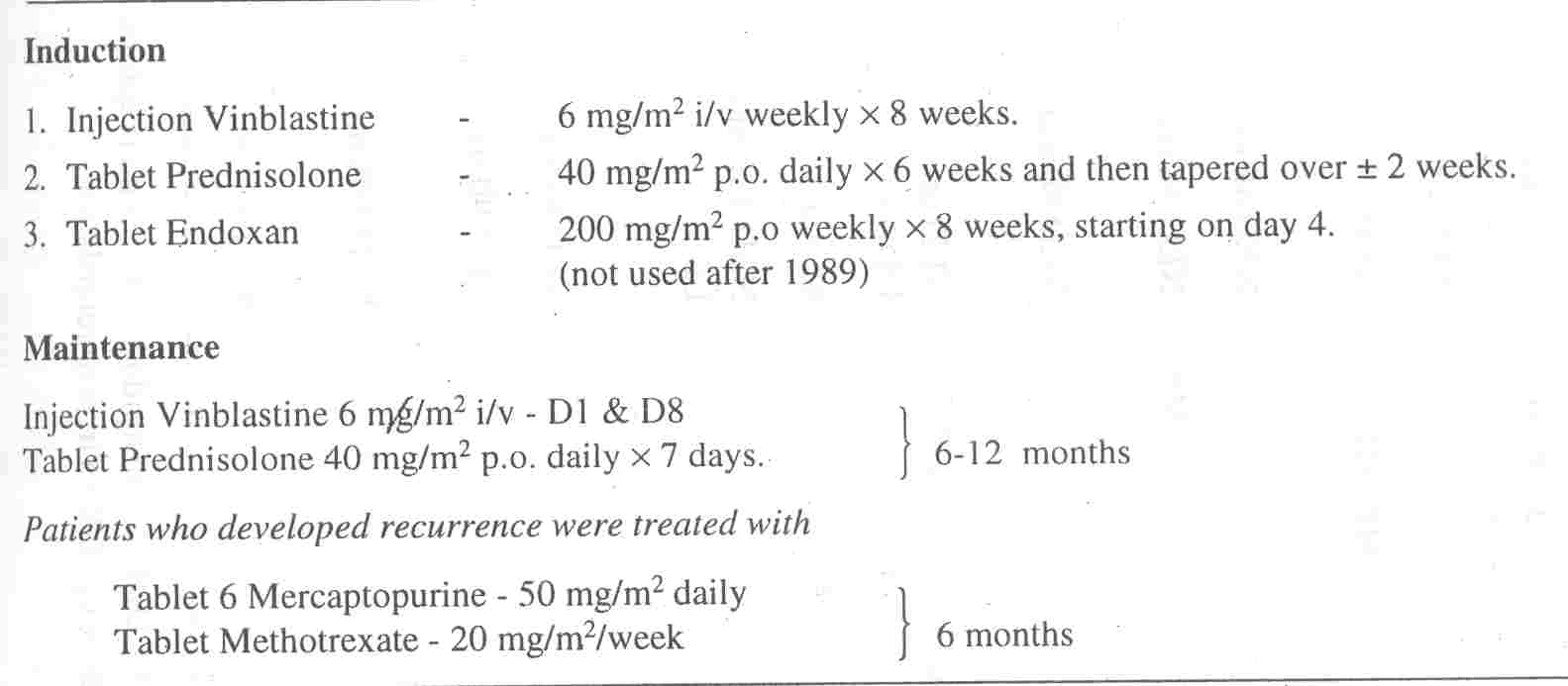
diagnosis,. Chemotherapy protocol used is summarized in Table I.
|
TABLE I
Chemotherapy Protocol Used. |
 |
Treatment response was assessed as per Raney's criteria(1). Complete response
was defined as the disappearance of all evidence of disease, partial response as
lesions shrinking by at least 50% and stable disease as <50% reduction of lesion without any evidence of new lesion. Worsening of lesions were considered as evidence of progressive disease. The duration of survival was calculated from the date of diagnosis.
Results
Patients ranged in age from 52 days to 24
-
months, the median age at diagnosis was -18 months. The male to female ratio was 1.2: 1. The median follow up for surviving patients was 62 months (range 34-161 mo).
Table II shows the site of disease, treatment modality, duration of treatment, response to treatment and current status of 13
children without organ dysfunction. Three patients had skull lesions only, 9
cases had multi focal lesions and one subject had a posterior ethmoidal mass that extended intracranially.
TABLE II - Patient
Characteristics Without Organ Dysfunction
|
No. |
Age
(Mo) |
Sex |
Sites involved |
Treatment & duration |
Response
(Mo) |
Recurrence
site & time |
Retreatment & duration
|
Current Status |
Sequelae |
|
1 |
13 |
M |
Skull tibia, skin |
VB, PDN 12m |
Complete |
Nil |
- |
NED 40 mo |
Nil |
|
2 |
23 |
M |
Maxilla, vertex, mandible |
VB, PDN 6m |
Complete |
Skull 12 mo
Gums 18 mo |
6 MP, MTX
6 mo |
NED 42 mo |
Nil |
|
3 |
24 |
F |
Skull |
Biopsy |
Complete |
Nil |
- |
NED 40 mo |
GR |
|
4 |
22 |
F |
Skull c1+c2 vertebrae |
RT 600/4F to vertebrae |
Complete |
Skull, gum
18 mo |
Steroids, 6MP 6 mo |
NED 44 mo |
GR |
|
5 |
18 |
F |
Fever, Skull skin, gum paronychia |
VB, PDN 12m |
Complete |
- |
- |
NED 60 mo |
|
|
6 |
18 |
M |
Mastoid gum, skin |
VB, PDN |
Complete |
DI, gum, skull 24 mo |
6MP, MTX, VB |
NED on DDAVP |
Nil |
|
7 |
10 |
M |
Periorbital swelling |
RT 600/4F |
Complete |
- |
6 mo |
65 mo |
- |
|
8 |
19 |
F |
Skin, otitis, skull, liver, spleen |
Refused tt |
Complete |
- |
- |
NED 136 mo LFU |
Nil |
|
9 |
10 |
M |
Skin LN, Liver, Spleen |
Refused tt |
Complete |
- |
- |
- |
Nil |
|
10 |
9 |
M |
Skull |
Biopsy |
Complete |
- |
- |
NED 88 mo |
Nil |
|
11 |
24 |
F |
Clavicle, skull, femur |
VB, PDN RT tofemur 6 m |
Complete |
- |
- |
NED 90 mo |
Nil |
|
12 |
48 |
F |
Posterior ethmoid swelling extending
intracranially |
Excision+ RT 600/4F |
Complete |
- |
- |
NED 108 mo |
|
|
13 |
24 |
M |
Ottis, skull, mastoid |
RT 600 cy/3F |
Complete |
- |
- |
NED 161 mo |
|
LN - Lymphnode; VB -
Vinblastine; PDN - Predinisolone; RT - Radiotherapy; tt - Treatment;
DI - Diabetes insipidus; MP - 6 mercaptopurine; MTX - Methotrexate;
NED - No evidence of disease; DDAVP - Desmopressin; LFU - Lost for
follow up; GR - Growth retardation
Table II also shows site of disease, treatment modality, duration, of
treatment response to treatment and. current status of seven children with organ
dysfunction. Two
patients had hepatic and hematopoietic dysfunction, 3 had hematopoietic dysfuction, one had hematopoietic, hepatic and pulmonary dysfunction and one had hepatic dysfunction alone.
TABLE II - Patient
Characteristics with Organ Dysfunction
|
No. |
Age (mo) |
Sex |
Clinical |
Organ dysfunction |
Treatment |
Response |
Outcome |
|
1. |
24 |
F |
Fever, Jaundice, pallor, skin lung
bones, hepatosplenomegaly |
Hepatic, Hematopetic & pulmonary |
VB PDN |
Nil |
DOD 2nd week |
|
2. |
18 |
M |
Skull, skin BM, liver |
Hepatic &Hematopetic |
VB, PDN, Endoxan |
Nil |
DOD 4 week |
|
3. |
7 |
M |
Skin, ear, gum, BM, Liver, Spleen |
Hematopetic |
Nil |
- |
Refused it |
|
4. |
3 |
F |
Skin, LN, liver, spleen |
Hepatic |
VB, PDN |
|
Died 2nd day |
|
5. |
18 |
F |
Skin, Otitis, anemia, purpura, liver |
Hematopetic |
- |
- |
Refused it |
|
6. |
24 |
M |
Skull, skin, liver, spleen, BM |
Hepatic &Hematopetic |
VB, PDN, Endoxan |
- |
DOD 2nd week |
|
7. |
2 |
M |
Fever, skin, pupura, diarrhea,
hepatosplenomegaly |
Hematopetic |
- |
- |
Expired before it |
BM - Bone marrow; LN -
Lymphnode; VB - Vinblastine; PDN - Prednisolone; DOD - Died of
disease; TT - Treatment
Of the 13 patients without organ dysfunction, 2 patients were lost for follow up and 11 patients were evaluable
for treatment response. Two patients with skull lesion had only biopsy, 4 patients had radiation (RT)
also and 5 patients received chemotherapy. Complete response was noted in all
these patients. Four patients developed recurrences, one in RT alone group and
others in chemo- therapy group. Three patients had recurrences more than once. All of them were salvaged with further chemotherapy. The
sequelae noted were growth retardation in two patients, diabetes insipidus in one, loss of teeth in 2 patients and chronic otitis in one patient.
Two of the seven patients with organ dysfunction were not treated because of parents refusal. Two patients died of disease before any form' of treatment
was started. One patient died the day after treatment was started. Other two patients died of progressive disease within 4 weeks of starting chemo- therapy. Thus, none of the patients in this group is alive at present.
Discussion
LCH is a comparatively rare disease and constitutes about 2% of all pediatric malignancy cases registered in our centre. Although, there is no evidence that LCH is a malignant process, its course is often un- predictable. Pathogenesis of LCH is still unknown
and so the approach to treatment is empirical, not rational. Management of patients with LCH continues to present a challenge for the physician for the disease may progress at variable speed and the response
to treatment may be unpredictable. In patients presenting with only single system disease in the form of bone involvement, the disease rarely spreads to extraskeletal sites
.
and the patients fare extremely well. At the other extreme young
children with vital organ dysfunction do badly with high mortality. Identification of prognostic factors within the disease range of LCH is important with the changing concept of the disease from malignancy to an immunologic disorder
(7-9). In each patient treatment decision should be made taking into account the
likely natural history of the disease and we should weigh the possible benefits
of treatment against likely risk. It is no longer justifiable to treat all these
patients with potential carcinogens so that cytotoxic drugs are becoming reserved for poor prognostic cases. Many studies confirm that children under 2 years of age with organ dysfunction form the poorest prognostic group(5). The aim of treatment in these patients is to reduce mortality but there is no evidence that this goal is being achieved by more aggressive chemotherapy.
In this report we studied the disease outcome in children upto 2 years of age. There was no mortality in children without organ dysfunction even though multiple "Organs were involved in 6 patients. However, mortality was 100% in patients with organ dysfunction. Rivera Luna et
al. studied 55 childrenl:5elow the age of 2 years(10). Patients presenting without organ dysfunction had mortality of 31 % and with dysfunction in
"
one organ had a mortality of 46% while with initial dysfunction of 2 or more organs had a mortality of 92%. Greenberger et
al. studied 127 patients with LCH and divided them according to age and organ involvement (ll). In this study children less than 2 years with multiple organ involvement' had significantly greater mortality than the older, age group. Overall mortality was 36% in patients with
organ dysfunction in another series (12). Egeler et al. treated 8 infants
who ranged in age from birth to 9 months with life threatening organ dysfunction(13). The chemotherapy used was vincristine and steroids and cytosine arabinoside.
Five out of these 8 patients are long term survivors. But none of our patients
with organ dysfunction survived more than 6 weeks. In a recent Indian series of 22 cases of childhood histiocytosis over a 10 year period, the treatment outcome was not detailed and hence no comparison can be made(14). Also, the small size of most these studies and lack of agreement over staging system makes comparison between different studies difficult.
The presence of bone lesion in, an other- wise poor prognostic group is considered as a
favorable prognostic feature(l5). All the patients without organ dysfunction in
our series had bone involvement but it was seen in only one patient. with organ
dysfunction. All patients with organ dysfunction succumbed to disease and hence it is difficult to comment about the prognostic importance of bone disease in this group of children with organ dysfunction.
Dermal involvement alone in younger age has been considered as an unfavorable prognostic factor(16,17).
All the patients with organ dysfunction had skin involvement, while only 3 out of 11 evaluable patients
without organ dysfunction had skin involvement. These patients received chemotherapy.
Of these two patients developed recurrences and are alive without disease now.
All recent studies support the fact that there is a high correlation between.
initial response to treatment and outcome(18,19). Children who fail to achieve a
favorable response within 6 weeks of treatment are at high risk of progressive disease. In all our
children with organ dysfunction disease progression was rapid and all of them died within 4 weeks. Eleven of the thirteen children
without organ dysfunction are alive now. The median follow up of surviving patients is 62 months (range 34-161 mo). Three patients in this group have few sequelae like growth retardation, diabetes insipidus and dental abnormalities. No second malignancies have been reported in this group.
In conclusion, in all age groups, children with localized LCH have a good prognosis and they should not be exposed to unwarranted risk of chemotherapy. Patients with multi-system involvement may benefit from chemotherapy especially. when associated with systemic symptoms. All children with organ dysfunction require chemotherapy. Despite the use of intensive polychemotherapy
infants with organ dysfunction respond to treatment poorly. This is a patient group in which new treatment approach such as the use of cyclosporine has to be considered(20,21). The use of cyclosporine along with chemotherapy may be helpful in controlling the disease in these patients.
|
1.
Raney RB, D' Angio B. Langerhans cell histiocytosis: Experience at the Children's Hospital of Philadelphia 1970
- 1984. Med Pediatr Oncol 1989; 17: 20 - 28.
2.
Matus Ridley M, Rarey RB, Thawerani H, Meadows AT. Histiocytosis in children: Pat- tern of disease and results of treatment. Med Pediatr Oncol 1983; 11: 99-105.
3.
Ceci A, Terlizzi M, Colella R, Criuseppe L, Balducci D, Giammarco, et al. Langerhans cell histiocytosis in childhood: Results from the Italian Co-operative AIEOP - CNR Hx
83 study. Med Pediatr Oncol-1993; 21: 259-264.
4.
Kusuma Kumary P. Rajeev Kumar S, James FV, Chellam VG, Krishnan Nair M, Warrier RP. Langerhans cell histiocytosis in children:
Pattern of disease and treatment results in Kerala. Int J Pediatr Hematol Oncol 1996; 3: 297-303.
5.
Lahey ME. Histiocytosis: A analysis of prognostic factors. Pediatrics 1975: 87: 184-189.
6. Starling KA. Chemotherapy of histocytosis. Am J .Pediatr Hematol Oncol 1981; 3: 157- 160.
7.
Osband ME, Lipton JM, Lavin P, Levey R, Vawter G, Greenberger JS. Histocytosis X: Demonstration of abnormal immunity; T cell
histamin H2 receptor
-
deficiency and successful treatment with thymic extract. N Engl J. Med 1981; 304: 146-153.
8.
Nezeloff C. Histiocytosis X: A proliferative disorder of Langerhans cell system. Med Pediatr Oncol 1986; 1.4: 105-115.
9.
Willman CL, Busque L, Griffith BB, Blaise E,
et al. Langerhans cell histiocytosis
-
A clonal proliferative disease. A Engl
J Med. 1994; 331: 154-160.
10.
Rivera-Luna R, Alter Molchadsky N, Cardenas Cardes R, Martinez Guerra G. Langerhans cell histiocytosis in children under 2 years of age. Med Pediatr Oncol 1996;- 26: 334-343.
11.
Greenberger JS, Crocker AC, Vawter G, Jaffe N, Cassady JR. Results of treatment. of 127 patients with systemic histiocytosis 1989; 60: 311-338.
12.
McLelland J, Broadbent V, Yeomans E, Malone M, Pritchard J. Langerhans cell histiocytosis.
The case for conservative treatment. Arch Dis child. 1990; 65: 301-303.
13.
Egeler M, Jan de Kraker, Voute PA. Cytosine arabinoside, vincristine and prednisolone. in the treatment of children with disseniinated langerhans cell histiocytosis with organ dysfunction. Moo Pediatr Oncol 1993; 21: 265- 270.
14.
Goyal A, Rani S, Singh T, Choudhury P, Dubey AP. Childhood histiocytoses: A review of 22 cases. Indian Pediatr 1998; 35: 151- 156.
15.
Boradbent V, Favorable prognostic features in histiocytosis X: Bone involvement and absence of skin disease. Arch Dis Child 1986; 61: 1219-1221.
16.
Neuton W A, Hamoudi AB. A histologic classification with clinical correlation. In:
Perspectives in pediatric pathology, vol, 1. Eds. Rosenberg HS, Bolande RP. Chicago, Year Book Publishers, 1973; pp-25 1-283.
17.
Frederiksen P, Thommensen P: Histio-cytosis X-II. Histologic, appearance correlated to prognosis and extent of disease. Acta Radiol Oncol 1978; 17: 10-16.
18.
Gadner H, Heitger A, Grois N, Gatterer Menz I, Ladi,sch S for DALH X-83 study. Treatment strategy for disseminated Langerhans cell
histiocytosis. Med Pediatr Oncol 1994; 23: 72-80,
19.
Berry DH, Gresik MV, Humphrey GB, .star- ling K, Vietti T, Boyett S, et al.
Natural history of Histiocytosis X: A Pediatric Oncology Group Study. Med Pediatr Oncol 1986; 14: 1-5.
20.
Mahmoud HM, Wang we, Murphy, SB.. Cyclosporirie. therapy for advanced Langerhans cell histiocytosis. Blood 1991; 77: 721- 725.
21.
Arico M, Colella R, Canter V, Idolti P, Pession A. Cyclosporine therapy for refractony LCH. Med Pediatr Oncol 1995; 25: 12-16.
|
