ubacute sclerosing panencephalitis
(SSPE) is a slow progressive degeneration of the central
nervous system caused by a persistent defective measles
virus infection. The disease has a gradual progressive
course leading to death in many cases within one to three
years [1]. The latent period between measles infection and
SSPE is commonly 6-8 years [2]. We report an infant with a
very short latency.
Case Report
An 11-month-old infant presented to us
with complaints of right-sided focal seizures for 3 days
followed by myoclonic jerks and altered sensorium for last
one month. Prior to this illness, the infant was well and
achieving age-appropriate milestones At presentation, the
infant was unable to recognize his parents, unable to hold
neck or sit, and not vocalizing bisyllables. Myoclonus of
limbs was noted at the time of examination. Rest of the
clinical examination was unremarkable.
Infant was a product of non-consanguinous
marriage, and born by normal vaginal delivery. Antenatal and
postnatal period was uneventful and there was no history of
measles in mother either during pregnancy or at time of
delivery. At eight months of age, he had history of fever,
cough, coryza followed by maculopapular rash (first noticed
at forehead then descended downward), which was diagnosed as
measles by a pediatrician.
Complete blood count, serum electrolytes,
liver and kidney function test, ESR, tandem mass screening,
serum lactic acid, and ammonia were in normal ranges. Chest
X-ray was normal and Mantoux test was non-reactive.
Cerebrospinal fluid was clear with 4 cells (all
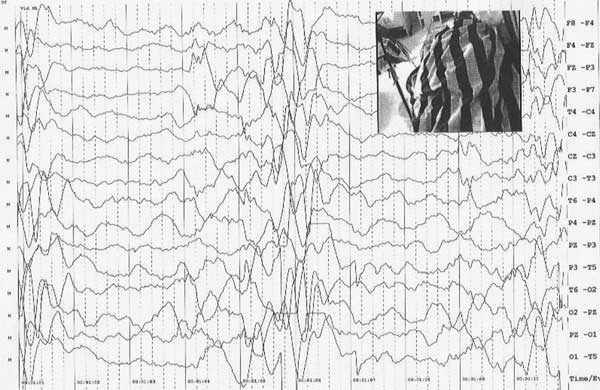
lymphocytes), CSF protein 24 mg/dL glucose 55 mg/dL. EEG
revealed periodic generalized complexes consisting of
bilaterally symmetrical, high voltage (>200µV) bursts of
sharp waves and delta waves which repeat at interval of 3 to
20 seconds interval with a slow background (Fig. 1).
Periodic burst was associated with each episode of myoclonus.
As EEG picture was suggestive of SSPE, a sample of CSF and
serum was obtained for anti-measles antibody. ELISA test
using commercial kits for IgG antimeasles antibody was found
positive both in CSF and serum (normal finding is CSF
negative for IgG antimeasles antibody). While IgM
anti-measles antibody was negative both in CSF and serum.
Blood and CSF serology for Herpes simplex, Toxoplasma
and Cytomegalovirus were all negative (both IgM and IgG).
 |
|
Fig.1 Generalized periodic
EEG pattern with a slow background.
|
MRI brain done at day five of admission
revealed hyperintense signal in the cortex and subcortical
white matter of frontal lobe. A repeat MRI done after one
month revealed diffuse cerebral atrophy of brain. Child was
treated with Isoprinosine (100mg/kg/day) but therapy with
interferon was not affordable. Sodium valproate and
clonazepam were added for control of myoclonus. However,
after three months of continuous follow up, patient did not
show any improvement in cognitive functions.
Discussion
Most of the patients with SSPE have a
history of primary measles infection at an early age.
Children infected with measles under the age of one year
carry a 16 times greater risk of SSPE than those infected at
age five year or later. The diagnosis is based upon
characteristic clinical manifestations, the presence of
characteristic periodic EEG discharges, and demonstration of
raised antibody titre against measles in the plasma and
cerebrospinal fluid [1]. The latent period between measles
infection and SSPE is around 6-8 years in most of the cases,
but may range between 3 months to 18 years [2]. In this
child, latent period of 2 months was noted which was much
shorter.
Atypical form of SSPE occurs in about 10%
of all patients. Unlike classical SSPE, in atypical form
there are no defined stages in clinical presentation due to
rapid course [3]. Atypical features also include unusual age
of onset, visual loss, seizures and other focal symptoms as
initial presentations, a lack of SSPE-specific EEG pattern,
and atypical fast progression of disease. A patient could
have more than one of these atypical features [4]. This case
is atypical as there is very early age of onset, a very
short latent period of 2 months between measles infection
and development of SSPE, and focal seizures as first
symptom.
Early onset SSPE with short onset latency
is generally associated with congenital and neonatal measles
infection. Zwiauer, et al. [5] diagnosed a case of
SSPE as early as 4 months of age after perinatally acquired
measles infection. In four of the five cases described in
the literature, onset of symptoms in the patients occurred
under one year of age. However, the diagnosis of SSPE was
made at 4 months, 13 months, 14 months, 18 months and 3
years of age in these series [5-7]. It appears that earlier
the age of measles infection, shorter will be the latent
period for development of SSPE.
The EEG pattern in our case was virtually
diagnostic [1]. CSF IgG anti-measles antibody test in our
patient was done with ELISA method, which has a sensitivity
of 100% and a positive predictive value of 100% [8]. MRI
commonly reveals focal abnormalities in the cortex and
subcortical white matter early in the course of disease and
diffuse cerebral atrophy at a later stage of disease [9].
No curative treatment is available for
SSPE but therapy with immunomodulators such as isoprinosine
and interferons; and antiviral drugs like ribavarin may help
in halting the progression of the disease [1,10].
A high index of suspicion is needed to
detect SSPE with atypical presentation. As the disease can
mimic acute encephalopathy, it is important to include SSPE
on the list of differential diagnosis of acute
encephalopathy, especially in infants.
References
1. Garg RK. Subacute sclerosing
panencephalitis. Postgrad Med J. 2002;78:63-70.
2. Sarkar N, Gulati S, Dar L, Broor S,
Kalra V. Diagnostic dilemmas in fulminant subacute
sclerosing panencephalitis (SSPE). Indian J Pediatr.
2004;71:365-7.
3. Kravljanac R, Jovic N, Djuric M,
Nikolic L. Epilepsia partialis continua in children with
fulminant subacute sclerosing panencephalitis. NeuroloSci.
2010;32:1007-12.
4. Cruzeria MM, Vale TC, Pires LA, Franco
GM. Atypical subacute sclerosing panencephalitis. Arq
Neuropsiquiatr. 2007;65:1030-3.
5. Zwiauer K, Frostenpointner E,
Popow-Kraupp T, Hauser T, Hauser E, Jellinger KA. Rapidly
progressive subacute sclerosing panencephalitis after
perinatally acquired measles virus infection. Lancet.
1995;345:1124.
6. Simsek E, Ozturk A, Yavuz C, Kocabay
K. Subacute sclerosing panencephalitis (SSPE) associated
with congenital measles infection. Turkish J Pediatr.
2005;47: 58-62.
7. Dasopoulou M, Covanis A. Subacute
sclerosing panencephalitis after intrauterine infection.
Acta Paediatr. 2004;93:1251-3.
8. Lakshmi V, Malathy Y, Rao RR.
Serodiagnosis of subacute sclerosing panencephalitis by
enzyme linked immunosorbent assay. Indian J Pediatr.
1993;60:37-41.
9. Öztürk A, Gürses C, Baykan B, Gökyiğit
A, Eraksoy M. Subacute sclerosing panencephalitis: clinical
and magnetic resonance imaging evaluation of 36 patients. J
Child Neurol. 2002;17:25-9.
10. Gascon GG. Randomized treatment study of inosiplex
versus combined inosiplex and intraventricular
interferon-alpha in subacute sclerosing panencephalitis
(SSPE): international multicenter study. J Child Neurol.
2003;18:819-27.

