Pulmonary agenesis is a rare condition as a result of
embryological defects, usually unilateral and is associated with
skeletal, cardiovascular and other anomalies(1). Isolated pulmonary
agenesis without any other associated anomaly except absence of right
pulmonary artery is being reported for its rarity.
Case Report
Case 1
A 13-year-old girl presented with main complaints of
poorly localized chest pain, fever, cough and expectoration for the last
two months. There was no past history of similar complaints. Her two
siblings were asymptomatic. The perinatal and develop-mental history was
normal. No parental con-sanguinity was present. She was moderately built
and nourished with mild pallor. There was no jaundice, edema,
significant lymph-adenopathy or any obvious congenital abnormality.
Chest examination showed diminished movements of chest on the right side
with trachea deviated to the right side. No breath sounds could be heard
over the right hemithorax. Normal heart sounds were heard on the right
side. Rest of the examination was unremarkable.
X-ray chest (Fig. 1) showed complete
opacification of right hemi-thorax with hyperinflation of left lung and
herniation to the contralateral side with shifting of mediastinum to
right side. Pulmonary function tests showed moderate restriction with no
airway obstruction. Three consecutive sputum examinations for AFB were
negative. Sputum pyogenic cultures showed S. pneumoniae.
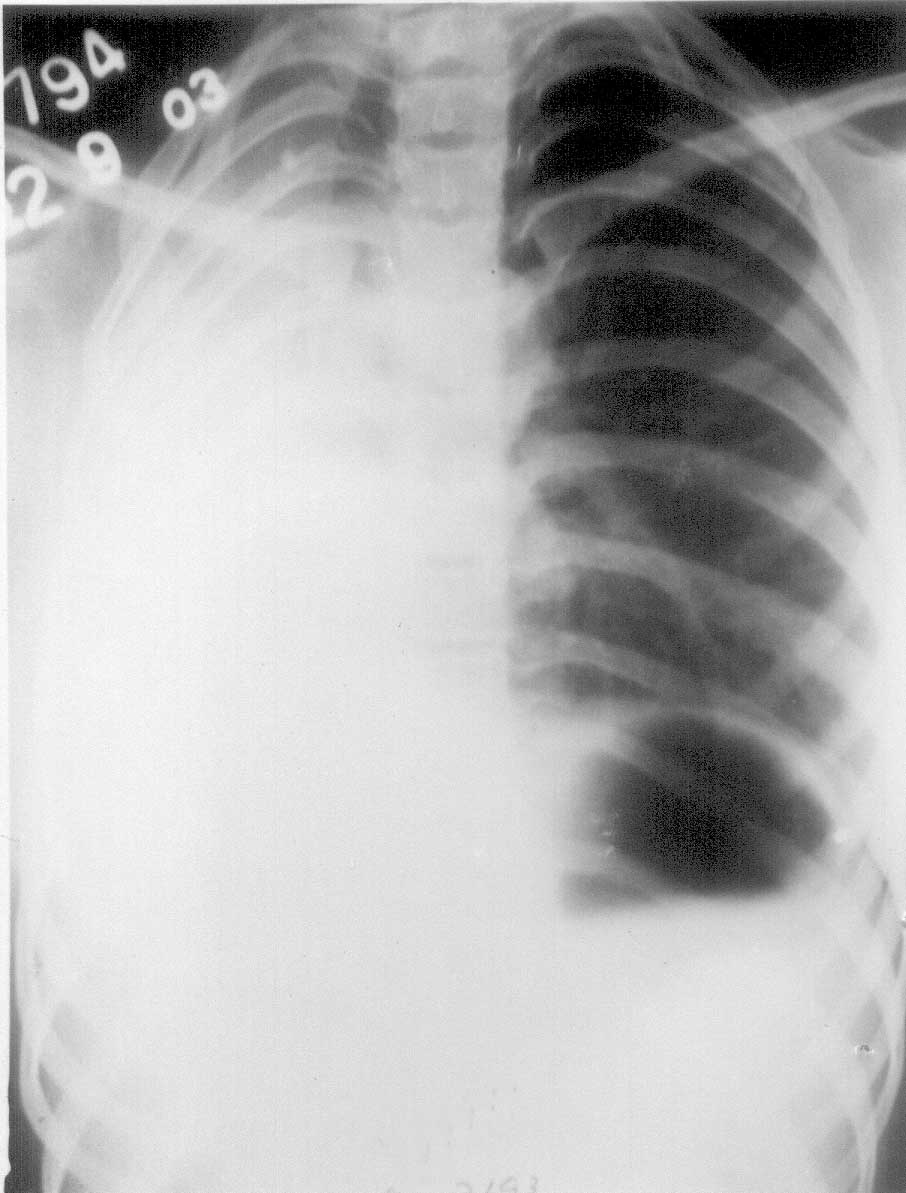 |
| Fig. 1.
Showing complete opacification of right hemi-thorax with
hyperinflation of left lung. |
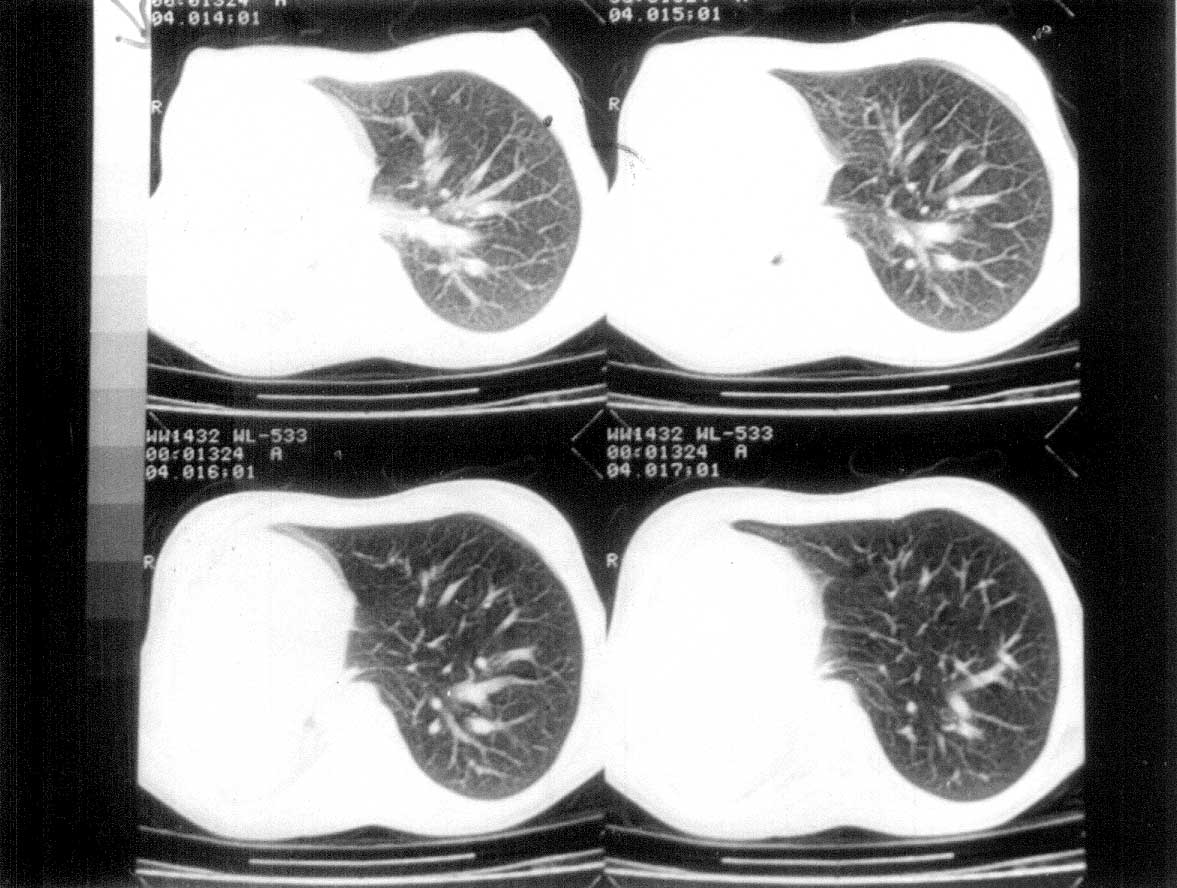
HRCECT scan chest (Fig. 2) showed no evidence
of any lung parenchyma on the right side. Apical region showed a small
soft tissue with focal calcification. Pulmonary trunk was located
anterolateral to ascending aorta with absent right branch of pulmonary
artery. Echocardiographic examination showed dextroposition of the heart
with no other cardiac anomaly. Ultrasound abdomen, X-rays of
hands, face, spine, pelvis and lower limbs were normal. Bronchoscopy
confirmed the diagnosis.
 |
|
Fig. 2. Showing HRCECT of chest with absent
lung parenchyma on right side, absence of right branch of
pulomonary artery. |
The pneumonia responded to a course of amoxycillin
and is on follow-up regularly.
Case 2
Second case was a 10-year-old girl born of
non-consanguineous parents. She presented with fever, cough and
expectoration of about one year duration. She also complained of
progressive, non-paroxysmal dyspnea. There was no past history of
similar complaints, tuberculosis, measles, diabetes and chicken pox.
Both parents had sputum positive pulmonary tuberculosis and had
completed anti tubercular therapy and were cured. She was moderately
built and nourished. Chest examination revealed diminished movements
over left side of chest with trachea and apex beat shifted to the left
side. Auscultation showed no breath sound over interscapular and left
supra-scapular region with coarse crackles over left infra-scapular
region. Cardiovascular examination was normal.
X-ray chest PA view showed a homo-geneous shadow
over left upper zone and a non- homogeneous shadow over left lower zone
with trachea and heart shifted to the same side, Left lateral film
showed a homogenous shadow over posterior mediastinum.
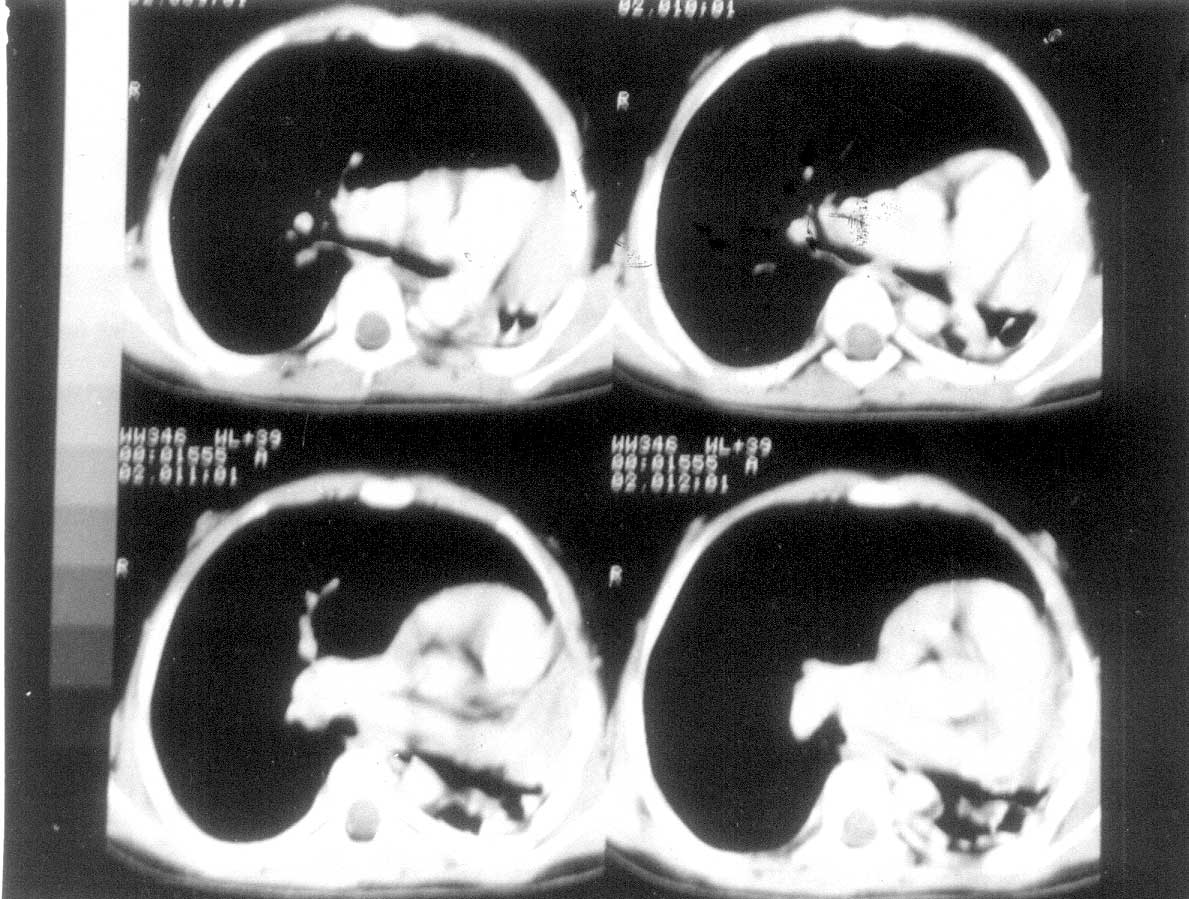
HRCECT scan chest (Fig. 3) showed reduction in
volume of left hemithorax, left upper zone had low attenuating soft
tissue opacity with no airways and communication with the bronchial
tree. Left upper lobe bronchus was not visualized, Left lower lobe
showed parenchymal destruction with cavitary changes. Right lung was
hyper inflated with herniation. Pleura was normal. These features were
suggestive of complete bronchial atresia of left upper lobe with
destroyed left lower lobe with compensatory over inflation of right
lung, There was agenesis of upper lobe of left lung.
 |
|
Fig. 3. HRCECT chest shows reduction in lung
volume of left hemithorax with no airways and communication with
the bronchial tree. Left lower lobe showed cavitory changes. |
Bronchoscopy under general anesthesia showed normal
right bronchial tree. Left upper lobe bronchus was absent and left lower
lobe bronchial tree showed inflammation with mucoid secretions. Acid
fast bacilli were isolated in bronchial washings and also in gastric
aspirate suggesting co-infection with pulmonary tuberculosis. Category I
anti tubercular therapy was started.
Discussion
Pulmonary agenesis usually presents in childhood but
may present in later life. If not complicated by other anomalies it is
quite compatible with normal living. Pulmonary agenesis needs to be
differentiated from pulmonary hypoplasia by the absence of bronchial
tree on bronchoscopy and the absence of lung tissue on radiological
investigations(2). Diagnosis is usually made by chest X-ray and
CT scan, and invasive procedures like bronchography, broncho-scopy and
angiography can be avoided(3). The typical CT findings are opaque
hemithorax with mediastinal shift towards the affected side with absence
of lung paren-chyma; pulmonary and bronchial tree as seen in our Case
1(4,5).
The condition is asymptomatic unless compromised by
infection, which can be bacterial (as in Case 1) or even mycobacterial
(as in Case 2). Differential diagnosis is from atelectesis,
diaphragmatic hernia which can be differentiated with the help of
tomography (HRCT), bronchography, and angiography (6). Asymptomatic
cases do not require any treatment especially when no other anomalies
are present. Chest infections are to be treated energetically. These
cases are high-risk cases for any surgery because of low respiratory
reserve and anesthetist and surgeon should take appropriate
precautions(6).
