|
|
|
Indian Pediatr 2019;56: 114-118 |
 |
Skilled Counseling in Enhancing Early and
Exclusive Breastfeeding Rates: An Experimental Study in an Urban
Population in India
|
|
Arun Gupta 1,
JP Dadhich1, S
Manazir Ali2 and
Neelima Thakur1
From 1Breastfeeding Promotion Network of India,
Delhi, and 2Department of Pediatrics, Jawaharlal Nehru Medical College,
AMU, Aligarh, Uttar Pradesh; India.
Correspondence to: Dr JP Dadhich,National
Coordinator, Breastfeeding Promotion Network of India (BPNI), Delhi,
India.
Email: [email protected]
Received: December 21, 2017;
Initial review: May 07, 2018;
Accepted: November 20, 2018.
|
|
Objectives: The study was
conducted to evaluate the effect of breastfeeding counseling and
breastfeeding support by trained counselors during the ante-natal period
at health facility and post-natal period at home on breastfeeding
practices during the first six months of life.
Design: This was a randomized
controlled study that compared the effect of counseling on breastfeeding
during the first 6 months of life.
Setting: study was done in a
government medical college in northern India, which is situated in an
urban area.
Participants: 300 healthy
pregnant women from an urban population attending the antenatal clinic
at Jawaharlal Nehru Medical College, Aligarh Muslim University were
recruited for the study.
Intervention: Subjects were
equally assigned randomly to the intervention (2 antenatal and 8
postpartum home counseling visits by the counselors) and control
(non-counseling) group.
Main Outcome Measures: Infant
feeding practices including rates of initiation of the breastfeeding
within one hour of birth; exclusive breastfeeding and bottle-feeding
during the first 6 months of life.
Results: Initiation of
breastfeeding within one hour of birth was 73.4% in intervention group
as compared to 33.6% in control group (P=0.001). More mothers in the
intervention group (88.1%) were able to sustain exclusive breastfeeding
rates at 6 months of age in comparison to the control group (50%) (OR
7.44, 95% CI 3.98-13.92).
Conclusions: This study
substantiates positive role of skilled counseling by a trained dedicated
breastfeeding counselor during the antenatal and post-natal periods on
breastfeeding practices during the first six months of life.
Keywords: Breastfeeding, Infant feeding,
Pregnancy.
|
|
B
reastfeeding practices like initiation of
breastfeeding within one hour of birth and exclusive breastfeeding for
the first six months of life have immense public health importance.
However, status of breastfeeding practices is far from satisfactory in
India where rate of initiation of breastfeeding within one hour of birth
is 41.6% while exclusive breastfeeding rate is about 55% [1].
Breastfeeding counseling helps in building mother’s
confidence, improving feeding technique, and preventing or resolving
breastfeeding problems. Several studies and a Cochrane review have
reported positive impact of breastfeeding counseling both at hospital
and at community in increasing rates of initiation of breastfeeding
within one hour of birth as well as duration of exclusive breastfeeding
[2,3]. Limited information is available on this subject from India. We
conducted this study to evaluate the effect of breastfeeding counseling
and breastfeeding support by trained counselors during the ante-natal
period at health facility and post-natal period at home on breastfeeding
practices during the first six months of life.
Methods
It was a randomized control study that compared the
effect of counseling on feeding practices during the first six months of
life. The study was conducted between March 2016 and December
2016 in the Obstetrics and Pediatrics services in the Jawaharlal Nehru
Medical College, Aligarh Muslim University, Uttar Pradesh, India.
The proportion of Exclusive Breastfeeding at 6 months
in India and Uttar Pradesh is 46.3% and 51.3% respectively according to
the NFHS-3 data. Expecting the proportion of EBF as 50% in the
non-counseled group at six months and expecting the proportion of EBF as
70% in the counseled group at six months with 90% power and 5% level of
significance, a sample of 124 subjects per group was required with 1: 1
ratio. After adding 15% as lost to follow-up, the number increased to
146 per group. Thus 300 subjects were planned to be included. The
Institutional Ethics Committee of Jawaharlal Nehru Medical College,
Aligarh Muslim University approved the study.
Women were recruited from antenatal clinic if they
met the following criteria: 18 years or more of age, gestational age of
18-22 weeks, singleton pregnancy, considering breastfeeding to feed her
newborn, planning to deliver in the same hospital, willing to stay in
Aligarh for at least 6 months after delivery. Informed consent was
obtained from the subjects recruited in the study. At the time of the
recruitment, data on their socio-economic and socio demographic status,
basic knowledge on breastfeeding practices, her telephone number and
house address were obtained in a structured questionnaire. Data of the
recruited subjects were entered into the database at the end of every
week. Exclusion criteria included mother having any medical complication
during the pregnancy or delivery; preterm delivery and neonate having
any medical complication. For randomization, the list of eligible women
was shared weekly with a statistician who assigned the subjects to
intervention and control group using the simple randomization process
with SPSS software. List of those women who were assigned to the
intervention group was given to the counselors every week. Within one to
two week of enrolment the counselor contacted the women and gave the
first antenatal counseling. This procedure was repeated every week till
300 eligible subjects were enrolled.
Two nutritionists were recruited to provide
counseling to the mothers in the intervention group. They received
training from the Breastfeeding Promotion Network of India (BPNI)
training team on infant and young child feeding counseling using the 7
days training programme titled "Infant and Young Child Feeding
Counseling: A Training course" [4]. Mothers assigned to the counseling
group (Intervention group) were offered 2 antenatal visits in hospital
and 8 postpartum home visits by the counselors. This was in addition to
the routine antenatal, intra-partum and postnatal obstetric care at the
health facility. Counselors conducted first antenatal counseling between
the first and second week after enrolment of mothers. Second antenatal
counseling was scheduled before 36 weeks of pregnancy. Pregnant women
were educated about the benefits of exclusive breastfeeding up to the
age of six months and dangers of artificial feeding and bottle-feeding.
Demonstrations were done for correct positioning and attachment,
expression of breastmilk and cup feeding technique. Women were
encouraged to clarify their myths and doubts. They were counseled to
initiate breastfeeding within one hour of birth and avoid pre-lacteal
feeds. Post-delivery, mothers received routine support for breastfeeding
at maternity ward by the regular maternity staff. Once the mothers in
the intervention group were discharged, 8 postpartum home visits for
counseling were scheduled as follows: at 3 rd,
7th, 15th
day and 2nd,
3rd, 4th,
5th and
6th
months after birth. During each follow-up visit, mothers and family
members were counseled for practicing exclusive breastfeeding, answers
to any specific queries were provided and skilled support was provided
to address any specific breastfeeding problems such as engorgement, sore
nipple, mastitis etc. The duration of each visit was about 20-30
minutes. Mothers in the control group were provided with the routine
prenatal care advice like diet in pregnancy, delivery related
precautions, breastfeeding, and care of newborn that are usually offered
to women in the hospital by the health professionals. They did not
receive any counseling by dedicated breastfeeding counselor during
ante-natal and post-partum period.
Two research assistants were recruited exclusively to
conduct antenatal and postnatal interviews with mothers for collecting
data on infant feeding practices and to take anthropometric measurements
of the infants (weight and height) every month in both the groups. They
were trained to administer pre-structured and pre-tested questionnaires
a day after delivery (before discharge from the hospital) and at
maternity ward to both groups. Detailed information about the antenatal
and postnatal experience, like initiation of breastfeeding, pre-lacteal
feeding, and infant feeding practices. Subsequently at each home visit,
data was collected on infant feeding practices using the 24 hours recall
method as defined by the World Health Organization (WHO) [5].
All the activities in the study, namely, enrollment
of subjects, recruitment of counselors, training of counselors,
scheduling of counseling of mothers, scheduling of data collection
interviews were supervised by the team of investigators in the JLN
Medical college, Aligarh and BPNI secretariat. Data were processed using
the SPSS software (version 16, Chicago IL). Socio demographic factors
and women characteristics between 2 groups at baseline were compared
using the t-test and Chi-square
analysis. Comparison between groups regarding initiation
of the breastfeeding was determined using the Chi-square test. Odd ratio
and its 95% CI were calculated for exclusive breastfeeding and
bottle-feeding at different age. Chi-square test was used to determine
the significance. Detailed information about the anthropometric data
will be reported in a separate communication.
Results
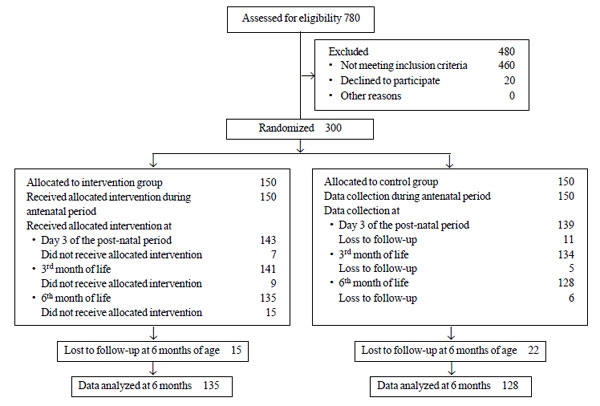
Of the 780 pregnant women screened in the antenatal
clinic, 300 eligible women were enrolled for the study. Fig. 1
provides the study flow details.
 |
|
Fig. 1 Flowchart of the participants.
|
Table I provides the baseline comparison
between the groups. The subjects were similar in two study groups. The
rates of initiation of breastfeeding within one hour of birth was
significantly higher in the intervention group (73.4%) as compared to
the control group (33.6%). (P<.001) Similar were the results when
stratified by mode of delivery (89.2% in intervention vs 55.4% in
control group amongst normal deliveries and 34.1% vs 9.1% in cesarian
deliveries).
TABLE I Baseline Socio-demographic Characteristics of Participants
|
Intervention |
Control group |
|
group (n=150) |
(n=150) |
|
Mother’s education |
|
Illiterate
|
26 (17.3) |
33 (22.0)
|
|
Primary |
16 (10.7) |
21 (14.0) |
|
Middle and intermediate school |
58 (38.7) |
54 (36.0) |
|
Graduate and higher
|
50 (33.3) |
42 (28.0) |
|
Occupation |
|
Home maker |
145 (96.7) |
146 (97.3) |
|
Working outside home |
5 (3.3) |
4 (2.7) |
|
Caste |
|
Scheduled caste |
2 (1.3) |
2 (1.3) |
|
Scheduled tribe |
1 (0.7) |
0 (0.0) |
|
Other backward class |
60 (40.0) |
76 (50.7) |
|
General |
87 (58.0) |
72 (48.0) |
|
Religion |
|
Muslim |
139 (92.7) |
134 (89.3) |
|
Hindu |
10 (6.7) |
16 (10.7) |
|
Sikh |
1 (0.7) |
0 |
|
Nuclear family
|
36 (24.0) |
27 (18.0) |
|
Place of Residence
|
|
Rural
|
7 (4.7) |
5 (3.3) |
|
Slum |
26 (19.3) |
46 (30.7) |
|
Urban |
114 (76.0) |
99 (66.0) |
|
Correct knowledge about infant feeding |
|
Initiation of breastfeeding |
57 (38.0) |
72 (48.0) |
|
Exclusive breastfeeding |
93 (62.0) |
90 (60.0) |
|
No statistically significant differences between the groups. |
The rates of exclusive breastfeeding at various ages
in both the groups are depicted in the Table II.
The exclusive breastfeeding rate remained significantly high throughout
the study period in the intervention group while in the control group;
it decreased sharply after 3 rd
month. More mothers in the intervention group were able to exclusive
breastfeeding at 6 months of age in comparison to the control group. At
the age of six months, mothers in the intervention group (8.4%) were
less likely to practice bottle-feeding than the mothers in the control
group (22.9%). (Odd Ratio=0.29; 95% CI, 0.13 -0.62).
TABLE II Rates of Exclusive Breastfeeding and Bottle-feeding in the Partcipants (3rd Day – 6 Months)
|
Age of the infant |
Feeding Practice |
Intervention Group (n=150) |
Control Group (n=150) |
Odds Ratio (95% CI) |
|
3rd day |
Exclusive breastfeeding (%) |
141/143 (98.6) |
119/139 (85.6) |
11.85 (2.71- 51.73) |
|
Bottle-feeding (%) |
2/143 (1.4) |
3/139 (2.2) |
0.64 (0.10-3.90) |
|
3 month |
Exclusive breastfeeding (%) |
135/141 (95.7) |
100/134 (74.6) |
7.65 (3.09 to 18.92) |
|
Bottle-feeding (%) |
4/141 (2.8) |
30/134 (22.4) |
0.10 (0.04 to 0.30) |
|
6 months |
Exclusive breastfeeding (%) |
119/135 (88.1) |
64/128 (50.0) |
7.44 (3.98 to 13.92) |
|
Bottle-feeding (%) |
10/135 (8.4) |
28/128 (22.9) |
0.29 (0.13 to 0.62) |
Discussion
In the present study, mothers who received
breastfeeding counseling and skilled support during the antenatal and
postnatal period by a trained and dedicated counselor in the
intervention group could achieve significantly higher rate of early
initiation of breastfeeding and exclusive breastfeeding.
A randomized control trial from Bangladesh, which
looked into peer counselors support to the pregnant and lactating women
during antenatal and postnatal period showed significantly better early
breastfeeding initiation rates and higher prevalence of exclusive
breastfeeding at 5 months for the intervention group [6]. A systematic
review on interventions to improve breastfeeding outcomes has reported
that providing breastfeeding counseling in combination settings of
health systems, home and family and the community environment results in
improved breastfeeding practices [7]. A study from China found antenatal
and postnatal breastfeeding support program efficacious and beneficial
to mothers in increasing the exclusive breastfeeding duration [8].
Similar results were reported in studies from Turkey and Pakistan in
which antenatal breastfeeding education and postnatal support led to
high rates of early initiation of breastfeeding resulted in longer
exclusive breastfeeding duration [9,10]. A systematic review has
reported beneficial role of dedicated lactation specialists and
lactation counselors to provide breastfeeding education and support to
pregnant and lactating women [11]. Similarly, a study from India on the
effect of peer counseling by mother support groups has reported enhanced
breastfeeding rates with provision of breastfeeding counseling [12].
Mother’s Absolute Affection (MAA) program [13] of Ministry of Health and
Family Welfare, Government of India recognizes counseling as a vital
intervention to enhance breastfeeding practices. This study
provides evidence that counseling by a trained, dedicated breastfeeding
counselor during the ante-natal and post-natal period helps in achieving
high rates of initiation of breastfeeding within one hour of birth and
sustaining exclusive breastfeeding at 6 months of age. To establish the
counseling services, allocation of resources and appointment of
dedicated counselors in public hospitals and maternity facilities are
needed. Government of India should also encourage the private health
care facilities to appoint the counselors.
Acknowledgements: Prof Seema Hakim, Prof Tamkin
Rabbani, and Dr Anjali Rani, from Jawaharlal Nehru Medical College, AMU
Aligarh; Dr. Shoba Suri, Ms. Nupur Bidla, Ms. Vibharika Chandola and Ms
Veena Rawat from BPNI for their contributions in conducting the study
and Dr Rajeev Kumar, statistician from AIIMS, New Delhi for his support
in analyzing the data.
Contributors: All the authors contributed in the
conceptualization and designing of the study, supervision of the
progress of the study, analysis and interpretation of data, drafting of
the manuscript. All the authors approved the final draft.
Funding: The study was part of an international
project for breastfeeding protection, promotion and support with
financial grant by Swedish Agency for International Development Agency
(SIDA). Funds for emoluments of the counselors and the data collection
team etc. were provided through this project.
Competing Interest: Three of the authors
(AG, JPD, NT) work with the Breastfeeding Promotion Network of India
(BPNI), one of the organization that conducted this study. BPNI works
for protection, promotion and support of breastfeeding.
|
What is Already Known?
•
For practicing optimal
breastfeeding, mothers need access to skilled practical help and
counseling support from trained health workers and counselors
What this Study Adds?
• Providing ante-natal and post-natal
counseling support to mothers by a dedicated breastfeeding
counselor can significantly enhance rates of early initiation
and helps mothers to sustain exclusive breastfeeding in hospital
born infants.
|
References
1. National Health and Family Survey - 4, 2015-16:
India Fact Sheet. Ministry of Health and Family Welfare, Government of
India. Available from: http://rchiips.org/NFHS/pdf/NFHS4/India.pdf.
Accessed December 17, 2017.
2. Leite AJ, Puccini RF, Atalah AN, Alves Da Cunha
AL, Machado MT. Effectiveness of home-based peer counselling to promote
breastfeeding in the northeast of Brazil: a randomized clinical trial.
Acta Paediatr. 2005;94:741-6.
3. Britton C, McCormick FM, Renfrew MJ, Wade A, King
SE. Support for breastfeeding mothers. Cochrane Database Syst Rev.
2007;24:CD001141.
4. The "4 in 1" Training Programme - Capacity
building initiative for building health/nutrition workers’ skills in
Infant and Young Child Feeding Counseling. Breastfeeding Promotion
Network of India (BPNI), International Baby Food Action Network (IBFAN)
Asia; Delhi, 2015. Available from:
http://bpni.org/Training/4-in-1-brochure.pdf. Accessed December 17,
2017.
5. World Health Organization. Indicators for
assessing infant and young child feeding practices: part 1: definitions:
conclusions of a consensus meeting held 6-8 November 2007 in Washington
DC, USA. Available from: http://apps.who.int/iris/bitstream/10665/43895/1/97892415966
64_eng.pdf. Accessed August 25, 2017.
6. Haider R, Ashworth A, Kabir I, Huttly SR. Effect
of community-based peer counsellors on exclusive breastfeeding practices
in Dhaka, Bangladesh: A randomised controlled trial. Lancet.
2000;356:1643-7.
7. Sinha B, Chowdhury R, Sankar MJ, Martines J,
Taneja S, Mazumder S, et al. Interventions to improve
breastfeeding outcomes: A systematic review and meta-analysis. Acta
Paediatr. 2015;104:114-34.
8. Liu L, Zhu J, Yang J, Wu M, Ye B. The effect of a
perinatal breastfeeding support Program on Breastfeeding Outcomes in
Primiparous Mothers. Western journal of nursing research.
2017;39:906-23.
9. Vural F, Vural B. The effect of prenatal and
postnatal education on exclusive breastfeeding rates. Minerva Pediatr.
2017;69:22-9.
10. Ahmad MO, Sughra U, Kalsoom U, Imran M, Hadi U.
Effect of antenatal counselling on exclusive breastfeeding. J Ayub
Medical College Abbottabad. 2012;24:116-9.
11. Patel S, Patel S. The effectiveness of lactation
consultants and lactation counselors on breastfeeding outcomes. J Human
Lactation. 2016;32:530-41.
12. Kushwaha KP, Sankar J, Sankar MJ, Gupta A,
Dadhich JP, Gupta YP, et al. Effect of peer counselling by mother
support groups on infant and young child feeding practices: The Lalitpur
experience. PLoS One. 2014;9:e109181.
13. MAA program for promotion of breastfeeding.
Operational guidelines. Ministry of Health and Family Welfare,
Government of India, 2016. Available from:
http://nhm.gov.in/MAA/Operational_Guidelines.pdf. Accessed December
17, 2017.
|
|
|
 |
|

