|
|
|
Indian Pediatr 2021;58: 184 -186 |
 |
Hepatic Visceral Larva Migrans Causing
Hepatic Artery Pseudo-Aneurysm
|
|
Ritu,1 Kumble S Madhusudhan2 and
Rohan Malik3*
Departments of 1Pediatrics, 2Radiodiagnosis,
and 3Hepatology and Clinical Nutrition,
All India Institute of Medical Sciences, New Delhi, India.
Email:
[email protected]
|
|
Visceral Larva Migrans refers to migration of second
stage nematode larvae through human viscera most commonly the liver and
lungs. This entity usually presents with fever, abdominal pain,
hepatomegaly and respiratory symptoms. Here we describe hepatic visceral
larva migrans causing hepatic artery pseudoaneurysm and presenting with
upper gastro-intestinal bleeding and its management.
Parasitic infections of liver are commonly
encountered in clinical practice and can have myriad presentations
posing a clinical diagnostic challenge. Hepatic visceral larva migrans
(VLM) is one such entity presenting with prolonged fever and liver
involvement especially in areas endemic for the parasite. Hepatic artery
pseudoaneurysm is a complication described mostly with traumatic liver
injury and post-surgery [1]. We describe this complication secondary to
hepatic VLM and its successful management.
A 12-year-old girl presented with high grade fever,
jaundice and right upper abdominal pain with progressive abdominal
distension associated with weight loss for four months and a history of
recurrent black tarry stools requiring blood transfusions. She was
resident of a rural area and her family of seven lived in an overcrowded
house, belonged to lower socioeconomic status with poor hygiene
practices, consumed vegetarian diet and had exposure to pet animals in
neighborhood. On examination she was underweight (BMI 12.5 kg/m2),
febrile and tachypneic, had severe pallor with pedal edema and no skin
lesions. Systemic examination revealed firm tender hepatomegaly (liver
span:17 cm) without ascites or splenomegaly and crepitations on right
side of chest. Ophthalmoscopic examination was unremarkable.
Investi-gations revealed anemia (hemoglobin 5.7g/dL), and leukocytosis
(16×103/L) with eosinophilia (1.4×103/L). Liver function tests were
alanine aminotransferase 23 U/L, aspartate aminotransferase 19 U/L,
alkaline phosphatase 590 U/L, total bilirubin 1.5 mg/dL with direct
fraction 1.2 mg/dL, serum albumin 1.9 g/dL with albumin:globulin ratio
of 0.4. As the child was sick at arrival, she was started on broad
spectrum antimicrobials and supportive treatment (blood transfusion and
albumin). Ultrasonography showed hepatomegaly with diffuse hypoechoic
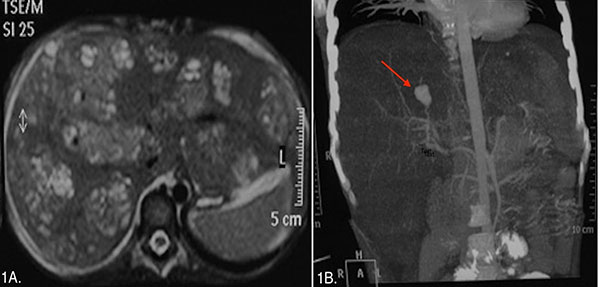
cystic lesions in both lobes of the liver. MRI abdomen showed lesions in
the liver appearing hypointense on T1-weighted and hyperintense on
T2-weighted images (Fig.1a) with mildly dilated common bile duct
and normal intrahepatic biliary radicles. Dual phase CT scan of abdomen
revealed multiple discrete and confluent hypodense lesions in both lobes
of liver along with a 1.5 cm pseudoaneurysm (arrow) arising from the
posterior branch of the right hepatic artery (Fig.1b). Based on
clinical and radiological findings, a differential diagnosis of visceral
larva migrans, cat scratch disease, Fascioliasis, disseminated
tuberculosis and invasive candi-diasis with underlying immunodeficiency
along with pseudo-aneurysm with suspected hemobilia was kept. The
patient underwent digital subtraction angiography (DSA) and successful
embolization of the pseudoaneurysm with n-butyl cyanoacrylate glue.
Subsequent investigations revealed normal stool examination and negative
Toxocara IgG serology, Echinococcus IgG serology, procalcitonin, Mantoux
test, gastric aspirate genexpert for Tuberculosis, and HIV serology.
Bacterial and fungal blood culture was sterile and upper GI endoscopy
was normal. Percutaneous liver biopsy demons-trated ill-defined
eosinophilic granulomas suggesting parasitic infiltration. Special
stains and tissue culture was negative for acid fast bacilli (AFB),
Bartonella and fungal elements. Based on clinical, radiological and
histopathological findings, diagnosis of visceral larva migrans was made
and child was started on albendazole (10mg/kg/day), diethylcarbamazine
(4mg/kg/day) and oral steroids (1mg/kg/day) in 3 cycles of 3 weeks each
with gradual tapering of steroids over next one month. Follow up imaging
at six months showed resolution of hepatic lesions.
 |
|
Fig. 1 (a) Axial T2 weighted MR image
shows multiple conglomerate heterogeneous lesions in both lobes
of liver, (b) Coronal CT angiography image shows a
pseudoaneurysm (arrow) arising from the posterior branch of
right hepatic artery.
|
Visceral larva migrans (VLM) refers to migration of
second stage nematode larvae through human viscera most commonly liver
and lungs. The etiological agents include Toxocaracanis, Toxocaracati,
Baylisascarisprocyonis, Cappilaria hepatica, and Ascarissuum
[2]. Humans are accidental hosts and acquire infection by ingestion of
food contaminated with infective eggs. The clinical manifestations are
fever, hepatomegaly, weight loss and respiratory symptoms mimicking
asthma. An IgG ELISA based on 30 kDa recombinant Toxocara excretory–secretory
antigen has 92% sensitivity and 89% specificity [3]. Features suggestive
of VLM on CT are presence of multiple confluent peripheral and
periportal ill-defined hypodense, oval or elon-gated nodular lesions
scattered throughout liver parenchyma with peripheral rim enhancement
and MRI shows T2 hyperintense/T1 hypointense lesions with restriction on
diffusion weighted sequences [4]. Confirmation is by histo-pathological
examination which shows presence of eosino-philic granuloma, palisading
histiocytes and very rarely larva may be visualized. The slow migration
of larva through the tissue incites a host inflammatory response along
with eosinophilic infiltration and destruction of liver parenchyma. The
cytotoxic eosinophil derived proteins may damage the endothelium causing
vascular complications [5]. Hepatic artery pseudoaneurysm, a rare
complication has not been previously described with VLM. Pseudoaneurysm
develops due to the erosion of the eosinophilic abscesses into the
hepatic artery. Rupture of the aneurysm results in hemobilia and the
patients may present with hematemesis or melena or both. In cases of
rupture of the aneurysm, early intervention by angio-embolisation of
feeding artery should be considered. The embolizing agents used include
coils, n-butyl cyanoacrylate glue and thrombin [1]. Medical therapy
includes diethyl-carbamazine, mebendazole or albendazole for 2-3 weeks.
Steroids are indicated in cases of ocular and neurological toxo-cariasis
and in acute inflammatory manifestations of VLM [6].
We conclude that hepatic VLM can be a rare cause of
hepatic artery pseudoaneurysm resulting in upper gastro-intestinal
bleeding. Early recognition and comprehensive management is of utmost
importance.
REFERENCES
1. Nagaraja R, Govindasamy M, Varma V,et al. Hepatic
artery pseudoaneurysms: A single-center experience. Ann Vasc Surg.
2013;27:743-9.
2. Beaver PC, Snyder CH, Carrera GM, Dent JH,
Lafferty JW. Chronic eosinophilia due to visceral larva migrans: Report
of three cases. Pediatrics. 1952;9:7-19.
3. Norhaida A, Suharni M, LizaSharmini AT, Tuda J,
Rahmah N. rTES-30USM: Cloning via assembly PCR, expression, and
evaluation of usefulness in the detection of toxocariasis.Ann Trop Med
Parasitol. 2008;102:151-60.
4. Laroia ST, Rastogi A, Bihari C, Bhadoria AS, Sarin
SK. Hepatic visceral larva migrans, a resilient entity on imaging:
Experience from a tertiary liver center. Trop Parasitol. 2016;6:56-68.
5. Young JD, Peterson CG, Venge P, Cohn ZA.
Mechanisms of membrane damage mediated by human eosinophilic cationic
protein. Nature. 1986;321:613-6.
6. Magnaval JF, Glickman LT. Management and treatment options for
human toxocariasis. In: Holland CV, Smith HV, editors. Toxocara:
The Enigmatic Parasite. CABI Publishing; 2006.p.113-26.
|
|
|
 |
|

