|
|
|
Indian Pediatr 2021;58:
182-183 |
 |
Introduction of Proton Beam Therapy in
Intracranial Germ Cell Tumors in India
|
|
Rishan Thimma Sudarsan,1 Srinivas Chilukuri,1
Noufal Manthala Padannayil,2
Pankaj Kumar Panda3 and Rakesh Jalali1*
From Departments of 1Radiation Oncology,
2Medical Physics, and 3Clinical Research,
Neuro-Oncology Cancer Management Team, Apollo Proton Cancer Centre,
Taramani,
Chennai, Tamil Nadu, India.
Email:
[email protected]
|
|
Intracranial germ cell tumors (ICGCT) represent rare
tumors comprising 1-2% of brain tumors and <3% of all neoplasms in
children [1]. Optimal management of ICGCT involves multimodal therapy
including surgery, radiotherapy (RT) and systemic chemotherapy [2].
Proton beam therapy (PT) has unique features of delivering sharp
fall-off of RT dose resulting in significant sparing of normal tissues
compared to traditional photon therapy. We describe our initial
experience in treatment of these tumors using image-guided intensity
modulated proton therapy (IMPT) at our center, the first and only PT
facility in South Asia.
An 18-year-old male presented with history of
decreased appetite, weight loss, and generalized weakness for six
months. Magnetic resonance imaging (MRI) of brain showed lesions in
periventricular region and subsequent stereotactic biopsy was suggestive
of intracranial germinoma with CD117 and Oct4 positivity. Cerebrospinal
fluid (CSF) analysis revealed increased beta human chorionic
gonadotrophin ( b-HCG)
and normal alpha fetoprotein (AFP) with no malignant cells. He received
four cycles of etoposide and carboplatin according to ACNS0232 protocol
[2], following which, his tumor markers normalized and he was
subsequently treated with IMPT to a total dose of 40 GyE in 23 fractions
(23.8GyE in 14 fractions craniospinal irradiation (CSI) and 16.2 GyE in
9 fractions boost to gross residual and pre chemotherapy volumes) [3].
He tolerated PT well and subsequent MRIs done 6 weeks, 6 months and 14
months post-PT did not show any residual disease. His tumor markers and
endocrine values were within normal limits with his height relatively
stable as he has already achieved his growth spurt. He has resumed his
socio-academic activities and is on regular follow-up for the past 20
months.
A 16-year-old boy presented with sudden onset
diplopia since five months. MRI showed well defined lobulated mass
lesion measuring 2.4×2.1×3.1 cm in the region of third ventricle. Tumor
marker analysis showed elevated serum â-HCG (1626 mIU/mL) and AFP (2.0
ng/mL). CSF analysis reported increased
b-HCG measuring 3589
mIU/mL and AFP measuring 0.47 ng/mL. A diagnosis of NGGCT (choriocar-cinoma)
was made and he subsequently received four cycles of ifosfamide,
cyclophosphamide and carboplatin (ICE), followed by IMPT to a total dose
of 54 GyE in 30 fractions (CSI 30.6 GyE in 17 fractions followed by
boost of 23.4 GyE in 13 fractions) [3]. Follow-up MRI post-PT after 2
month and 18 months showed interval decrease in residual disease.
Post-PT tumor markers were normal and endocrine functions optimal, with
the patient’s height relatively stable. He has been on regular follow-up
since past 20 months and has been continuing his normal socio-academic
activities.
 |
|
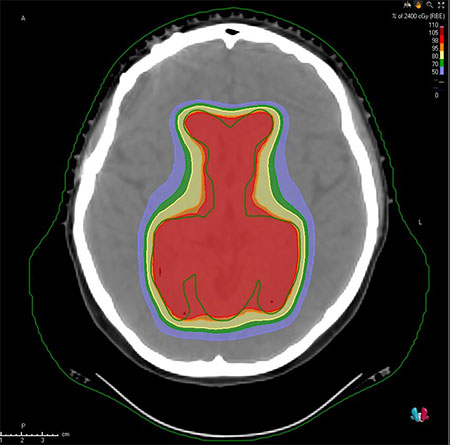
Fig. 1 Dose distribution of whole
ventricular radiotherapy using Intensity modulated proton
therapy.
|
A 15-year-old female with amenorrhea, presented with
increased thirst, micturition, weight loss, and blurring of vision
towards left side over a period of two years. Visual perimetry showed
bilateral temporal hemianopia. MRI brain with spine screening revealed a
2.1×2.3×2.3 cm suprasellar lesion compressing the optic chiasm. She
underwent a right pterional craniotomy and gross total resection of
lesion, reported as intracranial germinoma. Her tumor markers (serum and
CSF) showed mild elevation of b-HCG
(2.8 mIU/mL). She was on thyroid, cortisol and desmopressin supplements
post-surgery because of decreased endocrine functions. Her
neurocognitive evaluation before proton therapy showed her in the high
average range. She received four cycles of three weekly etoposide and
carboplatin followed by IMPT (Fig.1) to a total dose of 40 GyE in
25 fractions (24 GyE in 15 fractions to whole ventricular volume and 16
GyE in 10 fractions to tumor bed) [4]. Post-PT tumor markers were within
normal limits. Follow up MRI after one, six and twelve months did not
show any residual disease. Post proton therapy, her endocrine function
did not deteriorate and she was continued on hormone supplements.
Subsequent ophthalmic evaluation showed no visual deficits. The patient
has been on regular follow up for the past 15 months and has resumed her
normal academic activities.
For all these patients, cases were discussed in
multi-disciplinary tumor boards. Patients, after customized
immobilization, underwent a planning CT and MRI. Dedicated PT plans were
generated for each case using Monte-Carlo optimization and 3-4 PT fields
[3]. Treatments were delivered on a daily basis (5 fractions a week)
after carefully laid out quality assurance checks as per institutional
protocols. Significant reduction of the radiation dose to critical
structures such as hippocampi and cochlea were observed.
RT is an integral part of treatment of ICGCT but can
be associated with considerable late effects including neurocognitive
disturbances and risk of secondary cancers, and chemotherapy alone is
insufficient due to high rates of local and metastatic recurrence.
Current standard of care is ventricular radiotherapy in case of
localized and CSI in case of disseminated germinomas [4,5]. In
comparison with conventional radiotherapy, PT due to its unique physical
and biological characteristics results in delivering low entry dose and
deposit the majority of their energy at the end of their path, yielding
a typical dose energy peak called ‘Bragg peak.’ This steep fall-off
allows for the delivery of high radiation doses to the tumor and sparing
of tissue beyond the tumor. All our patients underwent PT as a part of
curative management and tolerated the treatment well. One patient
treated with CSI had grade III neutropenia managed conservatively,
whereas others did not experience more than grade II toxicities. Mean
dose to hippocampus for all our patients was less than 30 Gy, below the
accepted threshold for intelligence quotient preservation [6]. All
patients could resume their normal schooling after the treatment, with
no impact so far in their educational activities, and maintained quality
of life. However, neurocognitive assessments were not available for two
out of the three patients, and could not be planned due to the logistic
challenges because of the ongoing COVID-19 pandemic.
We have successfully implemented PT in the treatment
of ICGCT in India. PT should be considered as a treatment option for
optimal management of these curable tumors. Further follow up is
required to assess the long-term sequelae of treatment in these
patients.
REFERENCES
1. Kakkar A, Biswas A, Kalyani N, et al. Intracranial
germ cell tumors: A multi-institutional experience from three tertiary
care centers in India. Childs Nerv Syst. 2016;32:2173-80.
2. Calaminus G, Kortmann R, Worch J, et al. SIOP CNS
GCT 96: Final report of outcome of a prospective, multinational
nonrandomized trial for children and adults with intracranial germinoma,
comparing craniospinal irradiation alone with chemotherapy followed by
focal primary site irradiation for patients with localized disease.
Neuro Oncol. 2013;15:788-96.
3. Tonse R, Chilikuri S, Shamurailatpam D, Jalali R.
Introduction of image-guided pencil beam for skull base tumors in India:
A report of two cases and a brief review of the literature. Neurol
India. 2020;68:42.
4. MacDonald SM, Trofimov A, Safai S, et al. Proton
radiotherapy for pediatric central nervous system germ cell tumors:
Early clinical outcomes. Int J Radiat Oncol Biol Phys. 2011;79:121-9.
5. Rogers S, Mosleh-Shirazi M, Saran F. Radiotherapy
of localised intracranial germinoma: Time to sever historical ties?
Lancet Oncol. 2005;6:509-19.
6. Goda JS, Dutta D, Krishna U, et al. Hippocampal
radiotherapy dose constraints for predicting long-term neurocognitive
outcomes: Mature data from a prospective trial in young patients with
brain tumors. Neuro Oncol. 2020;;22:1677-85.
|
|
|
 |
|

