Rabies vaccines containing neural elements of lower
animals are associated with neurological complications like
encephalitis, encephalomyelitis, myeloradiculitis and
polyradiculitis(1-4). These neural vaccines are still used in many
countries including India(1,2). There is a paucity of Indian literature
on the adverse neurological effects of the rabies vaccines including the
sheep brain vaccine. It is essential that these are highlighted so that
scientific evidence compels the community to discontinue the use of
these animal brain vaccines, to promote the use of safer rabies vaccines
and to take appropriate measures to control the menace of animal bites.
We report three cases who presented to us in years 2000-2001 with varied
neurological complications caused by the neural tissue containing rabies
vaccines.
Case Reports
Case 1: A 2˝-year-old boy presented with
high-grade fever, irritability and altered sensorium for two days. The
child had received one dose of beta propiolactone inactivated neural
rabies vaccine and four doses of chick embryo cell culture vaccine
(following an unprovoked dog bite on the dorsum of the right hand) 3
weeks ago. The patient had history of multiple seizures, poor feeding,
unsteadiness of gait and irrelevant speech.
On examination, the child was febrile. His vital
parameters were normal. Ataxia was the only abnormal neurological
finding in addition to drowsiness. The CT-scan of the brain showed
evidence of diffuse cerebral edema. The examination of the cerebrospinal
fluid (CSF) demonstrated 11 polymorphs, 9 lymphocytes and 4
erythro-cytes with normal concentrations of protein (42 mg/dL) and sugar
(55 mg/dL with the simultaneous blood sugar level of 92 mg/dL).
Treatment to decrease cerebral edema (mannitol) was instituted. Over the
next five days, his senso-rium worsened and the patient developed
hyperventilation, hypertonia, brisk reflexes, extensor plantar responses
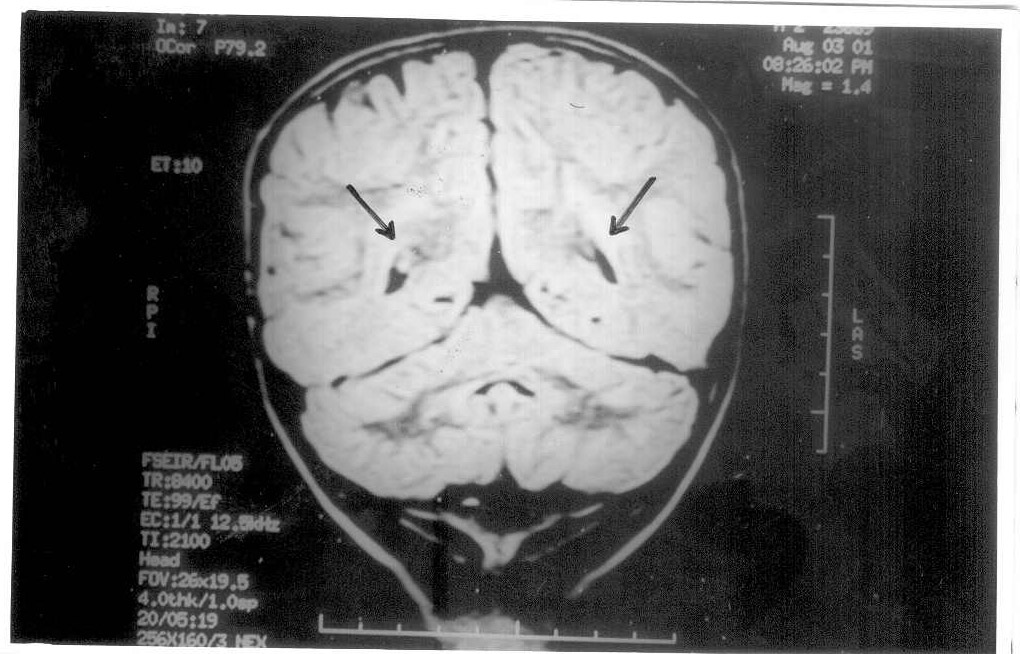
and quadriparesis. In view of the clinical deterioration, MRI of the
brain was performed which revealed altered signals in the parasagittal
area and pons suggesting demyelination (Fig. 1). The child was
treated with intravenous fluids, intravenous methyl prednisolone for 5
days, antibiotics and physiotherapy. The child did not have any
improvement in sensorium or neurological signs. Three weeks later he was
discharged from the hospital but with residual quadriparesis and
intellectual deterioration.
 |
|
Fig. 1. MRI brain of case 1. Coronal section at
level of trigone of the lateral ventricle and through the 4th
ventricle. Note the hyperintensities in the peritrigonal deep
white matter suggestive of demyelination (arrows). |
Case 2: A 12-year-old boy presented with moderate
grade fever, pain in the neck and upper back and distal weakness of the
right limb of six days’ duration. He had been bitten by a stray dog on
his left thigh 15 days earlier and had received neural rabies vaccine
for seven days. History of trauma, altered sensorium, speech and gait
disturbances were absent. The child was neurologically normal prior to
this episode.
On general examination, the child had normal vital
parameters. The neurological examination was normal except for weakness
of the distal muscles of the right upper limb. The grip was weaker in
the right hand. His blood counts and biochemical tests were normal. The
MRI of cervico-dorsal spinal region showed demyelination (Fig. 2).
EMG-Nerve Conduction (NC) was normal. There was complete spontaneous
recovery over next one week.
 |
|
Fig. 2. MRI spine of case 2. T1 weighted
sagittal section of cervicodorsal spine showing cord edema from C2
to C6 with hyperintensity within the spinal cord suggestive of
demyeli-nation and effacement of subarachnoid space. |
Case 3: A 7-year-old boy presented with
progressive weakness of lower limbs followed by upper limbs with pain in
the limbs since five days. He had dog bite on the right thigh three
weeks back and had received seven doses of beta propiolactone
inactivated neural rabies vaccine for post-exposure prophylaxis. There
was no respiratory illness or gastroenteritis preceding the weakness.
On examination, the patient had normal vital
parameters. On central nervous system examination, the higher functions
and cranial nerves were normal. There was hypotonia of all limbs with
quadriparesis; the lower limbs being more affected (muscle power 1/5)
than the upper limbs (muscle power 2/5). Deep tendon reflexes and
plantar reflexes were absent. Bladder/bowel involvement was lacking and
there was absence of any sensory level. The clinical impression was
acute inflammatory demyelinating polyradiculo-neuropathy (AIDP). The
child was treated with a five-day course (400 mg/kg/day) of intravenous
immunoglobulin and physio-therapy. His blood counts, renal and liver
function tests were normal. The EMG-NC showed peripheral demyelinating
neuropathy. The patient showed gradual improvement in muscle power over
the next 7 days (muscle power of 4/5) and could stand and walk with
support at discharge (after 10 days of ward stay).
Discussion
Developing countries continue to use the neural
tissue rabies vaccines despite the high frequency of serious
neurological complica-tions such as encephalitis, encephalomyelitis,
myeloradiculitis and polyradiculitis(1-4). The frequency of neurological
complications following anti-rabies vaccines varies from 1 in 600 to 1
in 1575 vaccinations(2).
The pathogenesis involves demyelination occurring due
to an autoimmune reaction against myelin, triggered by the vaccine(1,2).
All of our cases demonstrated lesions of demyelination in various parts
of the nervous system. They had received neural tissue rabies vaccine.
It is interesting to note that Case 1 had received one dose of neural
tissue rabies vaccine and four doses of the chick embryo cell culture
vaccine.
The availability of neuroimaging modalities like CT
scan and MRI offer an opportunity to visualize the nature of the lesions
and their extent and severity. The radiological features of
demyelination are better appreciated on MRI rather than the CT scan(1).
MRI lesions of acute demyelinating encephalomyelitis (ADEM) complicating
the use of neural-tissue containing rabies vaccine have been described
by Bavdekar, et al.(1). The MRI findings in the report included
hyper-intense signals in the thalami, basal ganglia, cortex and corpus
callosum(1). High signal lesions in the cerebrum, deep grey matter,
cerebellar peduncles and brainstem have been reported as well(1,2).
These MRI changes are similar to those seen in ADEM following infections
(1,2). Resolution of these lesions has been reported(2). As noted in
Case 2, involvement of the spinal cord consists of swelling and
alteration of signals extending over several segments(2). Case 1 and 2
demonstrated various characteristic features on MRI. The clinical
presentation reflects the topographic extent of the lesion and the
severity of involvement.
The prognosis seems to be variable. The patients with
demyelination can be treated with steroids. Complete recovery is
possible with both brain and spinal cord involvement (as seen in Case
2). Some patients may be left with partial improvement while others may
have significant permanent neurological deficits(1,2). Given the hazards
of serious and permanent neurological handicap associated with neural
tissue rabies vaccines, there is an urgent need for a change over to the
use of safer tissue culture derived products. Use of these tissue
culture vaccines is also not without complications as illustrated by the
report of acute inflammatory demyelinating polyradiculoneuropathy – AIDP
(Landry- Guillian-Barre-Strohl syndrome) following chick embryo
vaccine(3). Case 3 had AIDP due to the neural rabies vaccine. One of the
cases reported here (Case 1) had received four doses of the chick embryo
cell culture vaccine following a single dose of neural tissue rabies
vaccine. It is practically impossible to implicate either of the
preparations in causation of the neurological manifestations. Such
instances following the tissue culture rabies vaccine are an exception
and should not discourage the preferential use of tissue culture rabies
vaccine for post-exposure prophylaxis. Newer generation rabies vaccines
that do not use animal neural tissue should be preferred for the
post-exposure prophylaxis, as has been advised by the Committee on
Immunization of the Indian Academy of Pediatrics(5).
Acknowledgement
The authors thank Dr. N.A. Kshirsagar, Dean, Seth G.S.
Medical College and KEM Hospital, Mumbai for granting permission to
publish the manuscript.
