|
|
|
Indian Pediatr 2019;56: 1025-1028 |
 |
Children’s Color Trail Test for Objective
Assessment of Attention in Children with Attention Deficit
Hyperactivity Disorder: A Diagnostic Accuracy Study
|
|
Monica Juneja 1,
Harpreet Mehar2,
Smitha Sairam1,
Neha Verma2,
Rahul Jain1 and
Devendra Mishra1
From 1Department of Pediatrics; and 2Child
Development Center; Lok Nayak Hospital, Maulana Azad Medical College,
New Delhi, India.
Correspondence to: Dr Devendra Mishra, Professor,
Department of Pediatrics, Maulana Azad Medical College, New Delhi 110
002, India.
Email: [email protected]
Received: January 03, 2019;
Initial review: March 09, 2019;
Accepted: September 30, 2019.
|
|
Objective: To compare the
Children’s Color Trail Test scores in children with and without
Attention Deficit Hyperactivity Disorder to assess its diagnostic
performance in assessing attention-deficit. Methods: 50 children
with Attention Deficit Hyperactivity Disorder (diagnosed as per
Diagnostic and Statistical Manual, 5th edition) and 50 age- and
sex-matched children underwent Test 1 and Test 2 of the Children’s Color
Trail Test. A Receiver Operating Characteristics curve was constructed
for the diagnostic accuracy of Children’s Color Trail Test in Attention
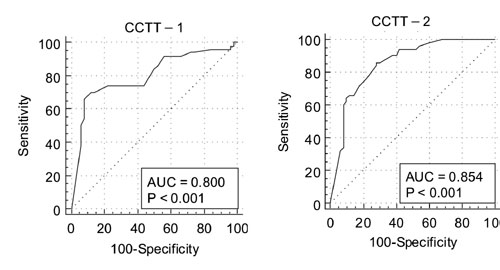
Deficit Hyperactivity Disorder. Results: The Receiver Operating
Characteristics curve showed a score
£32 for
Children’s Color Trail Test 1 [AUC: 0.8 (0.71 to 0.87); P<0.001]
and score £40
for Children’s Color Trail Test 2 [AUC: 0.85 (0.77 to 0.92); P<0.001]
as the best cut-off for diagnosing Attention Deficit Hyperactivity
Disorder. Conclusion: Children’s Color Trail Test is a promising
tool for diagnosing attention deficit, and could be used in settings
where parent or teacher reports are not available.
Keywords: Attention deficit disorders,
Diagnosis, Neurodevelopmental disorders.
|
|
T
he diagnosis of Attention deficit hyperactivity
disorder (ADHD) is typically based on the
reports of the caregivers, family members and
teachers. The criteria laid down in the Diagnostic and Statistical
Manual for Mental Disorders, 5th
edition (DSM-5) is considered the gold standard for its diagnosis [1].
In clinical settings, interview schedules like Conner’s Parent Rating
Scale (CPRS) and Conner’s Teacher Rating Scales (CTRS) [2] are often
used to elicit the symptomology, as they provide an objective score,
which can be used for assessing response to therapy [3,4]. Although
widely accepted, the assessment based on caregivers/teachers report has
many shortcomings. At times, the information may be inaccurate. The
diagnosis becomes difficult when caregivers and/or teachers are not
available, or if their reports are contradictory to each other. There is
a need for instruments that can directly assess attention and/ or level
of hyperactivity in a child.
Few computer-based tests, commonly referred to as
Continuous performance tests (CPTs) have been developed to objectively
assess the attention level of a child; however, their cost is
prohibitive [5]. Children’s Color Trail Test (CCTT) is a simple
neuropsychological test that consists of circled numbers 1-15 placed
randomly on a paper, which have to be sequenced by a performer [6]. It
objectively assesses executive functions of the brain including visual
attention, psychomotor speed, sequencing and cognitive flexibility [7].
Although, it was initially developed for use in patients with Human
immuno-deficiency virus (HIV) and traumatic brain injury, previous
studies have shown that it can differentiate children with attention
deficits, and may be helpful in monitoring their course [8]. This study
intended to assess the diagnostic performance of CCTT in assessing
attention deficit in children with ADHD, and also study the correlation
of CCTT with Conner’s rating scales.
Methods
Following approval from the Institutional Ethics
Committee, this study was carried out from June, 2014 to May, 2016 in
the pediatric outpatient department (OPD) and Child development center
of Maulana Azad Medical College, New Delhi. A sample of convenience of
100 children aged 8-15 years (50 with ADHD and 50 without ADHD) were
enrolled after obtaining informed consent from one of the parents, and
assent from the participants.
Consecutive children presenting with features
suggestive of ADHD (e.g., lack of concentration in the classroom,
poor school performance, lack of interest in studies, motor
hyperactivity, forgetfulness, poor listening responses) were assessed
for inclusion. ADHD was diagnosed by a developmental pediatrician using
the DSM-V criteria, after interviewing the child and the parents. CPRS
and CTRS were administered, and scores on various sub-scales
(inattention, hyperactivity, learning problems, executive-functioning,
aggression and peer-relationship) were obtained [2]. IQ assessment was
done using the Binet Kamat Test [9]. Age- and sex-matched controls were
enrolled from the pediatric OPD. Children with Intelligence Quotient
(IQ) <70, neurological disorders likely to affect upper limb motor
performance or compliance with directions for the test, and those who
had received any treatment for behavioral problems/ADHD were excluded.
Children’s Color Trails Test (CCTT) was administered
to all the subjects by a blinded clinical psychologist. This test has
two parts – Part 1 (CCTT1) is a page with circled numbers 1-15 placed
randomly on a paper (even numbers printed in yellow circles and odd in
pink circles). The child has to rapidly connect numbers in sequence
using a pencil. In part 2 (CCTT2) of the test, numbers from 2–15 are
presented twice, as both pink and yellow circles. The child has to
rapidly connect the numbered circles in sequence, alternating between
pink and yellow circles. CCTT takes 15-20 minutes for administration.
The examiner records the time taken to complete each trail and errors
committed, to arrive at the score of each part [6].
Statistical analysis: SPSS version 20.0 was used.
Receiver Operating Characteristics (ROC) analysis was done and Area
under curve (AUC) determined as the measure of diagnostic performance of
the test. The best cut-offs on CCTT 1 and CCTT 2 for diagnosis of ADHD
was ascertained and the sensitivity, specificity, positive predictive
value and negative predictive values were reported. Correlation between
CCTT scores and CPRS and CTRS subscale scores was evaluated using
correlation coefficient (r).
Results
The study population consisted of 100 boys (50 in
each group), with median (IQR) age of 9 (8,12) years. The parental
educational status and other socio-demographic variables in both groups
are shown in Web Table I. Of the 50 children with ADHD, 39
had combined, 10 had predominantly inattentive, and one had
predominantly hyperactive type of ADHD.
Controls had significantly higher mean scores on CCTT
1 [41.7 (7.84) vs 29.5 (10.74), P<0.001] and CCTT2 scores
[45.1 (10.17) vs 29.5 (9.99), P<0.001] as compared to
children with ADHD. The ROC analysis showed that CCTT1 has an AUC of 0.8
(95% CI, 0.71 to 0.87) and CCTT2 has an AUC of 0.85 (95% CI, 0.77 to
0.92, P<0.001) for diagnosing ADHD. A score
£32 for CCCT1 and
£40 for CCTT2
were the best cut-off values for diagnosis (Fig. 1). The
sensitivity (95% CI) and specificity (95% CI) for a DSM-5 ADHD diagnosis
was 74 (59.7-85.4) and 74 (59.7-85.4) for a CCTT-I score
£32, and 84
(70.9-92.8) and 72 (57.5-83.8) for a CCTT-2 score
£40.
 |
|
Fig. 1 ROC curves for
diagnostic performance of (a) CCTT1 and (b) CCTT2 against DSM-5
diagnosis of ADHD.
|
TABLE I Correlation of Children Color Trails Test Scores with Conners Rating Scale Scores in Children with
Attention-deficit Hyperactivity Disorder (N=50)
|
Subscale scores (CRS) |
Correlation coefficient* |
|
CCTT1 |
CCTT2 |
|
Parent Scale |
|
Inattention |
-.498 |
-.524 |
|
Hyperactivity |
-.556 |
-.596 |
|
Learning problems |
-.383 |
-.579 |
|
Executive functioning |
-.535 |
-.534 |
|
Aggression |
-.448 |
-.487 |
|
Peer relationship |
-.458 |
-.581 |
|
Teacher Scale |
|
Inattention |
-.537 |
-.476 |
|
Hyperactivity |
-.540 |
-.578 |
|
Learning/ Executive functioning |
-.531 |
-.513 |
|
Aggression |
-.477 |
-.478 |
|
Peer Relationship |
-.517 |
-.513 |
|
CRS, Connors Rating Scale; CCTT, Children’s Color Trail Test
I and II; *All P<0.001 for correlation between Conners subscale
scores and the CCTT scores. |
Table I shows the correlation of the two CCTT
tests with CPRS and CTRS scores. All Connors scores correlated
negatively with CCTT-1 and CCTT-2 scores, with correlation-coefficients
(r) in the range of –0.44 to –0.59 (P<0.001), except for
Parent-learning problems subscale, which had r= –0.38 with
CCTT-1. CCTT-1 and CCTT-2 correlated significantly with each other (r=0.637,
P<0.001).
Discussion
In this study, CCTT showed good performance against
DSM-5 criteria for diagnosing ADHD, with a sensitivity and specificity
of >72%, at cut-off score of £32
and £40 for
CCTT I and CCTT II, respectively. CCTT also showed significant
correlation with various sub-scale scores of Connor’s parent and teacher
rating scales. As CCTT is a broad screener for executive functions, it
correlated well with learning problems and executive functioning
sub-scales, in addition to the inattention subscale. The correlation
with hyperactivity and aggression sub-scale can be explained by the fact
that in most children with ADHD these behaviors often co-exist with
inattention.
There are few studies on CCTT in children with
attention problems. William, et al. [7] compared the time taken
to complete the test in children with mild neurological disorders,
learning disability, ADHD and controls. Children with ADHD took maximum
time to complete the test followed by those with mild neurological
disorder [7]. A Korean study [10] also demonstrated that CCTT scores
differ significantly between ADHD group receiving medications, ADHD-drug
free group and normal children. This study also showed good test-retest
reliability of CCTT. Seo, et al. [11] showed that CCTT has good
correlation with Comprehensive attention test (CAT) in children with
ADHD. A few studies have used CCTT as a tool to evaluate improvement in
children with ADHD, with a demonstrable change after intervention
[12,13].
Studies have attempted to derive normative values of
CCTT in different populations. It has been noted that CCTT scores is
influenced by socio-demographic variables like age, sex, socio-economic
status and ethnicity [14-16].
The major limitations of this study are the small
sample size and convenience sampling. Children with predominantly
hyperactive type were under-represented in this study, making it
impossible to compare the performance amongst different sub-types of
ADHD. Further, it would have been ideal to test the tool in a community
sample or undiagnosed children with behavioral issues.
The good diagnostic accuracy of the CCTT in this
study suggests that its role in evaluation of children with ADHD needs
to be further explored. If substantiated, it can prove to be a useful
tool in the management of ADHD. Further studies may also explore its use
to assess response to intervention (drugs and/or behavioral therapy).
Studies with larger number of children in each age-group would be
helpful in providing age-specific norms for Indian children.
Contributors: MJ,RJ,DM,SS: study planning;
SS,HM,NV; participant assessment and evaluation; HM,DM,RJ,MJ:
statistical analysis; HM,DM: manuscript writing. All authors made
important intellectual contribution to study planning, data analysis,
and manuscript writing. All authors approved the final manuscript.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
• Children’s Color Trail Test is a promising tool in the
diagnostic armamentarium for attention deficit, especially
in settings where reliable reports from parents or teachers
are not feasible.
|
References
1. American Psychiatric Association. Diagnostic and
Statistical Manual of Mental Disorders, 5th ed. Arlington: American
Psychiatric Publishing; 2013.
2. Conners CK. Clinical use of rating scales in
diagnosis and treatment of attention-deficit/ hyperactivity disorder.
Pediatr Clin North Am. 1999;46:857-70.
3. Venkata J, Panicker A. Prevalence of attention
deficit hyperactivity disorder in primary school children. Indian
J Psychiatry. 2013;55:161-4.
4. Juneja M, Sairam S, Jain R. Attention deficit
hyperactivity disorder in adolescent school children. Indian Pediatr.
2014;51:151-2.
5. Berger I, Slobodin O, Cassuto H. Usefulness and
validity of continuous performance tests in the diagnosis of
attention-deficit hyperactivity disorder children. Arch Clin
Neuropsychol. 2017;32:81-93.
6. Llorente AM, Williams J, Satz P, D’Elia LF, eds.
Children’s Color Trails Test – Professional Manual. Lutz: Psychological
Assessment Recourses; 2003.
7. Williams J, Ricket VI, Hogan J, Light R.
Children’s color trails. Arch Clin Neuropsychol. 1995;10:211-23.
8. Llorente AM, Voigt RG, Williams J, Frailey JK,
Satz P, D’Elia LF. Children’s Color trails test 1 and 2: Test-retest
reliability and factorial validity. Clin Neuropsychol. 2009;23:645-60.
9. Kamat V. Measuring Intelligence of Indian
Children. Bombay: Oxford University Press; 1967.
10. Koo H-J, Shin M-S. A standardization study of
Children’s color trails test (CCTT). Journal of Korean Academy of Child
and Adolescent Psychiatry. 2008;19:28-37.
11. Seo JM, Kim HW, Yeo JY, Byun EH, Chung S.
Executive function in attention-deficit/hyperactivity disorder:
Relationship of comprehensive attention, stoop color-word, children’s
color trails, and Wisconsin card sorting tests. J Korean
Neuropsychiatr Assoc. 2012;51:59-69.
12. Kim JK. The effects of a home-based sensorimotor
program on executive and motor functions in children with ADHD: A case
series. J Phys Ther Sci. 2018;30:1138-40.
13. Kim SH, Han DH, Lee YS, Kim BN, Cheong JH, Han
SH. Baduk (the Game of Go) Improved cognitive function and brain
activity in children with attention deficit hyperactivity disorder.
Psychiatry Investig. 2014;11:143-51.
14. Konstantopoulos K, Vogazianos V, Thodi C,
Nikopoulou-Smyrni P. A normative study of the Children’s color trails
test (CCTT) in the Cypriot population. Child Neuropsychol.
2015;21:751-8.
15. Fasfous AF, Puente AE, Pe´rez-Marfil MN,
Cruz-Quintana F, Peralta-Ramirez I, Pe´rez-Garcý´a M. Is the Color
trails culture free? Arch Clin Neuropsychol. 2013;28:743-9.
16. Arango-Lasprilla JC, Riverab D, Ramos-Usugac D,
Vergara-Moraguesd E, Montero-L´opeze E, et al. Trail Making Test:
Normative data for the Latin American Spanish-speaking pediatric
population. Neuro Rehabilitation. 2017;41:627-37.
|
|
|
 |
|

