|
|
|
Indian Pediatr 2015;52: 166 |
 |
Isolated Pontine Tuberculoma Presenting as
Horizontal Gaze Palsy
|
|
*Piyush Gautam and Nivedita Sharma
Department of Pediatrics, Dr R. P. Medical College and
Hospital, Tanda, Kangra, Himachal Pradesh, India.
Email: [email protected]
|
|
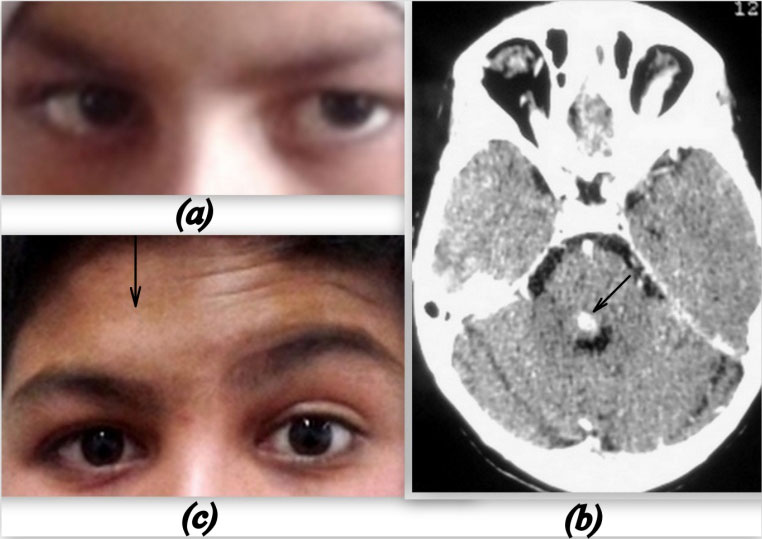
A 14-year-old boy presented with inability to move his eyes to the right
since one day. There was no history of fever, headache, vomiting or
impairment of vision. Vitals were stable while neurological examination
revealed right horizontal gaze palsy with contralateral deviation of
eyes (Fig. 1a). There was no diplopia,
while nystagmus and Dollís eye movement were absent. Pupillary reflex
and fundus examination were normal in both eyes. Respiratory system
examination revealed pleural effusion on the left side. A clinical
impression of right conjugate gaze palsy with left sided pleural
effusion, with the etiological possibility of tuberculosis was kept.
Investigations revealed hemoglobin 10g/dL, total leucocyte count in
normal range, and erythrocyte sedimentation rate of 37 mm/h. Chest X-ray
showed left sided pleural effusion and pleural tap revealed straw
coloured fluid, with an Adenosine deanimase of 87.5 U/L. Mantoux test
was non-reactive. Computerized tomography of head showed a ring
enhancing lesion, 8.7 ◊ 7.9 mm in the posteromedial aspect of the right
side of pons with perilesional edema (Fig. 1b).
 |
|
Fig. 1 (a) Right horizontal
gaze palsy with contralateral gaze; (b) Computed tomograpgh of
brain showing lesion in pons (black arrow); (c) Normal gaze at 7
weeks with right LMN facial nerve palsy.
|
The child was started on antitubercular treatment,
four drugs with prednisolone at 2 mg/kg/day. The gaze improved and was
completely normal after 4 weeks while the pleural effusion resolved
after 6 weeks. However, the child returned 3 weeks later with acute
onset of right sided facial nerve palsy, lower motor neuron type (Fig.
1c). Compliance with ATT was good and he was on tapering dose of
prednisolone. Magnetic resonance imaging of the brain showed a ring
enhancing lesion of size 6.6 ◊ 5.4 mm in the pons in the same area, with
perilesional edema. Prednisolone was continued at 2 mg/kg/day for 2
weeks and tapered-off over the next 4 weeks. The facial palsy was
completely normal 4 weeks later.
Isolated brainstem tuberculomas are rare, accounting
for 2.5-8% of all intracranial tuberculomas [1]. They commonly present
as cranial nerve palsies or focal neurological signs but presentation as
gaze palsy without diplopia is rare. [2]. Unilateral gaze palsy can
result from either a parapontine reticular formation (PPRF) or a VI
nucleus lesion [3]. The distinction between the two can be made by
Dollís eye manoeuvre, which is preserved in PPRF lesion whereas in a
nuclear lesion it is absent [3]. The close proximity of the VII nerve
fascicle to the VI nerve nucleus may result in facial nerve palsy, which
in our case developed as a paradoxical response seven weeks after
starting ATT. Paradoxical response during antituberculosis therapy
occurs in about 10-15% of patients and may develop between 14 to 270
days in HIV negative patients [4]. Brainstem tuberculoma should be
considered in the differential diagnosis of neurophthalmologic
syndromes, especially in endemic regions.
Acknowledgement: Dr Sanjeev Chaudhary.
References
1. Kumar R, Jain R, Kaur A, Chhabra DK. Brain stem
tuberculosis in children. Br J Neurosurg. 2000;14:356-61.
2. Lolly P, Rachita S, Satyasundar M. Ophthalmic
manifestations of central Nervous system tuberculosis- Two case reports.
Indian J Tuberc. 2011;58:196-8.
3. Bronstein AM, Rudge P, Gresty MA, Boulay GDu,
Morris J. Abnormalities of horizontal gaze. Clinical, oculographic and
magnetic resonance imaging findings. II Gaze palsy and internuclear
ophthalmoplegia. J Neurol Neurosurg Psychiatry. 1990;53:200-7.
4. Cheng VC. Paradoxical response during Anti tuberculosis therapy.
The Hong Kong Medical Diary. 2006; 2:20-1.
|
|
|
 |
|

