|
|
|
Indian Pediatr 2019;56: 1059 -1061 |
 |
IgG4-related Disease at Rectovesical Pouch Mimicking
Inflammatory Myofibroblastic Tumor
|
|
Souradeep Chakrabarti 1*,
Priyankar Pal1,
Shirsendu Dutta1 and
Ritambra Nada2
From 1Department of Pediatrics, Institute of Child
Health, Kolkata, West Bengal and 2Department of Histopathology, PGIMER,
Chandigarh; India.
Email:
[email protected]
|
|
Fever of unknown origin frequently
remains a diagnostic challenge. Immunological diseases account for about
20- 30% cases of these fevers. We report the case of a boy who presented
with high fever for 2 months and was finally diagnosed as a case of
IgG4-related disease at the rectovesical pouch.
Keywords: Inflammation, Pyrexia of unknown
origin, Positron emission tomography.
|
|
I
gG4-related disease is an immune-mediated chronic
inflammatory condition characterized by tissue infiltration with
lymphocytes and IgG4-secreting plasma cells with various degrees of
fibrosis [1]. It is a relapsing–remitting disease associated with a
tendency to mass forming, tissue destructive lesions in multiple sites
with systemic symptoms like fever and allergies.
A 9-year-old boy presented to us with intermittent
fever for 2 months (102 0-1030F,
usually 2 peaks/day). Other than mild pallor, systemic examination was
normal. Investigations showed hemoglobin of 8.2 g/dL, total leukocyte
count 12.4x109/L (Neutrophil
80%, Lymphocyte 10%) with persistently high C-reactive protein (270, 301
and 276 mg/L on three separate occasions done at an interval of 5 days)
and elevated platelet count (820x109/L).
Serum ferritin was 657 ng/mL (Normal 7-84 ng/mL). Urea, creatinine,
serum electrolytes, liver function test, Lactate dehydrogenase, uric
acid, procalcitonin, and urine microscopic examination were normal;
cultures showed no growth. Scrub typhus, tuberculin skin test, sputum
for acid fast bacilli (AFB) and Cartridge based nucleic acid
amplification test (CBNAAT), brucella IgM, Epstein barr virus (EBV) VCA
IgM, and parvo virus IgM were negative. Antinuclear antibody (ANA) was
not raised. Chest X-ray, USG whole abdomen with color doppler of
abdominal vessels and echocardiography were normal. Bone marrow
aspiration and biopsy were also within normal limit.
 |
|
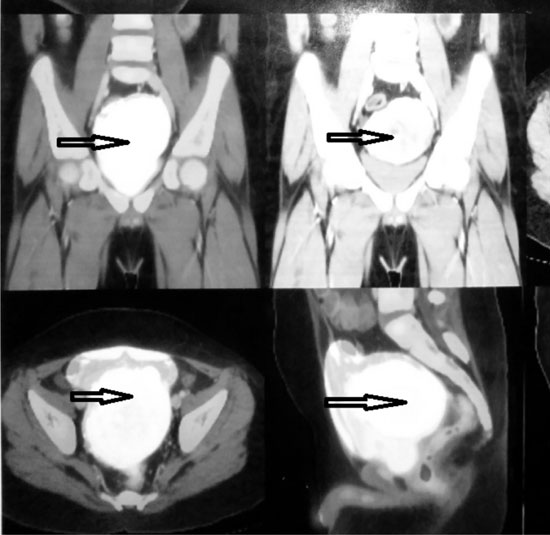
Fig. 1. PET–CT scan in coronal and
sagittal plane shows a large lobulated necrotic mass (87 mm × 75
mm × 59 mm) at rectovesical pouch with increased FDG uptake.
|
Considering high levels of acute phase reactants, a
whole body Positron emission tomographic scan (PET scan) was planned to
find out any hot spot, especially to look for any occult malignancy. PET
CT scan revealed a large lobulated mass (87 mm X 75 mm X 59 mm) in the
rectovesical pouch with intense heterogeneous enhancement, increased
fluorodeoxyglucose (FDG) uptake with central area of necrosis, preserved
perilesional fat planes and without evidence of any distal metastasis (Fig.
1). Fine needle aspiration cytology (FNAC) showed interlacing
spindle cells against a backdrop of dense chronic inflammatory
infiltrate suggestive of an inflammatory myofibroblastic tumor and
excision biopsy was planned.
Histopathology of the excision biopsy specimen showed
interlacing fascicles of spindle cells and extensive storiform fibrosis
associated with dense inflammatory cell infiltrate comprising of
lymphocytes and many plasma cells, which were more around the blood
vessels. Myofibroblastic cell proliferation and obliterative phlebitis
were noted. IgG4 immuno-staining showed increase in IgG4 positive plasma
cells (30-40/HPF). There was no nuclear atypia or increase in mitosis or
atypical mitosis. Immuno-stain for CD34, beta catenin and anaplastic
lymphoma kinase (ALK) were negative. The overall morphology was
consistent with IgG4-related disease. Serum total IgG was 2270 mg/dL
(cut off <1600 mg/dL) and IgG4 was 469 mg/dL (cut-off <135 mg/dL).
The fever subsided within 5 days of the complete
surgical excision of the mass and he remains asymptomatic after 12
months follow-up.
IgG4-related disease is a spectrum of disorders
previously appreciated as separate entities sharing particular
pathologic, serologic and clinical features [1]. It should be suspected
when there is an infiltrating mass involving one or more organs with
signs and symptoms of inflammation, particularly when serum IgG level is
very high and possibility of malignancy has been excluded. Pathogenesis
of the disease is poorly understood. It is thought that both autoimmune
and allergic mechanisms are central to the disease pathophysiology.
Mainly Th2 cytokines like IL10 and TGF beta play a major role in the
disease pathogenesis. Major presentation of this condition, which often
affects more than one organ include: (i) autoimmune pancreatitis;
(ii) sclerosing cholangitis; (iii) salivary and lacrimal
gland enlargement; (iv) retroperitoneal fibrosis and related
disorders; (v) thyroid diseases including Riedel’s thyroiditis; (vi)
lung and pleural diseases; and (vii) renal involvement causing
tubulointerstitial nephritis [2].
Diagnosis is based upon characteristic biopsy findings
with positive IgG4 staining. Serum IgG4 concentration and blood
plasmablast concentration are other biomarkers for diagnosis.
Inflammatory myofibroblastic tumor, an uncommon
benign tumor seen in children and young adults, usually is made up of
myofibroblastic spindle cells. Common organs involved are lung, orbit,
peritoneum and mesentery [3]. Diagnosis is based on the histology of the
spindle cells and plasma cells rich in background that specifically
stains with anaplastic lymphoma kinase-1(ALK-1) [4]. Though some
overlapping features of both the conditions with respect to clinical
presentations, location of the lesions and gross histology confused the
treating physicians initially, special staining with elevated serum IgG4
level finally helped in clinching the diagnosis.
All patients with symptomatic IgG4-related disease
requires treatment and glucocorticoids are the first line agents.
Immunosuppressives like rituximab, azathioprine and mycophenolate
mofetil are used in steroid-resistant cases [5]. Surgery and
radiotherapy are other modalities of treatment. Prognosis has not been
well defined. Majority responds well with standard treatment but most of
them relapse subsequently. Some studies suggest an increased risk of
malignancy but the issue remains controversial [6].
Contributors: SC, SD: investigated the case and
drafted the manuscript; PP: supervised the case management and provided
critical inputs to manuscript; RN: final diagnosis on histopathology of
the tissue sample and helped in finalization of the manuscript.
Funding: None; Competing interest: None
stated.
References
1. Kamisawa T, Zen Y, Pillai S, Stone JH.
IgG4-related disease. Lancet. 2015; 385:1460-71.
2. Rudmik L, Trpkov K, Nash C, Kinnear S, Falck V,
Dushinski J, et al. Autoimmune pancreatitis associated with renal
lesions mimicking metastatic tumours. CMAJ. 2006;175:367-9.
3. Coffin CM, Hornick JL, Fletcher CD. Inflammatory
myofibroblastic tumor: Comparison of clinicopathologic, histologic, and
immunohistochemical features including ALK expression in atypical and
aggressive cases. Am J Surg Pathol. 2007;31:509-20.
4. Ardini E, Magnaghi P, Orsini P, Galvani A,
Menichincheri M. Anaplastic Lymphoma Kinase: Role in specific tumors,
and development of small molecule inhibitors for cancer therapy. Cancer
Lett. 2010;299:81-94.
5. Khosroshahi A, Wallace ZS, Crowe JL, Akamizu T,
Azumil A, Carruthers MN, et al. International Consensus Guidance
Statement on the Management and Treatment of IgG4-Related Disease.
Arthritis Rheumatol. 2015;67:1688-99.
6. Yamamoto M, Takahashi H, Tabeya T, Suzuki C, Naishiro Y, Ishigami
K, et al. Risk of malignancies in IgG4- related disease. Mod
Rheumatol. 2012;22:414-8.
|
|
|
 |
|

