|
|
|
Indian Pediatr 2019;56: 1029-1032 |
 |
Limited Dorsal Slit Preputialplasty for
Management of Phimosis in Children
|
|
Pradyumna Pan
From Pediatric Surgery Unit, Ashish Hospital and
Research Center, Jabalpur, Madhya Pradesh, India.
Correspondence to: Dr Pradyumna Pan, Pediatric
Surgery Unit, Ashish Hospital and Research Centre, Jabalpur, Madhya
Pradesh 482 001, India.
Email: [email protected]
Received: January 07, 2019;
Initial review: June 06, 2019;
Accepted: September 19, 2019.
|
|
Objective: To evaluate the functional and cosmetic result of limited
dorsal slit preputialplasty for surgical management of phimosis in
children. Methods: This is a prospective cohort study (Jan 2010
to Dec 2019) of 246 children (age >5 y) who were unable to retract the
foreskin and were symptomatic. Results: No intraoperative
complications were encountered. Preputial edema was the most common (n=45,
18.2%) immediate postoperative occurrence. At one year follow-up, a
total cosmetic score of 6 (considered optimal) was seen in 203 (91%)
patients. A score of 5 was observed in 13 (5.9%) and the remaining 7
(3.1%) had a score of less than 4. All pubertal children, except one,
could retract prepuce freely without discomfort. Conclusion: This
preputialplasty provides satisfactory cosmetic and functional result in
phimosis, and is an acceptable alternative to circumcision.
Keywords: Circumcision, Surgery,
Treatment.
|
|
P hysiologic phimosis is common
in newborn males due to flimsy adhesions between glans and prepuce. The
adhesion to glans and prepuce separates over time reducing to 50% at the
age of two years, 8% by seven years, and 1% by eighteen years of age.
Poor hygiene and recurrent balanoposthitis lead to the development of
true phimosis [1]. In children with phimosis, preputialplasty represents
a surgical alternative to circumcision, which is associated with many
functional and physiologic problems [2-4]. Complications like
hemorrhage, edema, infection, meatal stenosis, urethral fistulae, scars,
penile curvature, shortness of shaft skin, and partial or total penile
loss have been reported after circumcision [5]. Preputial-plasty
broadens the preputial meatus to permit its simple withdrawal and better
cleanliness while maintaining the typical cosmetic appearance of the
penis. This study aimed to evaluate the short-and long-term functional
and cosmetic results, and the patients’ and parents’ acceptance of
limited dorsal slit preputialplasty.
Methods
This prospective observational study was carried out
over a period of eight years (January 2010 to December 2018) in a
tertiary referral center. Institutional review board and ethical
committee approval was obtained. Parental preference and consent for
preputialplasty was obtained in these patients after discussing the pros
and cons of both circumcision and preputialplasty. We excluded patients
with balanitis xerotica obliterans or those with severely scarred
fibrotic prepuce. Participants included children older than five years
with pathological phimosis complicated with ballooning, straining,
recurrent balanoposthitis, painful erections, recurrent urinary tract
infection (UTI), urinary retention, preputial stenosis resistant to 3
months trial of adhesiolysis and retraction by parents, minimally
scarred prepuce or redundant prepuce.
All children underwent limited preputialplasty, which
is a modification of the classical dorsal slit technique. The foreskin
is mobilized, dividing glandular adhesions, and retracted to show the
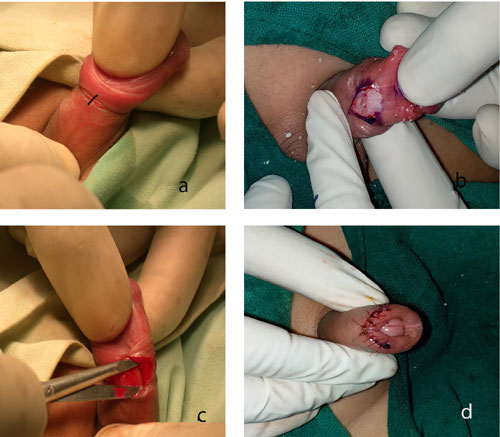
tight constricting band (Fig. 1a). The incision is given
longitudinally along the dorsum of the penis only over the band till the
bucks’ fascia (Fig. 1b). Space is created by undermining
into both lateral sides for 4-6 mm (Fig. 1c) and repeat
incision made on the ring laterally through the same incision. The
incision is closed transversely with absorbable 5/0 vicyrl rapid sutures
(Fig. 1d). This widens the tube of the prepuce and allows
its free movement. All procedures were conducted as day-care surgeries
under sedation and penile block by the author.
 |
|
Fig. 1 Steps of preputialplasty: (a)
showing tight constricting band after full prepuce retraction;
(b) showing incision over the band; (c) showing the creation of
lateral space; and (d) at the completion of preputialplasty.
|
All children underwent follow-up evaluation at 1, 3
and 4 weeks, and 3 and 6 months. The outcome was assessed in terms of
preputial edema, bleeding, retention of urine, discomfort in wearing
pants, infection, para-phimosis, retractibility, recurrence, sexual
pleasure (if applicable) and parental satisfaction for cosmesis. At 1
year follow-up, the modified Hollander wound evaluation scoring was done
[6,7]. Wound clinical examination was based on absence of step-off,
contour irregularities, wound margin separation >2 mm, edge quality,
distortion, and overall cosmetic appearance. Each of these categories
was graded on a 0 or l point scale. A total cosmetic score was derived
from the addition of the six categorical variables. A score of 6 was
considered the best, while lower scores suggested suboptimal results.
All patients were evaluated for the outcome by the author and one
independent observer.
Results
A cohort of 246 boys was studied with mean (SD) age
of 9.87 (1.87) years. The operating time ranged between 20 and 35
minutes. All children had presented with problems consequent to
pathological phimosis (Table I). No intraoperative
complications were encountered. The dorsal slit measured between 4 to 7
mm. There was no postoperative distress, postoperative bleeding or any
problems in passing urine. There was no need for the overnight stay, and
none required catheterization for urinary retention. All the children
after operation were able to wear pants immediately without any
discomfort. Preputial edema was the most common immediate postoperative
event encountered in 45 (18.2%) patients, which subsided in 3 to 5 days
in all except four (1.7%) patients with long redundant prepuce who
required 10-14 days for preputial edema to subside. Complaints of
burning during micturition (n=6, 2.5%) and straining (n=5,
2%) were seen in the first postoperative week. Bluish discoloration
suggesting hematoma was noticed in two patients which resolved within a
week. Mild inflammation also occurred in 6 (2.5%) patients. No patient
had wound infection or disruption. Wound healing was satisfactory in all
the patients at one month follow-up. Parents of the patients were
comfortable in learning and performing preputial retraction and
reposition at 7 th day
post-operative follow-up. The majority (178, 72.3%) could mobilize
foreskin freely without discomfort from the second week, or within 3
weeks (176, 92.7%). Two patients had paraphimosis following
preputialplasty. Twenty-three patients were lost to follow-up between
the 3rd and the 6th
months after surgery.
TABLE I Presentation of Pathological Phimosis in Children Older Than 5 Years (N=246)
|
Clinical presentation |
n (%) |
|
Ballooning and straining |
179 (72.8) |
|
Recurrent UTI |
21 (8.6) |
|
Recurrent posthitis |
17 (6.9) |
|
Long prepuce
|
11 (4.5) |
|
Minimally scarred prepuce |
9 (3.7) |
|
Painful erection |
7 (2.9) |
|
Urinary retention |
2 (0.9) |
At 3-month follow-up, no patient had a recurrence.
Minimal adhesions seen in 18 (7.5%) patients were separated, using
topical lignocaine. Four patients (1.8%) had partial narrowing of the
foreskin at 6 months follow-up. The final cosmetic scoring was done at
one year follow-up. A total cosmetic score of 6 (considered optimal) was
seen in 203 (91%) patients. A score of 5 was seen in 13 (5.9%), and the
remaining 7 (3.1%) had a score of less than 4. Long-term postoperative
complications in terms of recurrence of phimosis were seen in 7 (3.1%)
patients. One adolescent had problems pulling back the foreskin during
erection. None of our patients required a redo procedure and none of the
parents requested revision circumcision over a maximum of 8 years
follow-up.
Discussion
In this study, we observed that preputialplasty
provided satisfactory short-term and long-term results in children and
adolescents with symptomatic phimosis. Several other units have
performed the dorsal slit preputialplasty with transverse closure due to
its simplicity and excellent results as a day surgery procedure [8,9],
but in few patients, foreskin deformities in form of dog ears have been
noted on both sides of the suture [9].
We modified the dorsal slit preputialplasty by
incising only the fibrotic band, undermining into both lateral sides for
4-6 mm and again incising the ring through the same incision. We found
that fibrotic ring was better divided in 3 places through a small single
incision. Mobilization of the lateral space gave contour a rounded
appearance instead of dog ears. In our series, the short-term results of
limited dorsal slit preputialplasty were excellent in terms of view low
occurrence of complications of edema, hematoma, inflammation and wound
disruption apart from long-term retraction and cosmetic results.
The main limitation of our study was an observational
design with absence of any control intervention. The generalizability of
the results is likely to depend on the surgical expertise of the
treating surgeons and patients volume of the handling units.
The results of previously reported studies in
children undergoing preputialplasty showed a functional and cosmetic
satisfaction rate of 77%-97.6% [10,11]. Cuckow, et al. [9]
compared it with circumcision, and reported that preputialplasty is
associated with few complications and good functional and cosmetic
results, provided the prepuce is mobilized regularly after surgery.
This study suggests that limited dorsal slit
preputialplasty is a safe surgical procedure for phimosis in children.
It preserves the prepuce and has low complication rate, and seems to be
a suitable alternative to circumcision. Future controlled studies are
recommended with longer follow-up periods.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
•
Limited dorsal slit preputialplasty is safe, day care
surgical procedure with low complication rate.
•
It preserves the prepuce and has satisfactory cosmetic
and functional outcome.
|
References
1. Ashfield JE, Nickel KR, Siemens DR, MacNeily AE,
Nickel JC. Treatment of phimosis with topical steroids in 194 children.
J Urol. 2003;169:1106-8.
2. Wilkinson DJ, Lansdale N, Everitt LH, Marven SS,
Walker J, Shawis RN, et al. Foreskin preputioplasty and
intralesional triamcinolone: A valid alternative to circumcision for
balanitis xerotica obliterans. J Pediatr Surg. 2012;47:756-9.
3. Shahid SK. Phimosis in children. ISRN Urol.
2012;5:1-6.
4. McGregor TB, Pike JG, Leonard MP. Pathologic and
physiologic phimosis: Approach to the phimotic foreskin. Can Fam
Physician. 2007;53:445-8.
5. P Agarwal, J D’Silva, D Sharma, V Raina. Bilateral
lateral slit preputialplasty: A technique preferred over circumcision in
primary phimosis. Internet J Surg. 2008;18:1-6.
6. Singer AJ, Arora B, Dagum A, Valentine
S, Hollander JE. Development and validation of a novel scar evaluation
scale. Plast Reconstr Surg. 2007;120:1892-7.
7. Angotti R, Molinaro F, Ferrara F, Pellegrino C,
Bindi E, Fusi G, et al. Preputialplasty can be considered an
alternative to circumcision? When, how, why? Experience of Italian
centre. Gland Surg. 2018;7:228-33.
8. Pal K. Outcome of a standardized technique of
preputial preservation surgery for phimosis: A single institutional
experience. Med J DY Patil Univ. 2014;7:290-3.
9. Cuckow PM, Rix G, Mouriquand PD. Preputialplasty:
A good alternative to circumcision. J Paediatr Surg. 1994;29:561-3.
10. Fischer-Klein Ch, Rauchenwald M. Triple incision
to treat phimosis in children: An alternative to circumcision? BJU Int.
2003;92:459-62.
11. Pedersini P, Parolini F, Bulotta AL, Alberti D.
Trident preputialplasty for phimosis in childhood. J Pediatr Urol.
2017;13:278-81.
|
|
|
 |
|

