|
|
|
Indian Pediatr 2019;56: 109-113 |
 |
Aquagenic Wrinkling of Skin: A Screening Test
for Cystic Fibrosis
|
|
Anuj Singh 1,
Rakesh Lodha1, Shivaram
Shastri1, G Sethuraman2,
KN Sreedevi1,
Madhulika Kabra1 and SK
Kabra1
From Departments of 1Pediatrics and 2Dermatology, All
India Institute of Medical Sciences, New Delhi, India.
Correspondence: Dr SK Kabra, Professor, Department of
Pediatrics, All India Institute of Medical Sciences,
New Delhi 110 029, India.
Email: [email protected]
Received: February 02, 2018;
Initial review: May 19, 2018;
Accepted: December 18, 2018.
|
|
Objectives: To study the utility
of aquagenic wrinkling as screening test for children with cystic
fibrosis.
Design: Evaluation of diagnostic
test.
Setting: Pediatric Chest Clinic,
and Pediatric Wards of a tertiary care hospital in New Delhi.
Participants: Three groups
(children with cystic fibrosis, carriers of cystic fibrosis, and
controls).
Method: Time taken to develop
aquagenic wrinkling was measured. The test was performed by asking the
enrolled subject to put their one hand in water and was checked for
development of wrinkling every minute, and a photograph was also taken
every minute.
Results: A total of 64 children
with cystic fibrosis, 64 controls and 64 carriers were enrolled in the
study. Median (IQR) time to develop aquagenic wrinkling in the three
groups was 2 (1.5,3) minutes, 4 (3,5) minutes and 8 (5,11) minutes,
respectively. The optimal cut-off was calculated as 3 minutes by
Receiver operating characteristic curve with a sensitivity and
specificity for identification of children with cystic fibrosis as 81%
and 57%, respectively. The area under curve was 76.5%. The 3 minute
cut-off for development of aquagenic wrinkling was applied to 54
children referred for sweat test. 20 children had sweat chloride values
of ³60
mEq/l and diagnosed as cystic fibrosis. 15 of these developed aquagenic
wrinkling at £3
minutes, giving a sensitivity of 75%.
Conclusion: In places with no
facility for sweat test, children with phenotype compatible with cystic
fibrosis who develop aquagenic wrinkling in 3 minutes may be diagnosed
as probable cystic fibrosis and referred for confirmation by sweat test.
Keywords: Diagnosis, Sensitivity, Specificity,
Sweat test.
|
|
C
ystic fibrosis (CF) is the one of the common
life-limiting genetic disorders in Caucasians with an incidence of
approximately 1 in 2500 children born in the United Kingdom [1].
Previously considered to be rare, recent reports suggest that CF occurs
in India and diagnosis is missed [2,3]. The precise incidence of CF
among Indian subcontinent is not known. The incidence in migrant Indian
populations in the USA has been estimated to be 1 in 40000 [4], same in
UK has been estimated between 1 in 10000 to 1 in 12000 [5,6]. A study on
955 cord blood samples reported carrier rate of common mutation
c.1521_1523delCTT (also known as DF508) as 0.4% [7]. By using same data
the incidence of CF in India is estimated as 1 in 40000 live births.
The prevalence of genetic mutations differs among
population subgroups. The commonest mutation is DF508, which is reported
between 19 to 44% Indian children [8].
In view of multiple mutations associated with CF, use
of genetic mutation testing as diagnostic test for CF is not feasible.
With a population of over one billion in India, diagnostic facilities
for CF are available in less than ten centers in the country. Even if a
clinician suspects CF in a child, he/she is not able to confirm the
diagnosis as the patient may have to travel hundreds of kilometers to
get the sweat test done. Therefore, diagnosis of CF is not confirmed or
gets delayed. It is important to identify children with CF early and
administer appropriate treatment.
It has been documented in some studies that children
with CF may develop aquagenic wrinkling more rapidly as compared to
controls, and has been reported to be a sensitive test for screening
children with CF [9-12]; however, it has not been studied in detail.
Therefore, we planned the present study to calculate sensitivity and
specificity of this simple test as screening test for children with CF.
In this study our primary objective was to document
the prevalence of aquagenic wrinkling of skin in patients with cystic
fibrosis. Secondary objective was to identify optimal time for aquagenic
wrinkling for cases and carriers, study utility of aquagenic wrinkling
of skin as screening test for cystic fibrosis and to determine
genotype-phenotype correlation for aquagenic wrinkling in children with
cystic fibrosis.
Methods
Study design was descriptive study for evaluation of
diagnostic test, and conducted at Pediatric Chest Clinic and Pediatric
Wards at a tertiary-care center in Northern India. The study was
conducted from July 2014 to March 2016 for a total duration of 21
months. There were three groups of participants as cases, control and
carriers. Cases were children with cystic fibrosis age >12 months
diagnosed with clinical phenotype and sweat chloride >60 mEq/L on two
occasions. Carriers were biological mother or father of children with
CF. Controls were children without respiratory symptoms attending the
pediatrics outpatient department. Exclusion criteria were participants
who received aminoglycoside antibiotics in past one month, or those
having other dermatological condition affecting palms.
For calculating sample size, it had been documented
that aquagenic wrinkling is observed in >53-84% of children with CF in
<5 minutes. We presumed the prevalence as 65% and precision of 12%,
sample size calculated to be as 64 children with cystic fibrosis.
Children referred for sweat chloride during study period were also
enrolled for validating the study results.
Eligible participants were enrolled in the study
after informed consent. Details for each patient including demographic
profile, mutation analysis for cystic fibrosis, and sweat chloride
result were recorded. Examination of both hands was done and images were
taken (16-megapixel camera) to compare the result prior to immersion in
water. RO (Reverse osmosis filter) purified water was used at
temperature (25-30 oC) in
clean standard size tray and kept on level surface. The study
participant was asked to immerse one hand in water and time noted as
zero. Hands were examined for 3 seconds after every minute to look for
wrinkling till 5 minutes and photographed till wrinkling appears on
finger tips or palm (Fig. 1). If wrinkling did not
appear till 5 minutes, hands were examined every minute and photographs
were taken at appearance of wrinkling. Those who did not develop
wrinkling by 15 minute were assigned a wrinkling time of 15 minute and
photograph taken at 15 minute time. At appearance of wrinkling (by
comparing with other hand outside water), time was recorded and
photograph was taken. Carriers and controls were examined in a similar
fashion.
 |
| (a) |
(b) |
(c) |
|
Fig. 1 showing hands at (a) start and
(b) at 1 minute of immersion of left hand in RO water in
standard tray. Figure 1(c) shows (aquagenic wrinkling of left
palm and taken as end point by observer) at end of 2 minutes of
immersion in the same child.
|
Outcome variables were defined as aquagenic wrinkling
i.e. wrinkling of skin on immersion of hand in water that is
taken as end point as assessed by observer. Time to aquagenic wrinkling
was defined as time from immersion of hand in water to the development
of wrinkling of skin of hand by comparing with other hand. Study
protocol was approved by institutional Ethics Committee. Participants
were enrolled after obtaining a written informed consent from
participants/parents or guardians of children.
Statistical analysis: Data were managed using
Microsoft Excel and analyzed using Stata 11.0 software. The prevalence
of aquagenic wrinkling in CF was the proportion of children positive for
aquagenic wrinkling in 5 minutes. The prevalence was compared with that
in carriers and controls. Sensitivity and specificity of aquagenic
wrinkling at different time intervals was calculated using sweat test as
diagnostic gold standard for CF. Mean and median time for development of
wrinkling was calculated. Mean time for wrinkling in CF children with
positive DF508 and negative for DF508 were compared. For determination
of optimal cut off time, Receiver operator characteristic curve (ROC)
was drawn.
Results
A total of 64 children with cystic fibrosis, 64
controls without clinical symptoms of cystic fibrosis, 64 parents of
children with CF were enrolled over a period of 21 months. The median
(IQR) age for cystic fibrosis cases was 9 (5-13.7) years; 43 (67.2%)
were boys and 21 (32.8%) were girls. Median (IQR) age of controls is 6.5
(5- 8) years; 44 (68.7%) boys. The median (IQR) age of 64 carriers
(biological parents of children with cystic fibrosis) was 36 (33-40)
years; 30 (46.8%) were males. Fifty-four children, referred for sweat
chloride test, were also enrolled; their median (IQR) age was 6 (4-10)
years (70.4% boys).
All the 64 enrolled children with CF developed
aquagenic wrinkling within 8 minutes. Sixty-one children developed
aquagenic wrinkling by 5 minutes, giving a prevalence of aquagenic
wrinkling by 5 minutes as 95.3% (95% confidence interval of 90.1- 100%).
The prevalence in carriers and controls using the 5-min cut-off was
29.7% and 82.8%, respectively (P value for comparison of
prevalence in the 3 groups <0.0001). Median time (IQR) for wrinkling in
children with CF was 2 (1.5- 3) min while same in controls was 4 min
(3-5) and in carriers was 8 min (5-11), respectively. The difference was
statistically significant suggesting that it can discriminate between
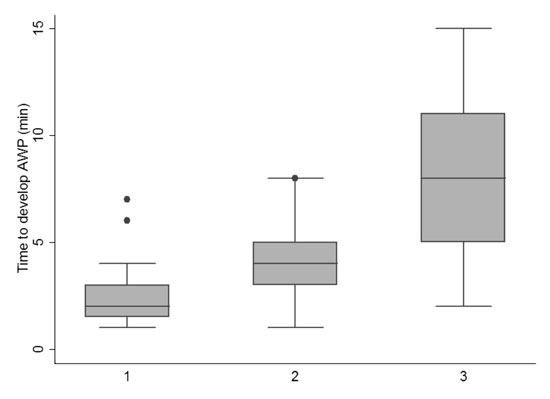
different groups (P=0.0001) (Fig. 2).
 |
|
Fig. 2 Time to develop aquagenic
wrinkling in children with cystic fibrosis, controls and
carriers of cystic fibrosis gene mutation.
|
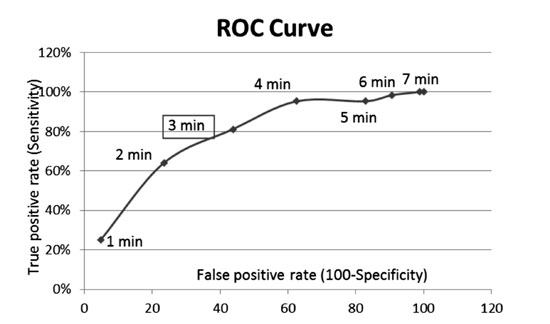
Sensitivity and specificity of aquagenic wrinkling
were calculated by using different cut-off time in cases and controls.
Sensitivity for identification of children with CF if they developed
wrinkling at one minute was 25% and increased to 100% at 8 minutes.
Similarly, specificity at cut-off of one minute was 95% but decreased
progressively and was 5% at 8 minutes. Receiver operator (ROC) curve for
different cut-offs of time to aquagenic wrinkling was drawn and it
suggested an optimal cut-off at 3 minutes with a sensitivity of 81.2%
and specificity of 56.2% (Fig. 3). The area under curve
was 0.76.
 |
|
Fig. 3 Receiver Operating
Characteristic curve for time to develop aquagenic wrinkling of
palms as a screening test for cystic fibrosis.
|
Time to develop aquagenic wrinkling was checked in 54
children referred for sweat chloride test. A total of 20 children had a
sweat chloride value of ³60
mEq/L. Of these 20 children, 15 developed aquagenic wrinkling by 3
minutes. Considering sweat chloride value of
³60 mEq/L for
diagnosis of CF, sensitivity of aquagenic wrinkling of palms by 3 minute
was 75%. A total of 13 (20%) children were positive for DF508 and 51
(80%) were negative for mutation. Median (IQR) time of wrinkling in
DF508 mutation positive cases was 2 (1- 2) min and in mutation negative
cases was 2 (2- 3) min (P=0.04). In each age subgroup (less than
and more than 6 year age), cases developed aquagenic wrinkling of palm
at statistically significant less time as compared to control group. For
cases there is trend towards aquagenic wrinkling at less time in
subgroup £6
year of age (Table I).
TABLE I Aquagenic Wrinkling of Palms in Children with Cystic Fibrosis and Controls
|
Age category |
Median (IQR) time to develop aquagenic wrinkling of
palms; min |
|
n |
Cases |
n |
Controls |
|
Age £6 y |
23 |
2 (1- 3) |
32 |
4 (2.5- 5) |
|
Age > 6 y |
41 |
2 (2- 3) |
32 |
4 (3- 5) |
|
P<0.01 for comparison between cases and controls for both
age-groups; For comparison between the two age-groups, P=0.43
for cases and P=0.45 for controls. |
Discussion
In this diagnostic test evaluation study, we found
that the prevalence of aquagenic wrinkling in children with CF was 95%.
We observed that the median time to develop aquagenic wrinkling in
children with cystic fibrosis is significantly less as compared to
controls (children without CF) and in carriers (parents of CF).
Aquagenic wrinkling by 3 minutes had a reasonable sensitivity and
specificity for identification of children with cystic fibrosis of 81%
and 56%, respectively. Children with CF having DF508 mutation had lower
time to aquagenic wrinkling as compared with those negative for DF508
mutation.
Our study had some limitations. The cut-off to define
wrinkling of skin was based on observer decision. However, the observer
had been trained and supervised; photographs were also taken. In carrier
population mutation analysis is not available for all and we assumed
parents of CF children as heterozygous for mutation. There is also
possibility that the control group may have carriers as we have not done
mutation analysis in control group to rule out the same.
Aquagenic wrinkling in CF was first reported in 1974
[13]. After this observation, there were only few case reports until
2004 when Katz, et al. [14] reported DF508 homozygous cases
presenting with aquagenic wrinkling. Berk, et al. [9] did a
blinded comparison of 44 CF cases and 26 controls for aquagenic
wrinkling of palm by using tap water and 3 minute as cut-off time and
gave aquagenic wrinkling score to each participant from score 0 to score
4, and found that mean score was significantly higher in CF cases than
in control group. In our study the maximum sensitivity was at 3 minute,
although we did not use any aquagenic wrinkling score which might be a
more reproducible parameter, but we identified wrinkling at predefined
time points after immersion. Gild, et al. [10] did a case control
study and enrolled 21 patients, 13 carriers and 15 controls and patients
with a time to wrinkling of £3
min were defined as having aquagenic wrinkling. Mean time to wrinkling
was 2 min in cases, 7 min in carriers and 11 min in controls which was
comparable to our study. All carriers in our study were not having
genetic diagnosis and we enrolled parents of CF cases as carriers, their
median time for wrinkling of skin is also comparable. CF carrier having
higher time to aquagenic wrinkling can be explained by heterozygous
state and normal chloride conductance, in contrast to CF patients. Also
median age of carrier population is significantly higher than cases and
control which can affect detection of wrinkling in this group. Arkin,
et al. [11] in a prospective observation trial found higher
prevalence of aquagenic wrinkling of the palms in CF cases as compared
to controls with no genotype phenotype correlation. In our study we
found that children with CF having DF508 mutation had lower time to
aquagenic wrinkling as compared with those negative for DF508 mutation.
The variation in aquagenic wrinkling time with mutation analysis may be
due to possible role of chloride conductance channel role in wrinkling
of skin, but as exact pathophysiologic mechanism of aquagenic skin
wrinkling is not known so there may be role of other cell volume
regulation mechanisms [15]. Chinazzo, et al. [12] did cross
sectional study in 2014 on 58 children with CF and 23 carriers and seven
controls and found that aquagenic wrinkling of palm is more common in CF
cases as compared to carrier. No correlation was found between CF
genotype and AWP score severity. Garcon, et al. [16] did a cross
sectional study to determine the frequency of aquagenic palmoplantar
keratoderma in 27 CF cases for 2-3 minute in water and found that 41%
developed wrinkling of skin. In our study, we had a higher percentage of
81% CF cases developing wrinkling within 3 minutes of hand immersion.
Results are different possibly due to shorter time of immersion as
compared to our study.
None of the previous studies have evaluated the
utility of aquagenic wrinkling of skin as a screening test. In current
study, we could document a sensitivity of 75% in children referred for
sweat test. Data also suggested that there is a trend towards earlier
wrinkling of skin in younger children with cystic fibrosis. This can be
possibly attributed to characteristics of skin in younger children which
helps in early identification of wrinkling by observer.
Based on observations in our study aquagenic
wrinkling of skin by 3 minutes can be used a screening test and can help
for early identification of patients and their referral for diagnostic
investigations. In India, where diagnostic facilities for cystic
fibrosis is available at few centers, aquagenic wrinkling of skin can be
used as a clinically useful screening test. Strengths of our study
include enrolment of cases, controls and carriers. We tried to perform
test using water with similar electrolyte content (RO water),
temperature and compared development of wrinkling with other hand that
was not immersed in water. We also took photographs every minute to
ensure quality control.
We conclude that children with cystic fibrosis
develop aquagenic wrinkling faster than the healthy subjects. Aquagenic
wrinkling has a potential to be a simple, inexpensive method to use as
screening test for identification of children with CF and especially, in
resource limited situation, it may help in early referral and diagnosis,
which could translate to decreased morbidity of CF patients.
Contributors: AS: developed protocol, collected
data, analysis of data and writing of manuscript; RL: involved in
development of protocol, analysis of data and manuscript writing; SS:
involved in study development, genetic studies and manuscript writing;
GS: involved in development of protocol, monitoring and manuscript
writing; KNS: involved in data collection; MK: involved in protocol
development, genetic studies and manuscript writing; SKK: involved in
protocol development, analysis and manuscript writing. He will act as
guarantor for the study.
Funding: None; Competing Interest: None
stated.
|
What is Already Known?
•
Children with cystic fibrosis
may develop aquagenic wrinkling faster than normal children.
What This Study Adds?
•
Aquagenic wrinkling can be used as a potential screening
test for cystic fibrosis in children.
|
References
1. Dodge JA, Morison S, Lewis PA, Coles EC, Geddes D,
Russell G, et al, UK Cystic Fibrosis Survey Management Committee.
Incidence, population, and survival of cystic fibrosis in the UK,
1968-95. Arch Dis Child. 1997;77:493-6.
2. Ahuja AS, Kabra SK. Cystic fibrosis: Indian
experience. Indian Pediatr. 2002;39:813-8.
3. Kabra SK, Kabra M, Lodha R, Shastri S. Cystic
fibrosis in India. Pediatr Pulmonol. 2007;42:1087-94.
4. Powers CA, Potter EM, Wessel HU, Lloyd-Still JD.
Cystic fibrosis in Asian Indians. Arch Pediatr Adolesc Med.
1996;150:554-5.
5. Goodchild MC, Insley J, Rushton DI, Gaze H. Cystic
fibrosis in 3 Pakistani children. Arch Dis Child. 1974;49:739-41.
6. Spencer DA, Venkataraman M, Higgins S, Stevenson
K, Weller PH. Cystic fibrosis in children from ethnic minorities in the
West Midlands. Respir Med. 1994;88:671-5.
7. Kapoor V, Shastri SS, Kabra M, Kabra SK,
Ramachandran V, Arora S, et al. Carrier frequency of F508 del
mutation of cystic fibrosis in Indian population. J Cyst Fibros Off J
Eur Cyst Fibros Soc. 2006;5:43-6.
8. Kabra M, Kabra SK, Ghosh M, Khanna A, Arora S,
Menon PS, et al. Is the spectrum of mutations in Indian patients
with cystic fibrosis different? Am J Med Genet. 2000; 93:161-3.
9. Berk DR, Ciliberto HM, Sweet SC, Ferkol TW,
Bayliss SJ. Aquagenic wrinkling of the palms in cystic fibrosis:
Comparison with controls and genotype-phenotype correlations. Arch
Dermatol. 2009;145:1296-9.
10. Gild R, Clay Cd, Morey S. Aquagenic wrinkling of
the palms in cystic fibrosis and the cystic fibrosis carrier state: a
case–control study. Br J Dermatol. 2010;163:1082-4.
11. Arkin LM, Flory JH, Shin DB, Gelfand JM, Treat
JR, Allen J, et al. High prevalence of aquagenic wrinkling of the
palms in patients with cystic fibrosis and association with measurable
increases in transepidermal water loss. Pediatr Dermatol. 2012;29:560-6.
12. Chinazzo C, Alessandri AD, Menoni S, Romanisio G,
Rebora A, Rongioletti F. Aquagenic wrinkling of the palms and cystic
fibrosis: An Italian study with controls and genotype-phenotype
correlations. Dermatology. 2014; 228:60-5.
13. Elliott RB. Wrinkling of skin in cystic fibrosis.
Lancet. 1974;2:108.
14. Katz KA, Yan AC, Turner ML. Aquagenic wrinkling
of the palms in patients with cystic fibrosis homozygous for the delta
F508 CFTR mutation. Arch Dermatol. 2005;141: 621-4.
15. Arniges M, Vázquez E, Fernández-Fernández JM,
Valverde MA. Swelling-activated Ca2+ entry via TRPV4 channel is
defective in cystic fibrosis airway epithelia. J Biol Chem.
2004;279:54062-8.
16. Garçon-Michel N, Roguedas-Contios A-M, Rault G,
Le Bihan J, Ramel S, Revert K, et al. Frequency of aquagenic
palmoplantar keratoderma in cystic fibrosis: a new sign of cystic
fibrosis? Br J Dermatol. 2010;163:162-6.
|
|
|
 |
|

