|
|
|
Indian Pediatr 2018;55:1075-1082 |
 |
Congenital
Heart Disease in India: A Status Report
|
|
Anita Saxena
From the Department of Cardiology, All India
Institute of Medical Sciences,
New Delhi 110 029, India.
Email: [email protected]
|
Considering a birth prevalence of congenital heart disease as 9/1000,
the estimated number of children born with congenital heart disease in
India is more than 200,000 per year. Of these, about one-fifth are
likely to have serious defect, requiring an intervention in the first
year of life. Currently advanced cardiac care is available to only a
minority of such children. A number of cardiac centers have been
developed over the last 10 years. However, most are in the private
sector, and are not geographically well-distributed. Challenges to
pediatric cardiac care include financial constraints, health-seeking
behavior of community, and lack of awareness. Government of India is
taking a number of steps for improving health of children through its
various program and schemes that are likely to benefit children with
congenital heart disease, especially those who are vulnerable and
marginalized.
Keywords: Epidemiology, Birth defects, Congenital heart
defects, Echocardiography.
|
|
C
ongenital heart disease (CHD) is the most
frequently occurring congenital disorder, responsible for 28% of all
congenital birth defects [1]. The birth prevalence of CHD is reported to
be 8-12/1000 live births [2,3]. Considering a rate of 9/1000, about 1.35
million babies are born with CHD each year globally [4].
With rapid advances in diagnosis and treatment of
CHD, vast majority of children born with CHD in high-income countries
reach adulthood. However, this is not the case for children born in low-
and middle-income countries (LMIC) as such advanced care is not
available for all children. Considering a birth prevalence as 9/1000,
the estimated number of children born with CHD every year in India
approximates 240,000, posing a tremendous challenge for the families,
society and health care system. This article discusses the current state
of cardiac care available to children with CHD and how it has changed
over last decade [5].
Epidemiology
The birth prevalence of severe CHD has been
consistently reported as 1.5 - 1.7/1000 live births [3,6,7]. Use of
echocardiography is associated with higher birth prevalence as many
milder cases are also detected [6-8]. Similarly, hospital-based data is
unlikely to be representative of community prevalence in LMIC where a
substantial proportion of births occur at home. Critical CHD, especially
those dependent on patency of ductus arteriosus, may go undiagnosed in
these settings.
Most studies reported from India are on prevalence at
a given point of time, and not on prevalence at birth. Many reported
studies are based on data from pediatric patients reporting to hospitals
leading to a possible sampling bias [9-14]. The profile of patients with
CHD that present to healthcare facilities in LMIC is largely determined
by the natural history of individual conditions. A high attrition of
patients with serious CHD results in low frequency of these lesions
encountered in hospital settings, and may contribute to the prevailing
perceptions on their rarity.
The true incidence or birth prevalence has been
reported only in few studies from India, which also include only babies
born in the hospital (Table I) [15-18]. In two of these
studies, echocardiography was performed for all newborns. The birth
prevalence of CHD in these studies was higher in comparison to data
available from other countries. Several other studies have reported the
prevalence of CHD during childhood, and, it varies from 1.3 to 9.2/1000
population (Table II) [19-27]. The wide variation is
partly explained by population studied and the diagnostic method used
for evaluation.
TABLE I Birth Prevalence of Congenital Heart Disease in India
|
Author [Ref.] |
No. screened |
Screening method |
No. with CHD |
Prevalence/ 1000 live births |
|
Khalil, et al. [15] |
10964 |
Clinical examination only |
43 |
3.9 |
|
Vaidyanathan, et al. [16] |
5487 |
Clinical, Pulse oximetry, |
Minor*: |
Minor CHD*:74.4 at
|
|
|
Echocardiography in all cases |
408 at birth 119 at
|
birth 21.7 at 6 weeks |
|
|
|
6 weeksMajor**:17 |
Major CHD**:3.1 |
|
Sawant, et al. [17] |
2636 |
Clinical; echocardiography in |
35 |
13.3
|
|
|
suspected cases only |
|
|
|
Saxena, et al. [18] |
20307 |
Clinical, Pulse oximetry,
|
Significant#: 164 |
Significant#: 8.1 |
|
|
Echocardiography in all cases
|
Major##: 71
Major##: 4.5/1000 |
(95% CI 6.94; 9.40)
|
|
CHD: congenital heart disease; *Those which are likely to
normalize by 6 weeks and include; atrial septal defect >5mm,
patent ductus Arteriosus >2 mm with left ventricular volume
overload, ventricular septal defect with gradient of >30 mmHg,
aortic stenosis/pulmonic stenosis with gradients of <25 mmHg and
pulmonary artery branch stenosis with gradients of <20 mmHg;
**CHD that is likely to require early intervention; #atrial
septal defect >5 mm, patent ductus arteriosus >2 mm with left
ventricle volume overload, restrictive VSD, and valvular
aortic/pulmonary stenosis with gradients <25 mmHg (in addition
to Major CHD); ##any CHD that is likely to require intervention
within the first year, including newborns with critical CHD that
require intervention within the first 4 weeks of life. |
TABLE II Prevalence of Congenital Heart Disease in Children Beyond Neonatal Age
|
Author [Ref] |
Age group
|
Setting |
Place of study |
Total No. |
Screening
|
No. with |
Prevalence |
|
(y) |
|
|
|
method |
CHD |
per 1000 |
|
Gupta, et al. 1992 [19] |
6-16 |
Community |
Jammu |
10263 |
Clinical |
8 |
0.8 |
|
Vashishtha, et al. 1993 [20] |
5-15 |
School |
Agra |
8449 |
Clinical |
44 |
5.2 |
|
Thakur, et al. 1995 [21] |
5-16
|
School |
Shimla |
15080 |
Clinical |
30 |
2.25 |
|
Chadha, et al. 2001 [22] |
<15
|
Community |
Delhi |
11833 |
Clinical |
50 |
4.2 |
|
Misra, et al. 2009 [23] |
4-18
|
School |
Eastern Uttar Pradesh |
118212 |
Clinical |
42 |
1.3
|
|
|
|
|
|
Echo for
|
|
|
|
|
|
|
|
suspected
|
|
|
|
|
|
|
|
cases only |
|
|
|
Kumari, et al. 2013 [24] |
5-16 |
School |
Dist. Prakasam,
|
4213 |
Clinical and |
39 |
9.2
|
|
|
|
Andhra Pradesh |
|
Echo in all |
|
|
|
Saxena, et al. 2013 [25] |
5-15 |
School |
Ballabgarh, Haryana |
14716 |
Clinical
|
3577 |
2.37 5.23
|
|
|
|
|
|
Clinical and
|
|
|
|
|
|
|
|
echo |
|
|
|
Bhardwaj, et al. 2016 [26] |
All age
|
Community |
Himachal Pradesh |
1882 |
Clinical |
12 |
6.312.95 |
|
groups |
|
|
(<18 y: |
Echo for
|
|
(in <18 y) |
|
19.5 y
|
|
|
660) |
suspected
|
|
|
|
|
|
|
|
cases only |
|
|
|
Nisale, et al. 2016 [27] |
1st to |
School |
Latur, Maharashtra |
3,53,761 |
Clinical |
143 |
0.4
|
|
10th class |
|
|
|
Echo for
|
|
|
|
|
|
|
|
suspected
|
|
|
|
|
|
|
|
cases only |
|
|
Current Status of Care in India
The issue of pediatric cardiac care in India has been
discussed earlier [28,29]. Gross disparity exists between high-income
countries and LMIC as far as care of children with CHD is concerned.
Whereas one cardiac center caters to a population of 120,000 in North
America, 16 million population is served by one center in Asia [30].
Similarly, the number of cardiac surgeons is also much more in North
America and Europe (one cardiac surgeon per 3.5 million population) as
compared to Asia (one cardiac surgeon per 25 million population) [3]. Of
the 240,000 children born with CHD each year in India, about one fifth
would need early intervention to survive the first year of life. A large
pool of older infants and children who may have survived despite no
intervention add to the burden of CHD.
Status of Care for Serious CHD
A number of cardiac care centers have come up in
India over the last decade. The total number approximates to 63; ten of
these can be considered high volume centers (more than 500 cardiac
surgeries per year). As per data provided by all large and medium volume
centers and a majority of small volume centers, a total of approximately
27,000 patients with CHD underwent cardiac surgery over a one-year
period (2016-2017). Of this, about 9,700 patients were infants (<1
year), and about 1700 were neonates (<1 month). Considering the birth
prevalence of serious CHD (requiring intervention in first year of life)
as 1.6/1000 live births, about 43,000 babies are born in India every
year with serious CHD, of which only about one-fourth seem to be
receiving optimal cardiac care. This proportion, though still very low,
is much better when compared with similar projections from India a
decade ago [5,31]. These data suggest that pediatric cardiac care is
gradually improving in India; although, we still have a long way to go.
Regional Variations
There is marked regional variations in the population
and crude birth rates in various parts of India. The total number of
births are much higher in Northern and Eastern parts of India (Delhi,
Jammu and Kashmir, Punjab, Haryana, Himachal Pradesh, Rajasthan, Uttar
Pradesh, Uttarakhand, Bihar, Jharkhand, Orissa and West Bengal) as
compared to rest of four regions (Southern, Western, Central and
North-East). Consequently, the total number of babies born with CHD are
likely to be much more in regions with high birth rates (Fig.
1).
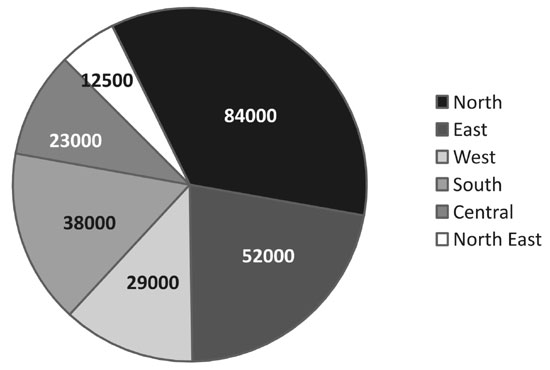 |
|
Fig. 1 Regional distribution of
infants born with CHD in India every year. (See color figure at
website)
|
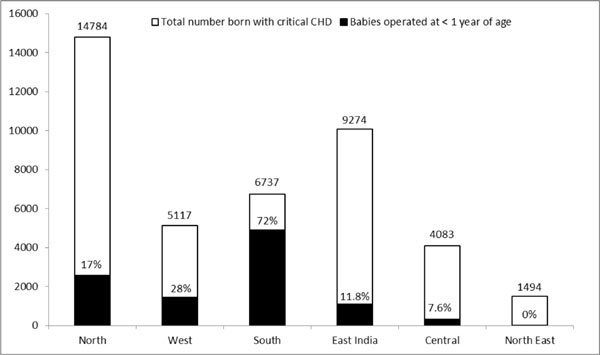
Based on the information provided by 47 centers in
India, there is a clear paradox as many centers are located in regions
with lower burden of CHD. When considering the critical CHD (requiring
intervention in first year of life), the Southern and Western states of
India have fared much better than other regions (Fig. 2).
On the contrary, states such as Uttar Pradesh, Bihar, Jharkhand and
Madhya Pradesh, which presumably have much higher CHD burden as compared
to the rest of states, have fared much worse. The data suggest that
children born with serious CHD in Southern India have a 70% chance of
receiving good cardiac care even if we consider that some of the
children operated in these centers are from other parts of India. In
contrast, babies born in Eastern and Central parts of India have a much
lower chance of receiving an intervention. This status may soon change
as the pediatric cardiac care centers start within the campuses of newly
opened government institutes (All India Institute of Medical Sciences).
These institutes are already operational in various states, including
those in eastern, central and northern parts of India. Currently, the
number of congenital heart surgeries is less in these institutes,
especially for neonates and infants.
 |
|
Fig. 2 Regional distribution of
infants with critical heart disease accessing surgery as
compared to total number born with critical heart disease.
|
Obstacles to Pediatric Cardiac Care in India
Lack of awareness and delay in diagnosis: A
substantial proportion of births in India occur at home, and the infant
is likely to die before the critical, ductus-dependent CHD is diagnosed.
Fortunately, the rate of hospital deliveries have significantly
increased due to several incentivized schemes by the Government of
India. Ductus-dependent CHD may still escape detection as babies are
often discharged earlier. Pre-discharge screening of newborns by pulse
oximetry, which may pick up these CHDs, is often not practiced,
especially in rural and semi-urban centers. Frontline health workers and
primary caregivers are not sensitized to the problem of CHD and a number
of them believe that a child with CHD is doomed and will never be able
to lead a fruitful life, even if intervened. Delay in referral results
in poor outcomes as complications and co-morbidities (such as under-
nutrition) may have already set in.
Maldistribution of resources: The resources for
treatment of CHD are not only inadequate but also seriously
mal-distributed. As mentioned earlier, the geographical distribution of
these centers is very uneven. Poverty, which is the greatest barrier to
successful treatment of CHD is more common in states with little or no
cardiac care facilities. Transport of newborns and infants with CHD is
another neglected issue in India. There is practically no organized
system for safe transport of newborns and infants with CHD. The risks of
developing hypothermia and hypoglycemia during long, unsupervised
transport further adds to the already serious condition of the infants
with CHD [32]. Limited resources and inefficient governance further
compromise a fair distribution.
Financial constraints: Medical insurance is
practically nonexistent in India, especially for birth defects. In most
instances, families are expected to pay for the treatment out of their
pocket, which they can barely afford. In a study from Kerala [33],
surgery for CHD resulted in significant financial burden for majority of
families. Approximately half of the families borrowed money during the
follow-up period after surgery [33]. Many families lose their wages as
they are away from work during care of these children. Though several
state government level programs, microfinance schemes, charitable and
philanthropic organizations exist for the benefit of economically weaker
sections of the society, awareness amongst community about such programs
is very low. The number of public hospitals which provide care at a low
cost are very few. Most cardiac centers, especially those set-up more
recently, are in the private sector and may not be affordable for the
majority. Public hospitals are faced with a very large number of
patients and have waiting lists ranging from months to years. Children
undergoing surgery are often in advanced stages of disease with
associated malnutrition [34]. The results of intervention in such
settings are expected to be less than ideal.
According to data collected from 47 centers in India,
about 35% of cardiac surgeries are funded by families themselves.
Government schemes, mostly at state level, cover about 40% of all
surgeries for CHD patients. Many hospitals partner with charitable
non-government organizations and multinational companies to assist
economically weaker families. About 20% of cardiac surgeries are funded
by such organizations. Other less common (<5%) funding sources include
parents’ employer and donations. Some of the charitable cardiac centers
are providing completely free treatments; however, such centers
generally have long waiting lists.
Health seeking behavior of the community:
Often the parents seek medical care only when child develops significant
symptoms. This may not be only due to financial constraints. Local
religious and socio-cultural practices in India affect the level of care
received by children with CHD. Illiteracy may be partly contributing to
such behavior. Gender bias, as prevalent in some societies, may put
girls at a disadvantage compared to boys. In a study from a referral
tertiary care center, girls were less likely to undergo cardiac surgery
for CHD than boys [35].
Lack of follow-up care: Most children with CHD,
including those who have undergone an intervention, require long-term
care for a good outcome. Unfortunately, a large number of children in
India, especially those from middle or lower socioeconomic strata, are
lost to follow-up. The onus of follow-up is totally on the family of the
affected child as our health system is not proactive despite having a
network of primary health care units.
Other factors: Investment on healthcare is one of
the lowest in India when compared with several other countries,
including many LMIC. There is no national policy for CHD. Rapid
population growth, competing priorities, inefficient and inadequately
equipped infrastructure, and a deficit of trained staff at all levels of
healthcare are some of the other major roadblocks to cardiac care of
children with CHD.
Strategies for Improvement of Cardiac Care
To make meaningful reductions in mortality and
morbidity from CHD, it is imperative to focus on comprehensive newborn
and infant cardiac care. However, improvements in maternal and child
health services must occur simultaneously. Health is a state subject and
the various states of India differ vastly in their economy, literacy
levels, population, languages, cultural beliefs and human development
indices. This regional diversity makes the task more difficult as ‘one
size fits all’ approach is not tenable [36].
Increasing awareness: Community needs to be
sensitized to the problem of congenital defects, through electronic and
print media. Targeting pediatricians and educating them not just about
diagnosing CHD in a newborn, but also about the advancements that have
occurred in the care of children with CHD should also be helpful.
Preventive measures and screening: So far, little
emphasis has been placed on preventive measures for CHD. This needs to
be stressed as the investment required is much smaller. Mass
immunization against Rubella should be the starting point at the
national level. Although one can have a specific preventive program for
children with CHD, a more comprehensive program which caters to the
well-being of children in general, and incorporates a number of other
common disorders is more likely to be sustainable. A flagship scheme of
Government of India (Rashtriya Bal Swasthya Karyakram, RBSK) has been
launched in February 2013 with a mandate to screen all children, aged
0-18 years for early detection and management of birth defects and other
diseases. Under this initiative, comprehensive health care is expected
to be provided for all diagnosed cases of birth defects. Periodic
education programs to sensitize the practicing physicians and
pediatricians are necessary. The frontline health workers as well
community in general should be made aware of the availability of
advanced care in India for children with CHD. Screening newborns with
pulse oximetry to diagnose critical CHD should become a part of newborn
care [37].
Geographic distribution of centers of excellence:
Establishing more centers for cardiac care would be ideal, but this is a
very challenging task. One not only needs sophisticated technology and
infrastructure, but also a motivated team of health professionals.
Pediatric cardiac care is a team effort involving cardiologists,
surgeons, anaesthesiologists and intensive care specialists. There
should be at least one center in each state unit, may be more in
populous states, so that families do not have to travel long distances
to new cities with different local environments and languages. Ideally,
these centers should be supported by the government, either directly or
through welfare schemes, so that families belonging to middle and lower
strata on socioeconomic scale can also reap the benefits. This would
also maintain a high volume of cases, leading to professional
satisfaction and motivation of the employed staff.
Optimal utilization of resources: The model of
piggybacking pediatric cardiac program on a successful ongoing adult
cardiac program is useful for optimizing resource utilization, and has
been successfully used in several hospitals. The cardiac catheterization
laboratory, operating rooms, staff and other services are shared for
both pediatric and adult patients. In such ‘adult-program first’ models,
the pediatric cardiac program is gradually expanded. However, this model
is not without problems as adult care may get preference over pediatric
care as adult program are much less resource-intense. Collection of
outcome data to assess the quality of program is very important for
self-sustainability.
In-country training of staff: Currently India has
approximately 130 pediatric cardiologists and 110 pediatric cardiac
surgeons. These numbers are grossly inadequate, but are much better than
what it was a decade ago. Given a choice, very few specialists choose
pediatric cardiology and cardiac surgery as these specialities are much
more demanding, less glamorous and provide lower monetary return.
Hand-holding of new recruits by senior staff/expatriates on short-term
deputation from established cardiac centers, is likely to improve skills
and morale of junior surgeons. With ever increasing numbers of centers,
in-country structured training programs for pediatric cardiac care
specialists are necessary as has been successfully done in some
countries [38]. In the last five years or so, some good quality training
programs have started in India, including a three year courses in
pediatric cardiology. Incorporating research into a training program is
also very important, and helps in its sustainability.
Indigenization and innovation: For cardiac
surgery and interventions to be affordable, cost-containment is
necessary. Currently, majority of equipment and disposable items
required for cardiac surgery are being imported. Encouraging home grown
technology will reduce the cost of equipment considerably. Few LMIC,
such as Brazil and Mexico, are manufacturing products locally, reducing
the costs significantly. However, high standards have to be prescribed
for local manufacturers and a strict quality control is necessary.
Prioritization of care: A contentious issue is
prioritizing CHD care for those cases which are ‘one time fixes’ with
good long-term outcome over those with complex CHD requiring multistage,
often palliative surgeries with suboptimal long-term survival. This
issue gains importance because of the enormous burden of CHD in India
and availability of limited facilities for their management. The denial
of cardiac surgery to children with complex CHD and single ventricle
physiology (e.g., heterotaxy syndromes) and to those associated
with significant extra-cardiac malformations is for efficient resource
utilization in a resource-constrained setting. Such decisions can be
challenged and are best taken in consultation with parents.
Providing financial support for treatment: A
number of financial models are supporting healthcare in India. Many of
them cater to children and cover for CHDs. Some of the private hospitals
support patients utilizing funding from corporate social responsibility
programs. Payment is sometimes linked to the patient’s capacity to pay,
helping to subsidize services for poorer patients. Charitable hospitals
often depend on donations. Insurance is another way to provide high
quality care. One of the successful schemes adopted by Karnataka, called
Yeshashwini, is a microfinance scheme where each member of a cooperative
group pays a nominal amount to create a corpus which is used to fund
surgeries [39]. Several other states have similar schemes under
different names. A number of initiatives by the central government are
directed at health of children. Provision is also provided for free
treatment of children from families which are below poverty line. In
addition, poor patients can get financial help from Prime Minister’s
Relief Fund and Chief Minister’s Relief Fund. The policy makers and
others in the government are taking note of pediatric health, and in
future, we may see more schemes for the benefit of children with CHD.
However, we must have the infrastructure to take care of this increasing
demand.
Recently government of India has launched a
National Health Protection Scheme, which is a flagship program
under Ayushman Bharat [40]. This scheme is expected to cover over 10
crore poor and vulnerable families (approximately 50 crore people).
Under this scheme, a coverage up to Rs. 500,000 per family per year will
be provided, for secondary and tertiary care hospitalization. Whether
this scheme would significantly impact the cardiac care of children with
CHD is to be seen, considering the mismatch between the high load of
cases and number of cardiac care centers in India.
Conclusion
The care available for children with CHD is vastly
different in MIC, including India, from that in high-income countries. A
large proportion of children with CHD go undiagnosed and untreated in
India due to the large numbers and limited resources. A significant
amount of progress has been made in India for the management of children
with CHD over the last three decades, but it still remains grossly
inadequate. Interactions with pediatricians and other front line health
staff are necessary to improve the overall outlook for children with
CHD. Advocacy with health policy makers is very important so that more
resources are allocated to care of children with CHD – at primary,
secondary and tertiary levels. Potential solutions to improve access to
cardiac care must consider the local social, economic and political
systems for each region. A locally relevant research must be a part of
this endeavor.
Acknowledgements: The author thanks all the
participating centers and the specialists who provided their centers’
data. A complete list is given below:
Prem Alva (AJ Hospital and Research
Centre, Mangalore), Sachin Talwar (All India Institute of Medical
Sciences, New Delhi), R Krishna Kumar (Amrita Institute of
Medical Sciences, Kochi), Muthukumaran C Sivaprakasam, Neville
A G Solomon (Apollo Children’s Hospitals, Chennai), Vikas Kohli
(Apollo Hospital, New Delhi), Nidhi Rawal, Viresh Mahajan, Aseem
R Srivastava, Pradipta K Acharya (Artemis Hospital, Sector 51,
Gurugram), Renu P Kurup (Aster MIMS Calicut), K Nageswara Rao
(Care Hospital, Hyderabad), KS Iyer (Fortis Escorts Heart
Institute and Research Centre, New Delhi), Swati Garekar (Fortis
Hospital, Mulund, Mumbai), Raghavan Subramanyan (Frontier
Lifeline Hospital, Chennai), Sumodh Kurien (G B Pant
Hospital, New Delhi), Sanjay Gandhi, Ramesh Patel (Geetanjali
Medical College & Hospital (Geetanjali Cardiac Center), Udaipur), M
Kalyanasundaram (GKNM Hospital Coimbatore), Jayakumar TK
(Govt. Medical College Kottayam), Shaad Abqari (Jawaharlal Nehru
Medical College Hospital, Aligarh Muslim University, Aligarh), Smita
Mishra (Jaypee Hospital, Sector-128, Noida), R Prem Sekar,
Karthik Surya (Kauvery Hospital Chennai), Snehal Kulkarni (Kokilaben
Ambani Hospital, Mumbai), Sudeep Verma, Gouthami V (Krishna
Institute of Medical Sciences (KIMS), Secunderabad), S Devaprasath
(Kovai Children Heart Center & Sri Ramakrishna Hospitals, Coimbatore),
Edwin Francis (Lisie Heart Institute, Kochi), K Sivakumar
(Madras Medical Mission, Chennai), Neeraj Awasthy (Max
Superspeciality Hospital, New Delhi), Amit Misri (Medanta
Medicity, Gurugram, Haryana), Anil Singhi (Medica
Hospital, Kolkata), R Saileela, Robert Coelho (MIOT centre for
Children’s Cardiac Care, Chennai), Karan Dave (Narayana Institute
of Cardiac Sciences Bangalore), Emmanuel Rupert, Debasis Das (Narayana
Superspeciality Hospital, Howrah), Prashant Mahawar (Narayana
Multi-specialty Hospital, Jaipur), Biswajit Bandyopadhyay (NH
Rabindranath Tagore International Institute of Cardiac Sciences,
Kolkata), Manoj Kumar Rohit (PGIMER Advanced Cardiac Centre,
Chandigarh), Dinesh Kumar,Vijay Gupta, Dheeraj Deo Bhatt (PGIMER
and Dr RML Hospital, New Delhi), Siddharth Gadage (Ruby Hall
Clinic, Pune), Sudeep Kumar (Sanjay Gandhi Postgraduate Institute
of Medical Sciences, Lucknow), Shivaprakash K (Sir HN Reliance
Foundation Hospital, Girgaum), Raja Joshi, Neeraj Aggarwal (Sir
Ganga Ram Hospital, New Delhi), K M Krishnamoorthy, Deepa S Kumar,
Arun Gopalakrishnan (Sree Chitra Tirunal Institute for Medical
Sciences and Technology, Trivandrum), Ashish Katewa, Balswaroop Sahu
(Sri Sathya Sai Sanjeevani Hospital, Raipur), Jayranganath M, Usha MK
(Sri Jayadeva Institute of cardiovascular Sciences and
Research, Bangalore), Anupama Rao, Krishna Manohar (Sri Sathya
Sai Institute of Higher Medical Sciences, Whitefield, Bangalore),
Saji Philip (St. Gregorios Cardio Vascular Centre, Parumala),
Nitin Rao, Ramkinkar Shastri (STAR Hospitals, Hyderabad), Srirup
Chatterjee (The Mission Hospital, Durgapur, West Bengal), Nilesh
K Oswal (UN Mehta Institute of Cardiology and Research Centre, Ahmedabad),
BRJ Kannan (Vadamalayan Hospitals, Madurai), Sumitra
Venkatesh, S S Prabhu, Biswa R Panda (Wadia Children’s Cardiac
Centre, Mumbai).
|
Key Messages
• Over 200,000 children are estimated to be
born with congenital heart disease in India every year.
• About one-fifth of these suffer from
critical heart disease requiring early intervention.
• The currently available care for these
children is grossly inadequate.
• There are over 60 centers that cater to
children with congenital heart disease; majority are in southern
states of India.
• Most of babies born with congenital heart
disease in most populous states of India, such as Uttar Pradesh
and Bihar, do not receive the care they deserve.
• Improving care of children with congenital
heart disease is an uphill task, but needs to be addressed.
|
References
1. Dolk H, Loane M, EUROCAT Steering Committee.
Congenital Heart Defect in Europe: 2000-2005. Newtownabbey, Northern
Ireland: University of Ulster; March 2009. Available from:
http://eurocat.bio-medical.co.uk/content/Special-Report.pdf.
Accessed May 18, 2017.
2. Bernier PL, Stefanescu A, Samoukovic G,
Tchervenkov CI. The challenge of congenital heart disease worldwide:
epidemiologic and demographic facts. Semin Thorac Cardiovasc Surg
Pediatr Card Surg Annu. 2010;13:26-34.
3. Hoffman JIE. The global burden of congenital heart
disease. Cardiovascular J Africa. 2013;24:141-5.
4. Hoffman JIE. Incidence of congenital heart
disease: I. Postnatal incidence. Pediatr Cardiol. 1995;16:103-13.
5. Saxena A. Congenital heart disease in India: A
status report. Indian J Pediatr. 2005;72:595-8.
6. Hoffman JI, Kaplan S. The incidence of congenital
heart disease. J Am Coll Cardiol. 2002;39:1890-900.
7. van der Linde D, Konings EM, Slager MA, Witsenburg
M, illem Helbing A, Johanna JM, et al. Birth prevalence of
congenital heart disease worldwide. A systematic review and
meta-analysis. J Am Coll Cardiol. 2011;58:2241-7.
8. Kothari SS, Gupta SK. Prevalence of congenital
heart disease. Prevalence of congenital heart disease. Indian J Pediatr.
2013;80:337-9.
9. Kapoor R, Gupta S. Prevalence of congenital heart
disease, Kanpur, India. Indian Pediatr. 2008;45:309-11.
10. Bhat NK, Dhar M, Kumar R, Patel A, Rawat A, Kalra
BP. Prevalence and pattern of congenital heart disease in Uttarakhand,
India. Indian J Pediatr. 2013;80:281-5.
11. Wanni KA, Shahzad N, Ashraf M, Ahmed K, Jan M,
Rasool S. Prevalence and spectrum of congenital heart diseases in
children. Heart India. 2014;2:76-9.
12. Kiran B, Chintan S, Reddy C, Savitha S, Medhar
SS, Keerthana TN. Study of prevalence of congenital heart diseases in
children in a rural tertiary care hospital. J Pediatr Res.
2016;3:887-90.
13. Abqari S, Gupta A, Shahab T, Rabbani MU, Ali SM,
Firdaus U. Profile and risk factors for congenital heart defects: A
study in a tertiary care hospital. Ann Pediatr Cardiol. 2016;9:216-21.
14. Mahapatra A, Sarangi R, Mahapatra PP. Spectrum of
congenital heart disease in a tertiary care centre of Eastern India. Int
J Contemp Pediatr. 2017;4:314-6.
15. Khalil A, Aggarwal R, Thirupuram S, Arora R.
Incidence of congenital heart disease among hospital live births in
India. Indian Pediatr. 1994;31:519-27.
16. Vaidyanathan B, Sathish G, Mohanan ST, Sundaram
KR, Warrier KK, Kumar RK. Clinical screening for congenital heart
disease at birth: A prospective study in a community hospital in Kerala.
Indian Pediatr. 2011;48:25-30.
17. Sawant SP, Amin AS, Bhat M. Prevalence, pattern
and outcome of congenital heart disease in Bhabha atomic research centre
hospital. Indian J Pediatr. 2013;80:286-91.
18. Saxena A, Mehta A, Sharma M, Salhan S, Kalaivani
M, Ramakrishnan S, et al. Birth prevalence of congenital heart
disease: A cross sectional observational study from North India. Ann
Pediatr Cardiol. 2016;9:205-9.
19. Gupta I, Gupta ML, Parihar A, Gupta CD.
Epidemiology of rheumatic and congenital heart disease in rural
children. J Indian Med Assoc. 1992;90:57-9.
20. Vashishtha VM, Kalra A, Kalra K, Jain VK.
Prevalence of congenital heart disease in school children. Indian
Pediatr. 1993;30:1337-40.
21. Thakur JS, Negi PC, Ahluwalia SK, Sharma R,
Bhardwaj R. Congenital heart disease among school children in Shimla
hills. Indian Heart J. 1995;47:232-5.
22. Chadha SL, Singh N, Shukla DK. Epidemiological
study of congenital heart disease. Indian J Pediatr. 2001;68:507-10.
23. Misra M, Mittal M, Verma AM, Rai R, Chandra
G, Singh DP, et al. Prevalence and pattern of congenital heart
disease in school children of eastern Uttar Pradesh. Indian Heart J.
2009;61:58-60.
24. Rama Kumari N, Bhaskara Raju I, Patnaik AN, Barik
R, Singh A, Pushpanjali A, et al. Prevalence of rheumatic and
congenital heart disease in school children of Andhra Pradesh, South
India. J Cardiovasc Dis Res. 2013;4:11-4.
25. Saxena A. Echocardiographic prevalence of
congenital cardiac malformations among 14,716 asymptomatic school
children in India. Presented at EuroEcho Imaging 2013.
26. Bhardwaj R, Kandoria A, Marwah R, Vaidya P, Singh
B, Dhiman P, et al. Prevalence of congenital heart disease in
rural population of Himachal - A population -based study. Indian Heart
J. 2016;68:48-51.
27. Nisale SH, Maske GM. A study of prevalence and
pattern of congenital heart disease and rheumatic heart disease among
school children. Int J Adv Med. 2016;3:947-51.
28. Kothari SS. Pediatric cardiac care for the
economically disadvantaged in India: Problems and prospects. Ann Ped
Cardiol. 2009;2:95-8.
29. Kumar RK. The nuts and bolts of pediatric cardiac
care for the economically challenged. Ann Ped Cardiol. 2009; 2:99-101.
30. Pezzella T. Worldwide maldistribution of access
to cardiac surgery. J Thorac Cardiovasc Surg. 2002;123:1016-17.
31. Kumar RK, Shrivastava S. Pediatric heart care in
India. Heart. 2008;94:984-90.
32. Kumar RK. Congenital heart disease profile: Four
perspectives. Ann Pediatr Cardiol. 2016;9:203-4.
33. Raj M, Paul M, Sudhakar A, Varghese AA, Haridas
AC, Kabali C, et al. Micro-economic impact of congenital heart
surgery: Results of a prospective study from a limited-resource setting.
PLoS One. 2015;10:e0131348.
34. Liu J. Challenges and progress of the pediatric
cardiac surgery in Shanghai Children’s Medical Center: A 25-year solid
collaboration with Project HOPE. Semin Thorac Cardiovasc Surg Pediatr
Card Surg Annu. 2009;12:12-8.
35. Ramakrishnan S, Khera R, Jain S, Saxena A,
Kailash S, Karthikeyan G, et al. Gender differences in the
utilisation of surgery for congenital heart disease in India. Heart.
2011; 97:1920-5.
36. Saxena A. Pediatric cardiac care in India:
Current status and the way forward. Future Cardiol. 2018;14:1-4.
37. Saxena A, Mehta A, Ramakrishnan S, Sharma M,
Salhan S, Kalaivani M, et al. Pulse oximetry as a screening tool
for detecting major congenital heart defects in Indian newborns. Arch
Dis Child Fetal Neonatal Ed. 2015;100:F416-21.
38. Pezzella AT. Cardiothoracic surgery residency
program in Shanghai, China. Ann Afr Chir Thor Cardiovasc. 2009;4:81-99.
39. Maheshwari S, Kiran VS. Cardiac care for the
economically challenged: What are the options? Ann Pediatr Cardiol.
2009;2:91-4.
40. Lahariya C. ‘Ayushman Bharat’ program and
universal health coverage in India. Indian Pediatr. 2018;55:495-506.
|
|
|
 |
|

