Eosinophilic meningitis (EM) is a chronic aseptic meningitis often
caused by helminthic infestation. EM is defined as eosinophils>10 per
mm3 in CSF or >10% of total CSF leukocyte [1,2]. The most common
infectious cause of EM worldwide are Angiostrongylus cantonenis,
Gnathostoma spinigerum and Basyliascaris procyonis [1,2].
Non-infectious causes include malignancy like non Hodgkin lymphoma,
multiple sclerosis, hypereosinophilic syndromes, malfunctioning
ventriculo-peritoneal shunt and adverse drug reactions [2]. Even though
EM has been reported in adults and children from India, parasitic
etiology has not been confirmed in those cases [4]. We report a one year
old child, resident of South Kerala, India, who reported with prolonged
fever due to confirmed helminthic infestation.
A 1-year-old female child presented with 3 weeks
history of irregular fever, irritability and poor oral intake. Child was
started on oral cefixime from suspecting UTI. On admission, she had
continuous fever for 5 days with irritability and episodes of
inconsolable cry for 3 days. No history of vomiting or seizure, ear
infection, head trauma, recent vaccination or contact with Tuberculosis,
or exposure to any drugs or allergens. On examination, vitals were
stable with no features of raised intracranial pressure or signs of
meningeal irritation and with a normal CNS examination. On
investigation, white blood cell count was 14.8×109/L (36% neutrophils,
42% lymphocytes, 22% eosinophils) with peripheral smear showing
eosinophilia and no parasites or abnormal cells. C-reactive protein was
negative. Stool and urine examination did not reveal ova or cysts. In
view of non remission of prolonged fever and history of irritability and
headache, CSF study was done on second day of admission which revealed
increased CSF pressure of clear fluid with 1150 whole blood cells, (30%
neutrophils, 70% lymphocytes) with a protein 115 mg/dL and sugar 30 mg/dL
(blood sugar- 89 mg/dL) suggestive of meningitis. Cultures of blood, CSF
and urine were sterile. Tuberculosis PCR, CSF biofilm for bacterial and
viral panel were negative. India Ink and CSF biofilm were negative for
Cryptococcus, KOH wet mount did not reveal any fungal elements. Mantoux
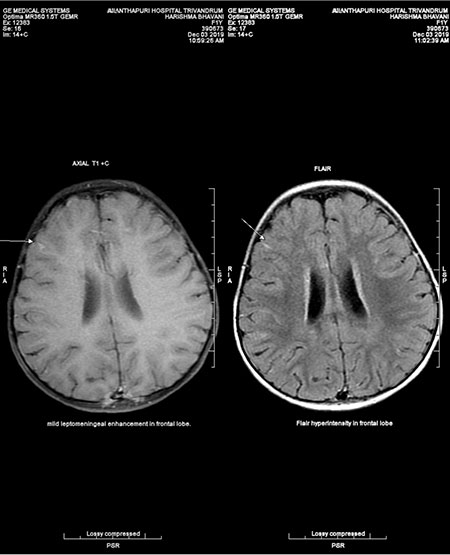
test and HIV ELISA were negative and Chest Roentgenogram was normal. MRI
contrast study of brain showed multiple cortical infarcts with sub
cortical and cortical hyper intensities in T2W/FLAIR, leptomeningeal
enhancement suggestive of meningitis. In view of meningitis, she was
initially treated with ceftriaxone, then upgraded to vancomycin,
meropenem and acyclovir. Since fever and irritability persisted even
after 7 days of antibiotics, repeat sepsis screen was done, which was
negative, and had similar findings on repeat MRI. Therefore, correlating
the peripheral eosinophilia with this history, EM was suspected. On
revisiting the history, mother gave history of a pet dog at home with
rat and snail infestation in the locality. Absolute eosinophil count was
3080/mm3 on day 1, 5500/mm3 on day 7, 2880/mm3 on day12, 3102/mm3 on day
17. Repeat CSF study revealed 295 white blood cell/mm3 (5% neutrophils,
85% lymphocytes, 25% eosinophils) with protein 104 mg/dL, sugar 34 mg/dL
(blood sugar-103mg/dL). Real Time PCR was done in CSF, which came
positive A. cantonenis. She was started on prednisolone 2
mg/kg/day along with Albendazole 15 mg/kg/day for 2 weeks. Within 48
hours of treatment she became afebrile, her sensorium improved with
improvement in activity and appetite. After 2 weeks of hospital stay she
was discharged in a stable condition with an absolute eosinophil count
of 625/mm3 on day 20.
Peripheral eosinophilia is an immunologically
mediated response to various conditions like allergic (atopy,
medications), neoplasms (leukemia, lymphoma, tumor associated) drug
induced hypersensitivity and infectious diseases (parasite, fungal). It
is essential to look for non infectious causes of hyper-eosinophilia
symptoms, before looking for parasitic infection.
 |
|
Fig.1 T1W/FLAIR images showing
leptomeningeal enchancement/hyperintensity in frontal lobe.
|
Overall parasitic meningitis is rare, but exact
incidence and prevalence is not reported. Among the three major
helminthes that cause EM [1,2], A.cantonensis is the most common.
Neurocysticrcosis, although rare, also is known to cause EM in endemic
areas.
Similar infections have been described in Southeast
Asia, South Pacific, Taiwan, Africa, Caribbean, Australia and North
America [1]. Shipboard travel of rats is the most common cause for the
spread of parasite to other continents as rats are the definitive host.
[2,3] and human beings are the accidental hosts. Infection occurs due to
ingestion of third stage larvae in raw or undercooked snails or fish and
children who play in the dirt in endemic areas are prone for infection.
Eosinophilic meningitis is diagnosed presumptively based on travel or
exposure history with CSF analysis showing >10% eosinophils, mildly
elevated protein and normal glucose or hypoglycorrhachia [5]. Peripheral
eosinophilia peaks about 5 weeks after exposure. MRI brain demonstrates
high signal intensities, leptomeningeal enhancement, hyper intense
signals on T2W image. For detection of parasite in CSF, ELISA is
sensitive and specific but is limited by commercial non availability and
cross reactivity between helminthic parasites. PCR based studies are
sensitive in detecting the parasite DNA.
Treatment is mainly supportive with analgesics,
corticosteroids and anthelminthic drugs [6,2]. There is higher incidence
of neurological sequelae among children and prognosis is good with 70%
improvement within 1-2 weeks and mortality is <1%.
This case is presented to sensitize the clinician,
the rarity of EM, caused by helminthic infection. The possibility of
eosinophilic meningitis/parasitic meningitis must be considered in a
patient with fever, peripheral eosinophilia, headache with or without
meningeal signs. In such patients, CSF eosinophil staining is
recommended along with demonstration of parasite antigen through real
time PCR will help to establish parasitic etiology and also in
prognostication and appropriate follow up.
Acknowledgement: Prof Arun Kumar, Director,
Manipal Institute of Virology, Manipal Academy of Higher Education,
Manipal for CSF PCR confirmation of A.cantonensis.
1. Weller, Liu L. Eosinophilic meningitis. Semin
Neurol. 1993; 13:161-8.
2. Parameswaran K. Case series of eosinophilic
meningoencephalitis from South India. Ann Indian Acad Neurol.
2006;9:217.
3. Hochberg NS, Blackburn BG, Park SY, et al.
Eosinophilic meningitis attributable to Angiostrongylus cantonensis
infection in Hawaii: Clinical characteristics and potential exposures.
Am J Trop Med Hyg. 2011;85:685-90.
4. Chotmongkol V, Wongjitrat C, Sawadpanit K, et al.
Treatment of eosinophilic meningitis with a combination of albendazole
and corticosteroid. Southeast Asian J Trop Med Public Health.
2004;35:172-4.
5. Jitpimolmard S, Sawanyawisuth K, Morakote N, et al. Albendazole
therapy for eosinophilic meningitis caused by Angiostrongylus
cantonensis. Parasitol Res. 2007;100: 1293-6.

