Noise is defined as an unwanted sound. Acoustic
signals producing a pleasant sensation are referred to as ‘sound’
whereas the unpleasant sounds are referred to as ‘noise’. Noise has
emerged as a modern day pollutant and an environmental stressor. Source
can be both indoors (audio and video devices, musical toys, games,
electrical gadgets, kitchen appliances, classroom noises etc.) or
outdoors (vehicular traffic ranging from aircrafts to road traffic,
factory sirens, loud speakers, environmental noises in play grounds
etc.). Increasing pollution and industrialization has contributed to the
menace. Most of our knowledge related to hazardous effects of noise
originates from studies on occupational effect of noise in adults; where
high ambient noise exposure may result in hearing impairment, the
toxicity being dose-dependent [1,2]. Harmful effects of noise in
children may start from the intrauterine period [3]. In variance with
adults, neonates and children are passive consumers of harmful noise,
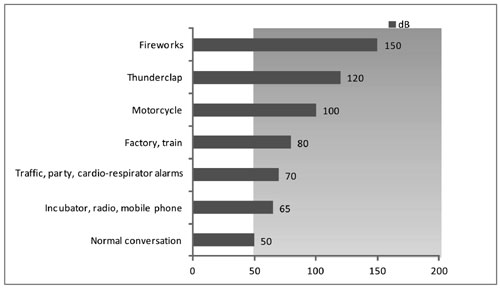
and are more susceptible to its damaging effects. Sound levels and their
adverse effects in some common situations in our surroundings are
depicted in Fig. 1.
 |
|
Fig. 1 Sound levels with their adverse
effects in some common situations.
|
Harmful Effects of Noise
Intrauterine Life
The auditory system starts developing by 3-6 weeks of
gestation [4,5], and the structural aspects required for audition are
well developed by 20 weeks of gestation. A functional vestibular system
develops by 29 weeks of gestation. That fetus is able to hear, is
indicated by observations of blink-startle responses to vibro-acoustic
stimulation during antenatal ultrasonography around 24 weeks of
gestation. Fetus can respond to auditory stimulus originating both
inside and outside the womb. Sources of sound in the materno-fetal unit
include heartbeat of mother, placental flow, mother’s voice, and
vibroacoustic stimulations from antenatal ultrasonography. Sources of
sound outside the womb depend on the environment in which the mother is
living or working. It can be from traffic signals, or from workplace
machinery for working mothers. Household sources of sound to fetus
include sounds from vacuum cleaner, mobile phone, washing machine,
televisions, radios, and loud conversations.
Hepper, et al. [4] observed that fetal
sensitivity to auditory stimulus initiates at lower frequencies;
response to higher frequencies develops later. Intrauterine exposure to
excessive sound can have long-lasting effects. Studies have documented
high frequency hearing loss in children who were exposed to noise in the
range of 85 to 95 decibels (dB) during intrauterine period [6,7]. In
utero exposure to loud noise can also cause cochlear damage. Besides
auditory damage, intrauterine exposure to noise may contribute to
prematurity and birth defects. Mamelle, et al. [8] documented
increased risk of preterm delivery in women exposed to 80 dB for an
8-hour shift. Knipschild, et al. [9] reported that women, who
resided in an area where the day-night sound level of aircraft noise
exceeded 60 to 65 dB, delivered low birth weight babies. Women residing
in areas adjacent to airport also have lower maternal placental lactogen
after 36 weeks of gestation [10].
Neonatal Period
Neonatal intensive care unit (NICU) environment is
characterized by continuous sounds from monitors, ventilators, alarms,
infusion pumps, incubators, and conversations between doctors, staff and
family. The American Academy of Pediatrics (AAP) Committee on
Environmental Health has recommended that sounds levels should be at or
below 45 dB in neonatal intensive care units (NICU) [3]. Hassanein,
et al. [11] evaluated the sound levels from equipment commonly used
in NICU and pediatric intensive care units (PICU). It was observed that
cardio-respiratory alarms increase the sound level to 73 dB,
endotracheal suctioning to 68 dB, and the telephone ringing to 83 dB.
Marik, et al. [12] demonstrated the sound inside an incubator
with all equipment off and the hood down is 53 dB, which increases to 59
dB with cardio-respiratory alarms. Intensity of sound further increases
to 68 dB with high-frequency ventilators. Normal activities in NICU thus
produce sound levels exceeding the AAP recommendations.
High intensity sounds may cause damage to the
cochlear cilia leading to hearing loss. Repeated arousal of the baby as
a result of the sounds produced by equipment may lead to fatigue and
irritability. Studies have also shown the possible synergistic effects
of aminoglycosides and noise on hearing loss in NICU graduates. Winkel,
et al. [13] studied the incidence of hearing loss in 91 preterm
NICU graduates at the age of 4-6 years; all five cases of moderate to
severe sensorineural hearing loss were seen in infants treated with
kanamycin and kept in incubators. Inappropriate sound exposure
(consistency, reverberation, frequency, and excessive levels) causes
negative neuro-sensory and physiologic long-term developmental outcomes
related to the maturation process. Johnson [14] concluded that increased
environmental sound is a cause of stress for the neonate, leading to
agitation and increased morbidity. Loud sounds interrupt sleep which is
essential for CNS development. Infants exposed to loud noises in the
NICU also demonstrate hypoxemia and changes in behavioral and
physiological responses [15,16].
Preterm infants are more vulnerable to adverse
physiological effects of noise like increased blood pressure, heart
rate, respiratory rate, and decreased oxygen saturation. Increased need
of oxygen and increase in caloric consumption are also more pronounced
in preterms [7].
Studies have shown the beneficial effects of noise
reduction in NICU. D’Agati , et al. [17] showed that earmuffs
worn by premature infants substantially increase the quiet sleep time.
Als, et al. [18], by reducing the frequency of opening and
closing of the incubator, concluded that the group treated with
environmental interventions needed considerably fewer days of
respiratory support and oxygen administration. Simple steps like
covering the infant incubator, modification of behavior of treating
physicians and nurses have shown to significantly reduce the ambient
noise [18,19].
Noise can also have long-term adverse affects on
neurodevelopmental outcome. Turk, et al. [20] conducted a
randomized control trial to evaluate the role of ear plug protection in
very low birth weight babies in NICU. Of the surviving infants at 18-22
months, those with ear plug protection scored 15.5 points higher on
Bayley Mental Development Index [20].
Beyond Neonatal Period
The source of noise in children can be both indoors
and outdoors. Rural homes are less burdened with sound exposure compared
to urban homes. Machines used in agriculture are less distressing
compared to traffic noise. Due to lack of proper planning and lack of
space in urban areas, particularly the metropolitan cities, residential
colonies and schools are placed close to busy roads, airports, railway
stations and even factories. Sources of noise inside the houses include
air conditioners, coolers, washing machine, televisions, music systems,
vacuum cleaners, video and computer games. Noise from social, cultural
and recreational activities is another nuisance, particularly in densely
populated cities. Many toys produce noise and children love to play with
them. A study in Finland on 40 toys concluded that toys which gave a
single impulse reached a peak level that was so high that even exposure
to one single impulse could cause hearing defect. Preschool children who
spend quite a good amount of time in day care institutions are also
exposed to noise originating from toys, overcrowding, and air
conditioners.
Schoolchildren spend most of their time in classroom
and playground. Noise in schools is multipronged originating from the
poor acoustics of the room, slamming of doors, noisy corridors,
ventilation systems and computers. In addition there is external noise
from road traffic particularly from schools built on highways or near
congested roads. Background noise is found to be higher in classrooms
with natural ventilation as compared to those with mechanical
ventilation as shown by a study in Denmark [21]. There is significant
drop in children’s reading performance when background noise interfered
with speech [22]. Teenagers frequently visit discotheques and concerts
where a very high sound pressure level is generated; this increases the
chances of hearing loss. Youths also turn up the volume of their car
stereo while driving, which is damaging not only for ears it further
increases the chances of traffic accidents.
Noise-induced hearing loss is particularly more
pronounced in children with learning disabilities, attention
difficulties and children on ototoxic medications. Noise-induced hearing
impairment is usually accompanied with loudness recruitment, paracussis
and tinnitus. These changes may be temporary or permanent. In 2001, it
was estimated that 12.5% American children between ages of 6 to 19 years
had hearing impairment in one or both ears [23]. Similar data for Indian
children are lacking. The ultimate results of hearing loss may range
from dejection, impairment of speech, absence of schooling and
restricted job opportunities.
Noise-induced sleep deprivation suppresses the rapid
eye movement (REM) sleep pattern [24]. The body response to noise is in
terms of fight or flight, thus resulting in adverse nervous, hormonal
and vascular changes. Exposure to noise during sleep increases the
adrenaline, noradrenaline and cortisol excretion. An increase in
cortisol indicates activation of hypothalamic-pituitary axis (HPA). Long
term activation of HPA is associated with insulin resistance,
hypertension, stress ulcers and cardiovascular diseases [24]. Another
side effect of noise is enhanced pain sensation, which may increase the
requirement of dose of analgesics.
Health hazards of noise exposure in different age
groups are summarized in Table I.
TABLE I Health Hazards of Noise in Different Age Groups
|
Timing of insult Sound (dB) |
Effects
|
|
Intrauterine
|
>80 for >8 h
|
High frequency hearing
|
|
at stretch
|
loss; Prematurity, low
|
|
|
birth weight, birth defects |
|
Newborn
|
>45 |
Damage to the cilia of the
|
|
|
cochlea leading to hearing
|
|
|
loss; Increased blood
|
|
|
pressure, heart rate, |
|
|
respiratory rate, and
|
|
|
decreased oxygen |
|
|
saturation; Increased need
|
|
|
in oxygen and energy
|
|
|
consumption. |
|
|
Changed behavioral and
|
|
|
physiological responses
|
|
|
of infants. Enhanced pain perception. |
|
Child |
>70 for prolonged period or sudden exposure to >100 |
Learning disabilities, attention difficulties. Ruptured ear
drum. |
The Steps Ahead
Pediatricians are responsible for creating parental
awareness regarding the harmful effects of noise in children. Simple
changes in the working environment can help in reducing the level of
noise in intensive care areas (e.g., responding to alarms immediately,
cleaning ventilator tubing, use of incubators with minimal opening of
ventilator hoods, use of plastic instead of metallic trash cans).
Practicing behavior changes, keeping mobile in silent mode, and use of
sound meters by patient’s bed side are other measures for decreasing
ambient sounds in hospitals. Surveillance for sound levels is essential
to facilitate early interventions. Sound levels produced by the
equipment should be one of the criteria to determine their procurement
for NICU and PICU. Universal screening of newborns for hearing loss is a
concept gaining foothold in India. Studies have shown that auditory
screening of NICU graduates help in early diagnosis and treatment before
6 months; which is an essential pre-requisite to prevent speech defects
[25].
Our daily life, whether indoors or outdoors, is full
of noise. Children brought up in this environment learn to identify
noise as the part and parcel of existence. Thus, they see no harm in
creating noise also. This trend can only be reversed by behavior change
modification, starting at parental level and percolating beyond to
family, community and population at large. Interventions are needed at
home, school, and other areas children frequent. Home appliances and
toys should be developed with a sound level below 50 dB. A potential
source of noise-induced hearing loss among youngsters is use of ear
phones. Ear buds that do not fit tightly into ear canals can be promoted
[26]. For pregnant women residing in areas with high environmental noise
like airports or industrial zones, sound proofing homes with acoustic
foam panels or installing carpets and wall coverings remain a viable
option. Noisy machines inside home (washing machines, dishwasher) should
be kept away from living areas as much as possible. Working females
should try to spend some time away from noise in library, silent zones,
or vacation to a quiet spot. Laws need to be strict regarding location
of schools and houses. There should be segregation of residential and
commercial zones while developing cities. Existing regulations against
the use of loudspeakers in social gatherings need strict enforcement.
"Cheers for ears", a pilot noise-induced hearing loss prevention program
initiated by Government of Australia [27] is a novel initiative to
reduce noise pollution.
Research is lacking in almost all areas related to
children and noise. Indian Academy of Pediatrics has not issued any
Guidelines on tolerable sounds and modes for prevention by excessive
noise. Sources and ill-effects of noise are mostly well documented.
Future research needs to focus on feasibility and role of interventions
designed to reduce and/or prevent noise. Advocates of child health
should call to emphasize and work towards the ‘Right to a Noise-free
Environment for Children.’
1. Berglund B, Lindvall T. Community noise. Arch
Center Sensory Res.1995;2:1-195.
2. Babisch W. Noise and health. Environ Health
Perspect. 2005;113:A14-5.
3. American Academy of Pediatrics, Committee on
Environmental Health. Noise: A hazard for the fetus and newborn.
Pediatrics. 1997;100:724-7.
4. Hepper PG, Shahidullah BS. Development of fetal
hearing. Arch Dis Child. 1994;71: 81-7.
5. Zimmerman E, Lahav A. Ototoxicity in preterm
infants: effects of genetics, aminoglycosides, and loud environ-mental
noise. J Perinatol. 2013;33:3-8.
6. Lalande NM, Hetu R, Lambert J. Is occupational
noise exposure during pregnancy a risk factor of damage to the auditory
system of the fetus? Am J Ind Med.1986;10: 427- 35.
7. Lary S, Briassoulis G, de Vries L, Dubowitz LM,
Dubowitz V. Hearing threshold in preterm and term infants by auditory
brainstem response. Pediatrics. 1985;107:593-9.
8. Mamelle N, Laumon B, Lazar P. Prematurity and
occupational activity during pregnancy. Am J Epidemiol.1984;119:309-22.
9. Knipschild P, Meijer H, Salle H. Aircraft noise
and birth weight. Int Arch Occup Environ Health. 1981;48:131-6.
10. Ando Y, Hattori H. Effects of noise on human
placental lactogen (HPL) levels in maternal plasma. Br J Obstet Gynaecol.
1977;84:115-8.
11. Hassanein SM, El Raggal NM, Shalaby AA. Neonatal
nursery noise: practice-based learning and improvement. J Matern Fetal
Neonatal Med. 2013;26:392-5.
12. Marik PE, Fuller C, Levitov A. Moll E. Neonatal
incubators: A toxic sound environment for the preterm infant? Pediatr
Crit Care Med. 2012;13:685-9.
13. Winkel S, Bonding P, Larsen PK, Roosen K.
Possible effects of kanamycin and incubation in newborn children with
low birth weight. Acta Pediatr Scand. 1978;67: 709-15.
14. Johnson AN. Adapting the neonatal intensive care
environment to decrease noise. J Perinat Neonatal Nurs. 2003;17:280-8.
15. Long JG, Lucey JF, Philip AG. Noise and hypoxemia
in the intensive care nursery. Pediatrics.1980;65:143-5.
16. Zahr LK, Balian S. Responses of premature infants
to routine nursing interventions and noise in the NICU. Nurs Res.
1995;44:179-85.
17. D’Agati S, Adams JA, Zabaleta IA. The effect of
noise reduction on behavioral states in newborns. Pediatr Res.
1994;35:221A
18. Als H, Lawhon G, Brown E. Individualized
behavioral and environmental care for the very low birth weight preterm
infant at high risk for bronchopulmonary dysplasia: Neonatal intensive
care unit and developmental outcome. Pediatrics. 1986;78:1123-32.
19. Saunders AN. Incubator noise: a method to
decrease decibels. Pediatr Nurs. 1995; 21:265-8.
20. Turk CA, Williams AL, Lasky RE. A randomized
clinical trial evaluating silicone earplugs for very low birth weight
newborns in intensive care. J Perinatol. 2009;29:358-63.
21. Lukas JS. Effects of aircraft noise on human
sleep. Am Ind Hyg Assoc J. 1972:33:298-303.
22. Hetu R, Truchon-Gagnon, Bilodeau SA. Problems of
noise in school settings: a review of literature and the results of an
exploratory study. J Speech Lang Pathol Audiol 1990;14:31-8.
23. Lisa Goines RN, Louis H. Noise pollution: A
modern plague. South Med J. 2007; 100:287-94.
24. Stansfeld SA, Matheson MP. Noise pollution:
non-auditory effects on health. Br Med Bull. 2003;68:243-57.
25. Rai N, Thakur N. Universal Screening of newborns
to detect hearing impairment –Is it necessary? Intern J Pediatr
Otorhinolaryngol. 2013;77:1036-41.
26. Harrison RV. The prevention of noise induced
hearing loss in children. Int J Pediatr. 2012;2012:473541.
27. Taljaard DS, Leishman NF, Eikelboom RH. Personal
listening devices and the prevention of noise induced hearing loss in
children: The Cheers for Ears Pilot Program. Noise Health.
2013~15:2618.

