|
Thirunavukkarasu Arun Babu and Noyal Mariya
Joseph
From the Department of Pediatrics, Sri Lakshmi
Narayana Institute of Medical Sciences (SLIMS), and Department
of Microbiology*, Mahatma Gandhi Medical College and Research
Institute, Pillaiyarkuppam, Pondicherry, India 607 402.
Correspondence to: Dr. Arun Babu. T, Assistant
Professor of Pediatrics, Indira Gandhi Medical College Research
Institute, Puducherry, India 605 509.
Email: [email protected]
Received: October 10, 2010;
Initial Review: October 11, 2010;
Accepted: October 22, 2010.
|
|
Small areas of
calcification in tonsils are a
common clinical finding in adults but, large well-formed concretions are very rare [1].
Tonsilloliths are due to a rare form of dystrophic
calcifications that are formed as a result of chronic
inflammation of the tonsils [2]. Tonsilloliths usually occur in
adults and are relatively rare in children [3]. We report an 8
year old boy who presented with recurrent bilateral earaches,
paroxysms of coughing and regurgitating tiny yellowish-white
foul smelling pellets. This case posed a diagnostic difficulty
before the simple diagnosis of tonsilloliths was made.
Case Report
An eight-year-old boy was referred to us by
his family physician for recurrent bilateral earaches and
self-limiting paroxysms of coughing and grunting for the last
three months. He was apparently normal between the episodes.
There was no fever, ear discharge, dysphagia or a history
suggestive of asthma. His past medical history was uneventful
except for having received two courses of empirical antibiotics
for suspected otitis media. Immunization, developmental history,
and anthropometry were appropriate for his age. Oral
examination, systemic examination, indirect laryngoscopy and
otoscopic examinations were normal. The differential diagnoses
considered at this point were convalescent pertussis and
gastroesophageal reflux disease. His baseline investigations
were normal and he did not respond to anti-reflux medications.
 |
|
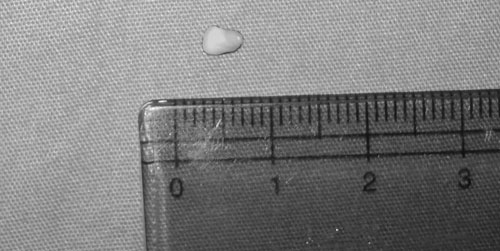
Fig.1 Tonsil Stone.
|
The boy was brought again by the mother who
complained that he was regurgitating tiny yellowish-white foul
smelling ‘worm eggs’ for the last few days and was having bad
breath. Examination of oral cavity was normal except for
halitosis. Stool microscopy was normal. We advised them to
maintain good oral hygiene and an anthelmintic drug was
prescribed. They returned in a week’s time with the regurgitant
sample. The specimen was hard in consistency, oval in shape and
yellowish-white in colour measuring around 5×2 mm. The panoramic
radiograph showed radio-opaque masses overlapping the ramus of
the right mandible. A detailed oral examination was undertaken
under local anesthesia. When gentle pressure was applied on the
anterior pillar of the right tonsil, few small white hard
structures popped out from the tonsillar crypts. These pellets
were confirmed as tonsilloliths (tonsil stones) and were
successfully removed under local anaesthesia. The post-operative
period was uneventful and the symptoms subsided.
Discussion
Tonsilloliths are calcareous concretions in
the crypts of tonsils which are usually asymptomatic and may
incidentally be found on radiographs [4]. Small concretions may
be asymptomatic, while more severe forms may present with pain
and foreign body sensation in the throat, swelling in the
tonsillar fossa, odynophagia, otalgia, peritonsillar abscess and
halitosis [1]. These are rarely seen in children [4]. Since
tonsils are supplied by glossopharyngeal nerve, any irritation
or pain can be referred to the ear along the tympanic branch of
the glossopharyngeal (Jacobson’s) nerve.
In our case, though the child presented with
earache and halitosis, we initially did not suspect tonsillolith
owing to the rarity of this condition in children and absence of
abnormal findings on oral examination. The history of extrusion
of egg-like structures was misleading and was responsible for
the delay in diagnosis. Although some worms infecting lungs
during their life cycle can present with regurgitation of eggs,
the helminthic eggs are too small to be seen with naked eye [5].
However, larval stages of housefly can be
seen in cases of oral myiasis. But they are photophobic and
often tend to hide deep into tissues for a suitable niche to
develop into pupa [6].
Tonsilloliths frequently consist of
carbonates and phosphates of calcium and magnesium [1]. The
exact pathogenesis is not known, but is believed to be
associated with chronic or recurrent oral infections [3,4].
Fibrosis near the openings of the
tonsillar crypts due to repeated inflammation may result in
accumulation of bacterial and epithelial debris and formation of
retention cysts which can subsequently calcify [2]. Unlike most
reported cases, there were no features suggestive of tonsillitis
in our case. This condition may be diagnosed by simple
inspection of both tonsillar crypts and can be confirmed by a
panoramic radiograph or computed tomography without contrast [1,
2]. Most tonsilloliths are small and asymptomatic and require no
treatment [2]. Small, symptomatic tonsilloliths can be removed
manually under local anesthesia, while large, symptomatic
tonsilloliths associated with pain, swelling and dysphagia
should be removed surgically [1].
Reference
1. Mesolella M, Cimmino M, Di MM, Criscuoli
G, Albanese L, Galli V. Tonsillolith. Case report and review of
the literature. Acta Otorhinolaryngol Ital. 2004;24:302-7.
2. de Moura MD, Madureira DF, Noman-Ferreira
LC, Abdo EN, de Aguiar EG, Freire AR. Tonsillolith: a report of
three clinical cases. Med Oral Patol Oral Cir Bucal.
2007;12:E130-3.
3. Thakur JS, Minhas RS, Thakur A, Sharma DR,
Mohindroo NK. Giant tonsillolith causing odynophagia in a child:
a rare case report. Cases J. 2008;1:50.
4. Pruet CW, Duplan DA. Tonsil concretions
and tonsilloliths. Otolaryngol Clin North Am. 1987;20:305-9.
5. Singh TS, Sugiyama H, Umehara A, Hiese S,
Khalo K. Paragonimus heterotremus infection in Nagaland:
A new focus of Paragonimiasis in India. Indian J Med Microbiol.
2009;27:123-7.
6. Sharma J, Mamatha GP, Acharya R. Primary oral myiasis: a
case report. Med Oral Patol Oral Cir Bucal. 2008;13:E714-6.
|

