|
|
|
Indian Pediatr 2011;48: 149-150 |
 |
Pseudoxanthoma Elasticum |
|
Vikram K Mahajan and Nand Lal Sharma
Department of Dermatology, Venereology and Leprosy, Dr RP
Govt Medical College,
Kangra (Tanda) 176 001, HP, India.
Email: [email protected]
|
|
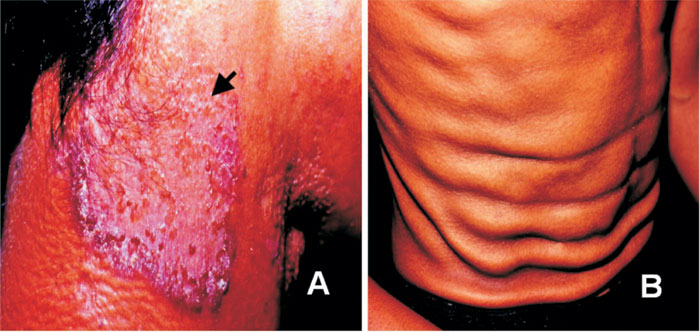
A 15-year-old boy of non-consanguineous
parentage had progressively increasing loose folded skin of three year
duration. Skin over neck, shoulders, chest and axillary folds showed
yellowish pebbly plucked-chicken skin appearance and large well-defined
atrophic plaques over neck having erythematous and ragged margins studded
with discrete keratotic papules which would bleed on removal (Fig
1). The trunk skin was soft, lax and had hanging redundant folds
(Fig 1). Hair, nails, mucous membranes and other systemic
examination were normal, and ophthalmoscopy showed no angioid streaks.
Laboratory investigations including hemogram, serum biochemistry,
urinalysis, chest X-ray, ECG, echocardiography and doppler studies
were normal. Histology showed normal epidermis, swollen, irregularly
clumped degenerated faintly basophilic and calcified dermal elastic
fibers, and mixed inflammatory cells. He was diagnosed having
pseudoxanthoma elasticum.
 |
|
Fig.1 (a) Perforating lesion of pseudoxanthoma elasticum
(arrow) showing central atrophy and discrete keratotic papules over
the erythematous margins and central atrophic skin. (b) Folded, lax,
redundant abdominal skin.
|
Pseudoxanthoma elasticum (PXE) is an uncommon autosomal
recessive disorder of generalized elastorrhexis and calcification of
elastic fibers in the dermis, Bruch’s membrane and arterial lamina.
Spontaneous perforating skin lesions with transepidermal elimination of
fragmented elastic fibers may develop manifesting as hyperkeratotic
papules. PXE needs be differentiated from yellow-orange plaques of
localized or generalized plane xanthomas seen associated with
abnormalities of lipid metabolism, and juvenile elastoma wherein skin
lesions show thickened elastic fibers histologically. A PXE-like
clinicohistopathologic syndrome in patients with
b-thalassemia,
sickle cell anemia or sickle thalassemia has late onset and is acquired as
consequences of the primary disease. In view of clinical heterogeneity,
the diagnosis of PXE requires all three major criteria; 1) The
characteristic "plucked-chicken-skin" appearance that becomes evident by
second decade and progressively becomes lax and redundant, 2)
characteristic histology and 3) angioid streaks, symmetric tears in the
Bruch’s membrane, in adults aged >20 years or, 2 minor criteria; 1)
characteristic histological changes in non-lesional skin and 2) history of
PXE in first degree relatives. Management includes timely photocoagulation
of retinal hemorrhage to prevent choroiditis and visual loss, prevention
and management of coronary occlusion, gastrointestinal or cerebral bleeds
which may end fatally otherwise, cosmetic improvement and genetic
counseling. Identification of mutations in the ABCC6 gene (chromosome
locus 16q13.1) encoding MRP6 protein provides prenatal and pre-symptomatic
testing in families at risk.
|
|
|
 |
|

