|
|
|
Indian Pediatr 2018;55:1107-1108 |
 |
Junctional
Epidermolysis Bullosa in a Neonate
|
|
Santhiya Srinivasan, Indar Kumar Sharawat and Lokesh
Saini*
Pediatric Neurology Unit, Department of Pediatrics,
PGIMER, Chandigarh, India.
Email: [email protected]
|
|
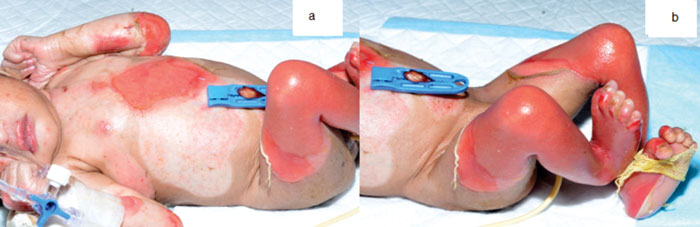
A term male newborn presented with extensive skin
peeling with multiple areas of blister formation since first day of
life. There was extensive peeling of the skin affecting about 40% of
body surface area. The oral mucosa was also involved. There were large
areas of flaccid bullae formation (Fig. 1). Initial
differentials considered were: bullous impetigo, staphylococcal scalded
skin syndrome and epidermolysis bullosa (EB). He was treated with
intravenous cefotaxime, amikacin and cloxacillin; cultures from blood
and wound were subsequently reported as sterile. The sepsis markers were
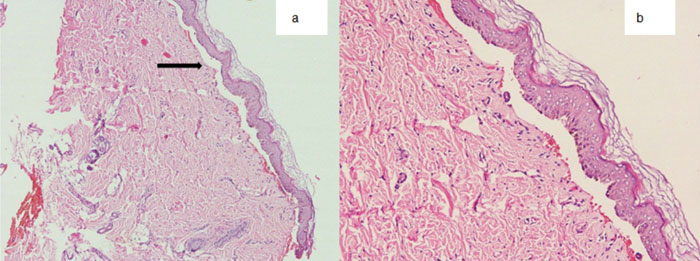
also negative. Skin biopsy revealed blister formation at dermo-epidermal
junction with no inflammatory cells in the blister, suggestive of
junctional epidermolysis bullosa (Fig. 2). Minimal
handling and daily dressing with vaseline gauze were done. Child died on
40th day of life due to extensive involvement and secondary sepsis.
 |
|
Fig. 1 Neonate showing extensive
blistering with erosions over the face, trunk and extremities.
|
 |
|
Fig. 2 Photomicrograph of skin biopsy
(haematoxylin and eosin stain: 10 X magnification) showing
clefting and blister formation at dermo-epidermal junction
(arrow) (a), with no acantholytic cells or inflammatory cells
within the blister (b).
|
The differential diagnosis for a neonate presenting
with blisters are: bullous impetigo, staphylococcal scalded skin
syndrome, epidermolysis bullosa and bullous pemphigoid. Junctional
epidermolysis bullosa (JEB) is a rare autosomal recessive disorder due
to mutations in the gene coding for Laminin 332 causing blisters in
Lamina lucida. Mechanical fragility at birth is the hallmark of the
disease characterized by extensive blistering of the skin associated
with crusting and erosions. Skin biopsy is the investigation of choice
for the suspicion of bullous disorders in the neonatal period. Light
microscopy helps to exclude the other infective bullous disorders;
immunofluorescence helps to diagnose the immune-mediated bullous
disorders. Electron microscopy helps in identifying the level of blister
formation within the dermo-epidermal junction. Finally genetic testing
helps in confirmation of the diagnosis. Treatment includes proper wound
care, prevention of secondary bacterial infections, adequate nutrition
and prevention of dehydration. This case probably had Herlitz type JEB,
presenting in neonatal period with extensive blistering and a lethal
course.
|
|
|
 |
|

