Primary vesicoureteric reflux (VUR) is caused
by a maturational abnormality of the vesicoureteric junction and passage
of urine in a retrograde manner up the ureter. Although the exact
prevalence in the general population is unknown, 30-40% of children with
urinary tract infections (UTI) are found to have reflux and urinary
tract infections occur approximately in 5-10% of children(1).
It is documented that VUR is a predisposing factor
for UTI, which in turn may involve the kidney parenchyma and cause
permanent renal scarring(1). Bailey first introduced the term reflux
nephropathy referring to the close relationship between reflux and
scarring. The severity of VUR is graded using the International Study
Classification from grade I-V, based on the appearance of the urinary
tract on contrast Micturating cystourethragram (MCU)(2). Children with
high-grade reflux (grade IV-V) who acquire a UTI are at significant risk
for pyelonephritis and renal scarring. This relationship between
scarring and the grade of reflux is shown in several studies. With
bladder growth and maturation, there is a tendency for reflux to resolve
or improve. Lower grades of reflux (grades I-III) are much more likely
to resolve than higher grades IV-V(3,4).
Hypertension and uremia are the two most serious
complications of scarring due to pyelonephritis. Proteinuria is an
important predictor of progression to end stage renal disease. The
incidence of hypertension in children with renal scarring has been
reported in more than 10%(5). Although there are a few studies on the
prevalence of VUR and renal scarring in Sri Lankan children presenting
with a documented UTI, but none evaluate the long-term outcome(5,6). The
aim of this study was to assess the long-term complications of primary
VUR.
Subjects and Methods
A prospective study was carried out on 808 children
below the age of 12 years with the initial episode of UTI, registered
from 1992 to 2004 in the renal clinic for children at Teaching Hospital,
Peradeniya.
Two consecutive midstream or clean catch samples of
urine were collected in children below the age of 12 years with a
suspected UTI. In toxic, ill children suprapubic aspiration was
performed before commencing on antibiotics. All the children with
significant bacterial growth (colony count >105 /mL) of a single
organism in the urine were diagnosed as having UTI.
Ultrasonography (USG) of the urinary tract was
performed in all children. A DMSA scan was performed 6 months after the
initial episode of UTI in all children below 5 years. MCU was performed
in all children less than two years with a confirmed UTI and in children
who had abnormalities on USG or DMSA scan. Out of 333 MCU performed
during the study period, 101 (30%) demonstrated VUR.
Children with primary VUR who had completed more than
six years of follow up were included for the present analysis. There
were fifty-six children who fulfilled the criteria. VUR was graded
according to the International Classification(2). All of them were
treated with low-dose antibiotic prophylaxis until the age of five
years. Repeat MCU was not routinely performed prior to discontinuation
of prophylactic therapy but children who developed symptomatic
break-through infections were re-evaluated with indirect radionuclide
cystourethrogram. Ureteric reimplantation was done in 2 patients who had
recurrent with grade V reflux.
Parents were educated regarding the illness, the
importance of prophylaxis and follow up. They were advised to report to
the pediatric unit with a urine culture if the child developed symptoms
of a UTI or side effects to the drugs. All the children were seen
monthly in the renal clinic under the supervision of the principal
author.
All episodes of febrile and culture positive UTI were
recorded. At each clinic visit, adverse effects to prophylactic drugs
were recorded. Urine for protein excretion (dipstick method) was
assessed once in three months and serum creatinine was checked annually.
Blood pressure was measured every three months and values were compared
with the age and sex specific percentiles for western children.
Prophylactic antibiotics were discontinued at the age
of five years. After discontinuation of prophylaxis they were followed
up periodically with assessment of the clinical status, blood pressure
and proteinuria. They were advised to report immediately if they became
symptomatic.
Results
Fifty-six children with primary VUR were followed up
for a period of 6-12 years (mean 8 years) ; 62.5% were boys with a male
to female ratio of 1.7:1. Mean age at presentation was 1.95 years (range
1 month -12 years). Seventy six percent were below the age of two years.
Thirty-three patients (58.9%) had unilateral reflux with 20 on the right
side and 13 on the left; in 23 (41.1%) it was bilateral. Majority
(48.2%) had grade III reflux while 28.6% had grade II and 8.9% had grade
I reflux. Major grades of reflux were seen less frequently, grade IV in
12.5% and grade 5 in 1.8% of patients respectively.
Thirty-one (55.3%) had detectable renal scars on DMSA
scan. Fourteen (45.2%) of them had upper pole scarring and 7 (22.6%) had
lower pole scarring of a single kidney. Five (16.1%) had involvement of
a single pole in both kidneys. Multiple scarring was noted in a single
kidney in 2 (6.4%) and in both kidneys in 3 (9.7%).
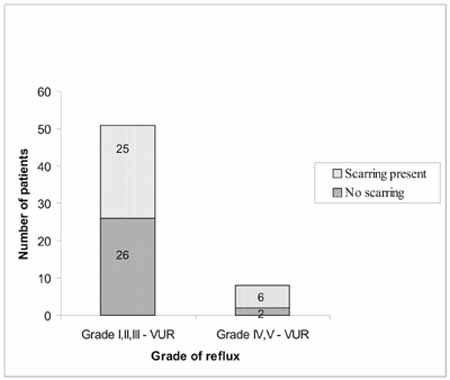
Seventy five percent of children with higher grades
(grades IV-V) of reflux and 49% children with lower grades of reflux had
detectable renal scars on DMSA scan but, standard errors of difference
between the two groups were not significant (P = 0.2).
Prophylactic antibiotics were administered to all
children until 5 years of age. Forty-eight (85.2%) received
nitrofurantoin as the first prophylactic agent and in 5 (11.1%) it was
changed to nalidixic acid due to vomiting. Four children (7.4%) received
nalidixic acid as the first prophylactic agent and were well tolerated.
Four children (7.4%) received cephalexin and co-trimoxazole. No major
adverse effects to any of the antibiotics were observed.
Eight (14.3%) patients had breakthrough UTI while on
prophylaxis and three (5.4%) had UTIs after discontinuing prophylaxis of
which only one was symptomatic.
Reimplantation of ureters was done in 2 (3.6%)
patients who had recurrent symptomatic breakthrough infections at the
ages of 3 and 10 yrs with a grade V VUR. Four patients underwent
circumcision due to recurrent balanitis and one had corrective surgery
for hypospadias.
Systolic blood pressure values in all patients were
below 90th percentile for age (Table I). Only one patient (1.8%),
with unilateral grade III reflux, had significant (1+ or above)
proteinuria. Serum creatinine values of all children were within the
normal range.
Table I
Distribution of Blood Pressure Measurements.
| Percentile |
Systolic
|
Diastolic |
| <5 |
17.3 |
3.8 |
| 5-10 |
17.3 |
- |
| 10-25 |
5.8 |
3.8 |
| 25-50 |
32.7 |
17.3 |
| 50-75 |
23.1 |
30.8 |
| 75-90 |
3.8 |
38.5 |
| 90-95 |
- |
1.9 |
| >95 |
- |
3.8 |
 |
|
Fig. 1 Renal scarring in relation to grade of VUR
|
Discussion
This study describes the long-term outcome of a group
of Sri Lankan children with primary VUR detected following a documented
UTI.
Sixty one percent with VUR in this study group were
males. This is in accordance with reports describing a male
preponderance of primary VUR in Indian children(3), although there are
some studies from other countries that report a female preponderance(7).
Renal scarring was detected in 55.3% in the study
group. The prevalence of renal scarring in children with VUR has been
reported to vary from 23-62%(7,8). The correlation between reflux and
scarring has been demonstrated in other studies. The proportion of
scarring in our study was higher in patients with higher grades (IV-V)
VUR when compared with lower grades (I-III). This is in accordance with
the finding that the risk of scarring is higher in patients with major
degrees of reflux who develop UTI, when compared with lower
degrees(7,8).
The management strategy for children with VUR has
been the avoidance of UTI induced damage by surgical correction of VUR
or long-term antibiotic prophylaxis or both. Most patients are managed
on long-term antibiotic prophylaxis until spontaneous resolution of VUR.
Almost all children except two in the study group were managed
conservatively on long- term antibiotic prophylaxis. The main drugs used
were nitrofurantoin, nalidixic acid, cephalexin and cotrimoxazole. No
patients in the study group had any major adverse reactions to drugs
e.g., hypersensitivity, peripheral neuropathy or benign intracranial
hypertension, but a few experienced minor side effects like anorexia,
nausea, vomiting and diarrhea. A systematic review of trials comparing
long-term prophylactic antibiotic use with placebo does not show any
major side effects of commonly used drugs except intolerance to
nitrofurantoin(10). Our observations are similar to findings of trials
in the published literature.
In this study, 15.3% had breakthrough UTI during
antibiotic prophylaxis. The frequency of febrile UTI reported by the
antibiotic-only arm of the International reflux study group after 5
years was 22% and combined surgery and antibiotic arm was 8-10%(11).
Inclusion of children with bilateral higher grades of VUR (grades IV-V)
may explain the higher percentage of breakthrough infections in their
study group in comparison to this study.
Studies have shown that reflux disappears without any
permanent renal impairment in a vast number of children on
prophylaxis(3,4) and therefore the management programmes for children
with VUR should take into account the self-resolving nature of reflux.
Although 55.3% of children had detectable scarring in
this cohort it is interesting to note that none of them had clinical or
biochemical evidence of deterioration of renal parameters during the
study period.
Acknowledgements
Authors acknowledge the help of C.K. Abeysinghe and
T.D. Manuwickrama in collecting data and providing care for the study
patients.
Contributors: CKA did drafting of manuscript,
analysis of data, overall supervision and contributed to patient
management. BMCDY contributed to collection and analysis of data and
literature search, ASA revised the article critically and contributed to
patient management.
Funding: None.
Competing interests: None.
|
Key Messages |
|
• Children with primary vesicoureteric reflux had detectable
renal scars in 55.3% cases.
• Majority of children with reflux
nephropathy can be managed conservatively with regular
monitoring and low-dose prophylactic antibiotic therapy without
clinical or biochemical deterioration.
|