|
|
|
Indian Pediatr 2018;55: 161-162 |
 |
Multiple Pulmonary
Nodules in an Immunocompetent Adolescent with Infectious
Mononucleosis
|
|
Praveena Nediyara Bhaskaran 1,
Mammen Puliyel2,
Melissa Myers3
and Nazha Abughali4
From Departments of 1Pediatrics, 2Pediatric
Hematology, 3Radiology and 4Pediatric
Infectious Disease, MetroHealth Medical Center, Cleveland, OH 44109,
USA.
Correspondence to: Dr Praveena Nediyara Bhaskaran,
Department of Pediatrics, MetroHealth Medical Center, Cleveland,
OH-44109, USA.
Email:
[email protected]
Received: October 30, 2016;
Initial review: March 20, 2017;
Accepted: November 23, 2017.
|
Background: Infectious mononucleosis is usually a self-limiting
illness, but can be rarely associated with complications. Case
characteristics: A 17-year-old boy with Epstein-Barr virus related
infectious mononucleosis and cold antibody-mediated autoimmune hemolytic
anemia with incidentally noted multiple pulmonary nodules.
Observations: Nodules regressed over the next few weeks without
specific therapy. Message: Pediatricians need to be aware of this
rare clinical presentation of infectious mononucleosis so that further
invasive testing can be avoided.
Keywords: Computed tomography, Epstein Barr virus, Lung
nodules.
|
|
E
pstein Barr Virus (EBV) infection is usually a
self-limiting disease. The age of the patient has a profound influence
on the clinical manifestations. In infants and young children, it is
either asymptomatic or accompanied by mild, nonspecific symptoms. In
contrast, approximately 50% of adolescents and young adults present as
infectious mononucleosis (IM) [1].
Case Report
A 17-year-old previously healthy boy initially
presented to the local pediatrician’s office with complaints of fever,
malaise, bodyache and decreased appetite of 14 days’ duration and
headache, sore throat and neck pain of 10 days’ duration. His girlfriend
was diagnosed with infectious mononucleosis a few weeks ago. Physical
examination revealed pharyngeal erythema, a grade 3+ tonsillar
enlargement bilaterally with purulent exudates and bilateral anterior
and posterior non tender cervical lymphadenopathy. Laboratory
investigations revealed hemoglobin (Hb) 150 g/L, white blood cell (WBC)
count 5.1 X 10 9/L with 18%
lymphocytes which included 16% of atypical lymphocytes, 33% Neutrophils
and 19% band cells. Monospot test was positive. Rapid streptococcal test
of the throat swab was negative. Patient was given a dose of intravenous
dexamethasone 5 mg for sympto-matic relief and was sent home on 2 days
of oral steroids.
On day 18 of illness, the patient presented to our
emergency department with multiple episodes of syncope, vomiting, poor
oral intake and fever. He was found to be febrile and hypotensive and
had a weight loss of 7% (79.3 kg to 73.9 kg). There was no history of
bleeding from any site. Investigations revealed hemoglobin 80 g/L,
reticulocyte 6.3%, absolute reticulocyte count 210×10 9/L,
LDH 281 U/L and elevated liver enzymes. Total bilirubin and haptoglobin
were normal, and urine hemosiderin was negative. Computed Tomography
scan (CT) of abdomen and pelvis did not show any evidence of splenic
rupture or hemoperitoneum, but showed moderate hepatospleno-megaly and
retroperitoneal lymph node enlargement with the largest one measuring
2.5×2.2 cm. It also revealed multiple pulmonary nodules in the
visualized lower lobes with the largest measuring 9×11 mm. CT chest
showed about 15-20 pulmonary nodules involving all lobes. The nodules
were solid and well circumscribed with spiculated margins.
 |
|
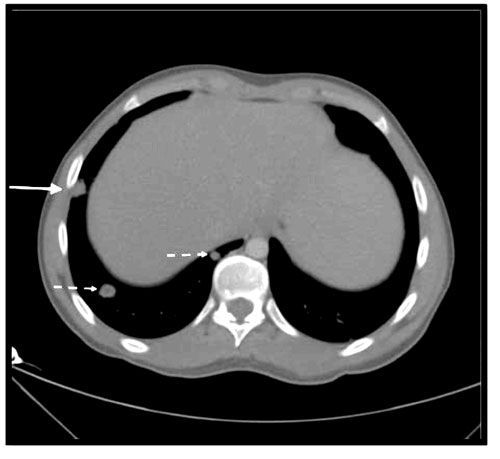
Fig. 1 Axial image through the lung
bases showing the multiple pulmonary nodules (broken arrow). The
largest one in this image (solid arrow) measures 13.5 × 1.7 mm.
|
Direct antiglobulin test was positive for complement
and negative for IgG. Cold agglutinins were negative and Donath
Landsteiner antibody was negative. The patient received one unit of
packed red cell transfusion with an inline warmer. Respiratory viral
panel as well as other infectious disease work up for Human
Immunodeficiency Virus (HIV), Cytomegalovirus (CMV), Parvovirus and
Mycoplasma were negative. Epstein Barr virus Viral Capsid Antigen
(EBV-VCA) IgM was positive suggestive of an acute EBV infection. The
anemia was attributed to cold antibody related hemolytic anemia due to
EBV infection.
Patient was followed up weekly for the next six
weeks. After six weeks, his hemoglobin was 111 g/L. He was asymptomatic
at the visit and had regained his weight. Low dose follow-up CT chest
two months after the initial presentation showed resolution of most of
the nodules.
Discussion
Infectious mononucleosis can sometimes cause
multi-systemic involvement including hematologic manifestations, splenic
rupture, hepatic involvement and rarely renal, cardiac and pulmonary
manifestations. The pulmonary involvement previously reported involved
either interstitial or parenchymal pneumonia. In immunosuppressed
patients, EBV can also cause lymphoproliferative disorder (PTLD) or
lymphoma, which can present as multiple pulmonary nodules [1]. Pulmonary
nodules occurring in immunocompetent children as part of EBV is rarely
reported in literature. Pelliccia, et al. [2] described a
14-year-old girl with EBV positive IMN with multiple pulmonary nodules
as well as mild pericardial effusion and hydrops of gall bladder, all of
which resolved on follow up . Shinozuka, et al. [3] described a
case of multiple lung nodules in an adolescent with IMN which
spontaneously regressed over a two year period.
There has been an increased incidence of detection of
pulmonary nodules in children due to widespread use of CT scans.
Currently there are no evidence based guidelines for the management of
pulmonary nodules in children. Metastatic disease is much more likely to
be a cause of a malignant nodule in a child than is a primary lung
tumor. The characteristics most likely to be associated with malignancy
include nodules with sharp borders, presence of a solid mass with a
hilic pattern of growth, or a mixed solid- cystic or completely cystic
mass. Fat, popcorn calcification, uniform calcification, peripheral
location, elongated lesion, pleural tag and stability compared with
prior studies are all associated with benign lesions. [4]
Pulmonary nodules could be part of the clinical
presentation of infectious mononucleosis in otherwise healthy children
and in an appropriate setting, a close follow-up with complete
resolution is adequate to rule out malignancy. Our patient was managed
conservatively with close monitoring and regular follow-up. The decision
on follow up imaging should be individualized based on clinical signs
and symptoms and imaging characteristics.
Contributors: PNB: drafted the manuscript; MP:
contributions to the conception and design of the work and diagnosis of
the disease; MM and NA: Revised the work critically for important
intellectual content.
Funding: None; Competing interests: None
stated.
References
1. Allen C, Rooney CM, Gottschalk S. Infectious
Mononucleosis and other Epstein-Barr Virus–associated Diseases. In:
Hoffman R, Benz EJ, Silberstein LE, Heslop HE, Weitz JI, Anastasi J,
editors. Hematology: Basic Principles and Practice. 6th ed.
Philadelphia: Elsevier Inc. 2013. p. 708-20.
2. Pelliccia P, Savino A, Cecamore C, Di Marzio D,
Chiarelli F, Primavera A, et al. Imaging spectrum of
EBV-infection in a young patient. J Ultrasound. 2008;11:82-4.
3. Shinozuka J, Awaguni H, Tanaka SI, Makino S,
Maruyama R, Inaba T, et al. Spontaneous regression of pulmonary
nodules presenting as epstein-barr virus-related atypical infectious
mononucleosis. J Pediatr Hematol Oncol. 2016;38:e162-5.
4. Brody AS, Mahani MG, Guillerman RP, Hegde SV,
Iyer RS, Lee EY, et al. The incidental pulmonary nodule in a
child. Part 1: Recommendations from the SPR thoracic imaging committee
regarding characterization, signi-ficance and follow-up. Pediatr Radiol.
2015;45:628-33.
|
|
|
 |
|

