|
|
|
Indian Pediatr 2015;52: 149 -150 |
 |
Preputial Calculus in a
Neurologically-impaired Child
|
|
RI Spataru, DA Iozsa and M Ivanov
From Department of Pediatric Surgery, Emergency
Clinical Hospital for Children "Maria Sklodowska Curie", University of
Medicine and Pharmacy "Carol Davila" Bucharest, Romania.
Correspondence to: Dr Spataru Radu-Iulian: 20, Bld.
Brancoveanu C., PC 041451, Emergency Clinical Hospital for Children
"Maria Sklodowska Curie", Bucharest, Romania,
Email: [email protected]
Received: July 28, 2014;
Initial review: September 01, 2014;
Accepted: October 09, 2014.
|
|
Background: Preputial calculi are rarely encountered in childhood.
Case characteristics: A 5-year-old boy with symptoms of chronic
balanoposthitis. Observation: A preputial stone was documented
and removed at circumcision. Outcome: Uneventful postoperative
recovery. Message: In children, association between phimosis and
neurologic impairment represent predisposing condition for preputial
stone formation.
Keywords: Children, Phimosis, Prepuce.
|
|
P
reputial calculi are an uncommon entity. It has
been described in isolated case reports, mostly in elderly men, with
tight phimosis and poor hygiene [1-4]. It is postulated that these
calculi originate from inspissated smegma with lime salts trapped into
the phimotic prepuce, infected stagnant urine or migrated calculi from
the upper urinary tract into the preputial sac [1]. Preputial calculi in
children are very rare [5-7] , usually associated with phimosis and
other urologic and/or neurologic anomalies.
Case Report
A 5-year-old-male was referred to our hospital with
the presumed diagnosis of balanoposthitis. The child had paraparesis and
incontinence for urine and feces, following surgery in infancy for
myelomeningocele. The penis looked severely swollen, from the tip almost
to the penoscrotal junction. The foreskin was significantly thickened,
with a tight phimotic ring showing ulceration on its circumference,
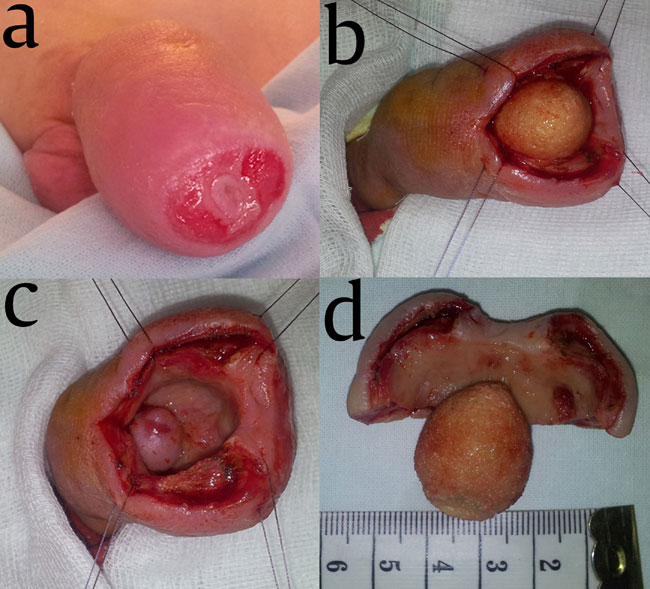
making impossible examination of the meatus opening (Fig. 1a).
No stricture band or hair tourniquet could be found along the penile
shaft or at the base of the penis. Testes and scrotum looked normal.
Significant diaper rash and pressure sores were evident in the inguinal,
perineal and sacral area. No signs of acute urine retention were noted.
The patient presented intermittent leaking urine without an obvious
stream. The patient was diagnosed with chronic balanoposthitis probably
occurring in the context of neurological impairment and tight phimosis.
Bladder catheterization for urine analysis was unsuccessful. A metal
probe was attempted to pass through the foreskin opening when a
presumable foreign body was identified with a hard, stone-like
consistency.
The radiologic examination of the abdomen and pelvis
showed a well-defined, round, radiopaque shadow in the distal penile
region. Ultrasound revealed a bright hyperechoic structure located in
the preputial sac; there were no signs of urolithiasis.
Circumcision was performed (Fig. 1 b-d)
with the removal of a thick preputial sac molded on a 3/2 cm ovalar
calculus with the glans imprint on it, light colored with a rough
surface. Penis had a normal size with an adequate meatus opening. Postop
urethral catheterization showed presence of leukocyte, but negative
urine culture. Postoperative recovery was uneventful. Chemical analysis
of the stone showed calcium oxalate with no foreign bodies found inside.
Serum and urinary levels of electrolytes and uric acid were in normal
ranges; parathyroid hormone level was also normal.
 |
|
Fig. 1 (a) Penis severely swollen,
from the tip almost to the penoscrotal junction; tight phimotic
ring showing ulceration on its circumference; (b,c,d) removal of
a thick preputial sac molded on a 3/2 cm ovalar calculus with
the glans imprint on it, light colored with a rough surface.
|
Pathological exam of the prepuce confirmed
balanoposthitis.
Discussion
In the first years of life the prepuce is attached to
the glans by physiological congenital adhesions, so there is a little
room for urine to collect in the preputial sac. There have been
described, in extremely rare cases, congenital giant deep preputial sac
with very large capacity for urine collection [8], which could favor
stone formation. In our case, no such anomaly could be identified.
Scarring of the prepuce with progressive fibrous
phimosis due to chronic pathological conditions such as Balanitis
xerotica obliterans (BXO) usually occurs in older children and adults.
Newly published data has shown a higher incidence than was previously
reported in children under the age of 5, if the diagnosis is based on
histopathological examination at the time of circumcision [9]. Our
histopathological examination was able to exclude BXO as a possible
cause for phimosis.
In adults with neurogenic bladder, 62.5% of
nephroliths were metabolic disease-related [10]. This research
highlights the importance of documenting metabolic disorders in
neurologically-impaired patients with urolithiasis. In children,
preputial stones occur in the presence of phimosis associated with other
urological and/or neurological malformation (e.g. epispadias and
low imperforated anus and myelomeningocele). Neglected preputial stones
may generate serious complications such as bilateral hydronephrosis and
acute renal failure [1], or even penile carcinoma [3]. One case
described in a child showed preputial skin fistula as a consequence of
multiple preputial calculi [7].
In our case, evaluation excluded presence of calculi
anywhere else along the urinary tract, or foreign body as a nucleus, or
signs of present urinary infection. We can assume that the possible
etiology was either migration of a proximal situated micro-calculus,
which developed further in the tight preputial sac or de novo
formation of the calculus in the stagnant urine in the preputial cavity.
In conclusion, preputial calculi can occur in
childhood, association between tight phimosis and urinary incontinence
representing a predisposing circumstance.
Contributors: SR: Conception of the work;
revising paper for important intellectual content; IDA: Analysis and
interpretation of the data for the work; drafting the work; IM:
Acquisition, analysis and interpretation of the data for the work;
drafting the work and revising it critically for important intellectual
content. All authors approved the final manuscript and take
responsibility for its conent.
Funding: None; Competing interests: None
stated.
References
1. Yuasa T, Kageyama S, Yoshiki T, Okada Y. Preputial
calculi: a case report. Acta Urol Jpn. 2001;47:513-5.
2. Hori N, Hoshina A, Kinoshita N, Kato M, Arima K,
Tajima K, et al. A case of preputial calculi. Acta Urol Jpn.
1985;31:327-9.
3. Mohapatra TP, Kumar S. Concurrent preputial
calculi and penile carcinoma a rare association. Postgrad Med J.
1989;65:256-7.
4. Nagata D, Sasaki S, Umemoto Y, Kohri K. Preputial
calculi. BJU Int. 1999;83:1076-7.
5. Sharma SK. Phimosis and the preputial calculus.
Indian Pediatr. 1983;20:386.
6. Ellis DJ, Siegel AL, Elder JS, Duckett JW.
Preputial calculus: a case report. J Urol. 1986; 136:464-5.
7. Tuğlu D, Yuvanç E, Yilmaz E, Batislam E, Gürer
YKY. Unknown complication of preputial calculi: preputial skin fistula.
Int Urol Nephrol, 2013, July 25, online, DOI 10.1007/s11255-013-0496-x.
8. Philip I, Hull NJL. Congenital giant prepucial
sac: Case reports. J Pediatr Surg. 1999;3: 507-8.
9. Jayakumar S, Antao B, Bevington O, Furness P,
Ninan GK. Balanitis xerotica obliterans in children and its incidence
under the age of 5 years. J Pediatr Urol. 2012;8:272-5.
10. Matlaga BR, Kim SC, Watkins SL, Kuo RL, Munch LC,
Lingeman JE. Changing composition of renal calculi in patients with
neurogenic bladder. J Urol. 2006;175: 1716-9.
|
|
|
 |
|

