|
|
|
Indian Pediatr 2016;53: 159 -161 |
 |
Acquired Toxoplasmosis Presenting with a
Brainstem Granuloma in an Immunocompetent Adolescent
|
|
Nitin Manwani, K Ravikumar, #V
Viswanathan, *Santosh Mohan
Rao and ‡Anita Mahadevan
From the Departments of Pediatric Intensive Care, #Pediatric
Neurology, *Pediatric Neurosurgery, Kanchi Kamakoti CHILDS Trust
Hospital and CHILDS Trust Medical Research Foundation (CTMRF), Chennai;
and ‡Department of Neuropathology, National Institute of Mental Health
and Neuro Sciences (NIMHANS), Bangalore, India.
Correspondence to: Dr Nitin Manwani, Department of Pediatric
Intensive Care, Kanchi Kamakoti CHILDS Trust Hospital, 12A, Nageswara
Road, Nungambakkam, Chennai 600 034, India.
Email: [email protected]
Received: June 22, 2015;
Initial review: August 20, 2015;
Accepted: December 05, 2015.
|
|
Background: Toxoplasmosis is an
uncommon disease in immunocompetent people. Case characteristics:
We report an adolescent boy with central nervous system toxoplasmosis
who presented with progressive lower cranial nerve palsies and a
ring-enhancing lesion on neuroimaging. Intervention: Diagnosis of
toxoplasmosis was confirmed on histopathology of the excised lesion.
Message: Toxoplasmosis should be considered in the differential
diagnosis of focal brain lesions irrespective of immune status.
Keywords: Immuno-deficiency, Ring-enhancing
lesion, TORCH infection.
|
|
S
ymptomatic toxoplasmosis is uncommon in
immunocompetent children. Presentation is generally with localized or
generalized lymphadenopathy [1], and CNS involvement is extremely rare.
We report an adolescent boy who presented with lower cranial nerve
palsies, and MRI brain showed a heterogeneously enhancing mass lesion in
the brain stem, which on histopathological evaluation was suggestive of
toxoplasmosis.
Case Report
A 14-year-old boy, who was previously well and
developmentally normal with normal nutritional status and no past
history of any chronic illness or any medication use was referred to our
hospital with a 10-day history of difficulty in closing the right eye,
deviation of angle of the mouth to the left, drooling of saliva, nasal
regurgitation of feeds, nasal twang to voice and an unsteady wide-based
gait. There was no history of convulsions or altered sensorium. There
was no history of any preceding febrile illness. On examination, he was
hemodynamically stable and conscious with GCS of 15. There was upper
motor neuron palsy of the right facial nerve, with involvement of the IX
and X cranial nerves. Rest of the neurologic examination was normal. No
adenopathy or hepatosplenomegaly was noticed.
Blood counts, Erythrocyte sedimentation rate (ESR),
liver and renal functions were normal. Mantoux test was negative and
there were no Acid Fast Bacilli seen on Ziehl Neelsen stain of gastric
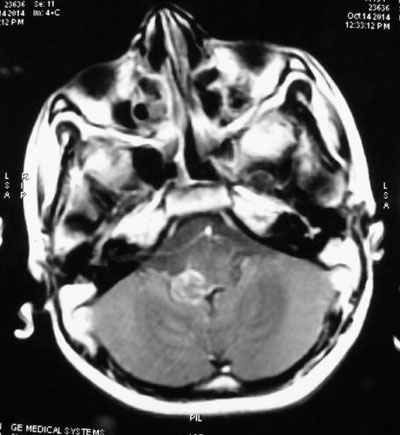
aspirate. MRI brain showed a hypo-intense lesion in the pons extending
into the medulla. The lesion was heterogeneously enhancing with contrast
with vague ring-enhancement dorsally (Fig. 1). The
possibility of a tuberculoma was considered. CSF analysis was within
normal limits. GeneXpert MTB/RIF (Nucleic Acid Amplification Test) in
CSF was negative. He had progressively increasing difficulty in
swallowing, absent gag reflex and also developed right hemiparesis. Due
to this inability to maintain his airway, he was intubated and
subsequently tracheostomy was done. In view of progression of
neurological deficits and lack of diagnosis so far, it was decided to
proceed with microsurgical biopsy and decompression of the lesion.
Repeat MRI brain prior to surgery showed a slight increase in the size
of the lesion.
 |
|
Fig. 1 MRI brain showing
heterogeneous ring-enhancing lesion in the brainstem.
|
He underwent a sub-occipital craniotomy with excision
of the lesion via a posterior midline approach. Using the right
velo-tonsillar route, the lesion was visualized. Lesion was
xanthochromic on the surface and avascular with a pseudocapsule. It was
excised completely. Tissue was sent for histopathological examination.
Intraoperatively, the lesion seemed to be a circumscribed glioma. On
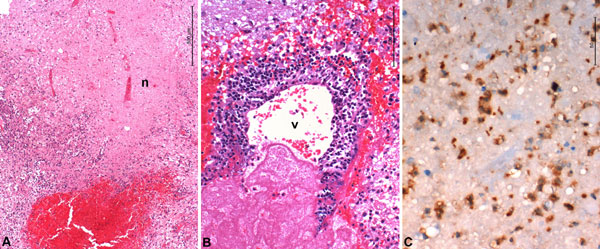
histopathology, tissue showed zones of necrosis, thrombosed vessels and
aggregates of large, foamy histiocytes with a single bradyzoite.
Toxoplasma immunostain highlighted clusters of tachyzoites (Fig.
2). The histological features were characteristic of the
encephalitic stage of toxoplasma infection.
 |
|
Fig. 2 Biopsy shows large zones of
necrosis (n), fresh hemorrhage and dense inflammation (a). Thin
walled veins show inflammation and necrosis of wall (b). Several
tachyzoite form of Toxoplasma gondii seen in the lesion on
immunohistochemistry (c). (See color images at website).
|
In view of the above diagnosis, he was further worked
up with regards to his immune status. HIV ELISA was negative (done
twice). Immunoglobulin profile was normal and peripheral blood flow
cytometry showed normal B and T cell markers. Toxoplasma IgM was also
done retrospectively after the HPE report was available and it was
positive. Due to non-availability of Sulfadiazine-Pyrimethamine
combination, which is the recommended treatment for this condition,
Trimethoprim – sulfamethaxazole (Cotrimoxazole) was started. However,
there was no improvement in the neurological status one week after
initiation of therapy. and the patient developed signs of brain stem
dysfunction in the form of fluctuating heart rates and blood pressure.
Two weeks after initiation of therapy, he died of a sudden cardiac
arrest.
Discussion
Toxoplasma gondii is transmited to humans usually
by ingestion of cysts/oocysts, transplacental or less commonly via blood
transfusion, organ transplantation and laboratory accidents [1]. While
clinical manifestation is common in immuno-compromised hosts, only about
10-20% of immuno-competent individuals present with symptoms. The most
common presentation is asymptomatic cervical lympha-denopathy while
meningoencephalitis, polymyositis and myocarditis are less commonly seen
[2].
CNS toxoplasmosis is well documented in patients with
AIDS and is the commonest cause of focal brain lesions in these patients
[3]. Other causes of focal lesions in brain stem which need to be
considered, especially in an immunocompetent individual include brain
stem glioma, acquired demyelinating disorders (multiple sclerosis, acute
disseminated encephalomyelitis, and neuromyelitis optica), infectious
brain stem encephalitis, rhombencephalitis, CNS involvement of
connective tissue disorders and other vasculitides (systemic lupus
erythematosus, Neuro-Behcet disease, and neurosarcoidosis), primary CNS
vasculitis, osmotic demyelination syndrome (CPM), brain stem ischemic
lesions and brain stem vascular anomalies [4]. In immunocompetent
individuals, CNS involvement with toxoplasmosis is extremely rare and is
generally associated with single or multiple focal lesions [2]. Isolated
brain stem toxoplasmosis with no apparent immunodeficiency, as in our
patient, has been reported in one other young adult [5].
The diagnosis is made by isolation of the organism,
demonstration of tachyzoites histopathology or by positive plasma
serology [6]. Neuroimaging features and a response to therapy have also
been used as a means of diagnosis in individuals with AIDS [3,7]. On
MRI, the lesions typically appear hypointense on T1 weighted images with
ring enhancement seen in about 70% of cases. The treatment of choice for
toxoplasmosis in an immunocompetent child is a combination of
pyrimethamine (1mg/Kg/day) and sulfadiazine (50mg/Kg 12-6 hourly) for
four to six weeks or two weeks beyond resolution of symptoms [5]. CNS
toxoplasmosis is found to respond well to antiparasitic therapy though
relapse is common in immunocompromised children. Immunocompetent adults
have shown a good response to both pyremethamine-sulfadiazine and co-trimoxazole.
The reason for a poor response to therapy is unclear
in this child. However, as this is an easily treatable condition,
toxoplasmosis should be considered in the differential diagnosis of
focal brain lesions, even in immune-competent individuals.
Contributors: All authors were
involved in patient management and manuscript writing. VV will act as
guarantor for the manuscript.
Funding: None; Competing interests: None
stated.
References
1. Montoya JG, Remington JS. Toxoplasma
gondii. In: Mandell GL, Douglas RG, Bennett JE, Dolin R, editors.
Principles and Practice of Infectious Diseases, 5th ed. Philadelphia:
Churchill Livingstone; 2000. p. 2858-88.
2. Kasper LH. Toxoplasma infection.
In: Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo D, editors.
Harrison’s Principles of Internal Medicine, 16th ed. New York:
McGraw-Hill; 2005. p. 1243-8.
3. Daras M, Koppel BS, Samkoff L, Marc J.
Brainstem toxoplasmosis in patients with acquired immunodeficiency
syndrome. J Neuroimag. 1994;4:85-90.
4. Alper G, Zuccoli SG. Isolated brain stem lesion in
children: Is it acute disseminated encephalomyelitis or not? Am J
Neurorad. 2012;10.3174.
5. Gupta A, Raja A, Mahadevan A, Shankar SK.
Toxoplasma granuloma of brainstem: A rare case. Neurol India.
2008;56;189-91.
6. Galli-Tsinopoulou A, Kyrgios I, Giannopoulou EZ,
Gourgoulia S, Maggana I, Katechaki E, et.al. Acquired
toxoplasmosis accompanied by facial nerve palsy in an immunocompetent
5-year-old child. J Child Neurol. 2010;25:1525.
7. Liesenfeld O, Wong SY, Remington JS.
Toxoplasmosis. In: Goldmann L, Bennett JC, editors. Cecil
Textbook of Medicine. 22 nd ed. Philadelphia PA, USA: W.B. Saunders;
2004. p. 2088-91.
|
|
|
 |
|

