|
|
|
Indian Pediatr 2018;55:1066-1074 |
 |
Indian Academy of
Pediatrics (IAP) Advisory Committee on Vaccines and Immunization
Practices (ACVIP) Recommended Immunization Schedule (2018-19)
and Update on Immunization for Children Aged 0 Through 18 Years
|
|
S Balasubramanian, Abhay Shah, Harish K Pemde, Pallab
Chatterjee, S Shivananda, Vijay Kumar Guduru, Santosh Soans, Digant
Shastri and Remesh Kumar
From Advisory Committee on Vaccines and Immunization
Practices (ACVIP), Indian Academy of Pediatrics, India.
Correspondence to: Dr Harish K Pemde, Director
Professor, Department of Pediatrics, Lady Hardinge Medical College,
Kalawati Saran Childern’s Hospital, New Delhi, India.
Email: [email protected]
|
|
Justification: There is a need
to revise/review recommendations regarding existing vaccines in view of
current developments in vaccinology. Process: Advisory Committee
on Vaccines and Immunization Practices (ACVIP) of Indian Academy of
Pediatrics (IAP) reviewed the new evidence, had two meetings, and
representatives of few vaccine manufacturers also presented their data.
The recommendations were finalized unanimously. Objectives: To
revise and review the IAP recommendations for 2018-19 and issue
recommendations on existing and certain new vaccines. Recommendations.
The major changes in the IAP 2018-19 Immunization Timetable include
administration of hepatitis B vaccine within 24 hours of age, acceptance
of four doses of hepatitis B vaccine if a combination pentavalent or
hexavalent vaccine is used, administration of DTwP or DTaP in the
primary series, and complete replacement of oral polio vaccine (OPV) by
injectable polio vaccine (IPV) as early as possible. In case IPV is not
available or feasible, the child should be offered three doses of
bivalent OPV. In such cases, the child should be advised to receive two
fractional doses of IPV at a Government facility at 6 and 14 weeks or at
least one dose of intramuscular IPV, either standalone or as a
combination, at 14 weeks. The first dose of monovalent Rotavirus vaccine
(RV1) can be administered at 6 weeks and the second at 10 weeks of age
in a two-dose schedule. Any of the available rotavirus vaccine may be
administered. Inactivated influenza vaccine (either trivalent or
quadrivalent) is recommended annually to all children between 6 months
to 5 years of age. Measles-containing vaccine (MMR/MR) should be
administered after 9 months of age. Additional dose of MR vaccine may be
administered during MR campaign for children 9 months to 15 years,
irrespective of previous vaccination status. Single dose of Typhoid
conjugate vaccine (TCV) is recommended from the age of 6 months and
beyond, and can be administered with MMR vaccine if administered at 9
months. Four-dose schedule of anti-rabies vaccine for Post Exposure
Prophylaxis as recommended by World Health Organization in 2018, is
endorsed, and monoclonal rabies antibody can be administered as an
alternative to Rabies immunoglobulin for post-exposure prophylaxis.
Keywords: Guidelines, Immunity, Infections,
Prevention, Vaccination.
|
|
T
he Indian Academy of Pediatrics (IAP) Advisory
Committee on Vaccines and Immunization Practices (ACVIP) has recently
reviewed and updated the recommended immunization schedule for children
aged 0 through 18 years based on recent evidence for the vaccines
licensed in India. The process of preparing the new recommendations
consisted of review of data and literature, consultative meetings twice
(4th and 5th August 2018 at Mangalore, and 22nd and 23rd September 2018
at Chennai), taking the opinion of various National Experts and arriving
at a consensus and drafting the recommendations while taking into
consideration the existing National immunization schedule and policies
of the government. All decisions were taken unanimously and voting was
not required for any issue. The recommendations in brief along with
supporting evidence from relevant literature are presented in this
article. The detailed information will be presented later in IAP
Guidebook on Immunization. While using these guidelines, pediatricians
are free to use their discretion in a particular situation within the
suggested framework.
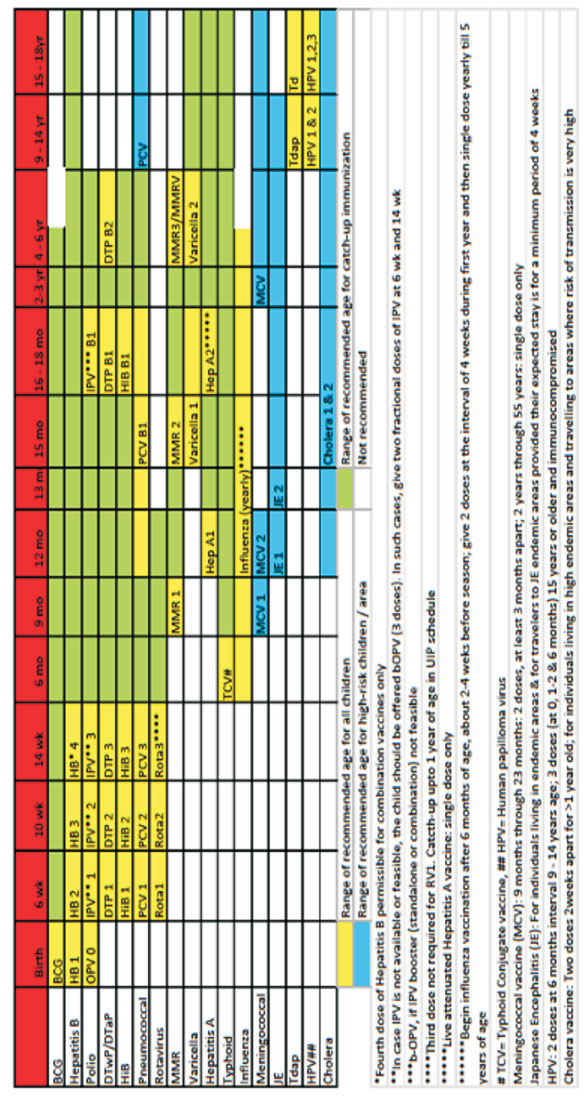
The current IAP ACVIP recommendations for the 2018-19
IAP Immunization Timetable are presented in Table I and
Fig. 1, and this also include some alterations from the
earlier recommended schedule [1].
TABLE I Key Updates and Major Changes in Recommendations for IAP Immunization Timetable, 2018-2019
|
Hepatitis B vaccine
• One dose of hepatitis B vaccine within 24 hours of birth.
• In case of use of a combination vaccines a total of four doses
of hepatitis B vaccine are justified.
DTwP, DTaP and combination vaccines
• DTwP or DTaP can be offered in primary series.
Polio vaccines
• Ideally IPV should replace OPV as early as possible.
• Three doses of intramuscular IPV in primary series is the best
option.
• Two doses of intramuscular IPV instead of three for primary
series if started at 8 weeks, with an interval of 8 weeks
between two doses is an alternative.
• In case IPV is not available or feasible, the child
should be offered three doses of bOPV. In such cases, the child
should be referred for two fractional doses of IPV at a Government
facility at 6 and 14 weeks or at least one dose of
intramuscular IPV, either standalone or as a combination vaccine,
at 14 weeks of age.
Rotavirus vaccine
• In case of Rotavirus vaccine, RV1 can be used in 6, 10 weeks
schedule.
Influenza vaccine
• Inactivated influenza vaccine (either trivalent or
quadrivalent) is recommended routinely to all children below 5
years of age starting from 6 months of age annually (2-4 weeks
before influenza season).
Measles-containing vaccines
• Measles-containing vaccine (MMR/MR) should be administered
after 9 months of age.
• MR vaccine as part of the national campaign is to be
administered irrespective of previous vaccination.
Typhoid vaccines
• Single dose of any of Typhoid conjugate vaccine (TCV 25 mg) is
recommended from 6 months onwards and can be
administered with MMR also.
• Booster dose of Typhoid conjugate vaccine not recommended in
subsequent years.
Rabies vaccines
• ACVIP IAP endorses administration of a 4-dose schedule of
Rabies vaccine recommended by WHO 2018 for Post-
exposure prophylaxis.
• ACVIP also endorses administration of Rabies monoclonal
antibody as an alternative to Rabies immunoglobulin for
category-III bites.
|
|
ACVIP: Advisory Committee on Vaccines and Immunization
Practices; IAP: Indian Academy of Pediatrics; IPV: Injectable
polio vaccine; OPV: Oral polio vaccine; bOPV: bivalent oral
polio vaccine; MR: Measles-Rubella vaccine; MMR:
Measles-Mumps-Rubella vaccine. |
 |
|
Fig. 1 IAP-ACVIP Recommended
immunization schedule for children aged 0-18 years (2018-19).
|
Hepatitis B Vaccine
The burden of chronic hepatitis B virus infection is
substantial as the coverage of the birth-dose (estimated as 39%
globally) is still low. World Health Organization (WHO) Position paper
2017 states that hepatitis B vaccine (HBV) should be administered as a
birth dose, preferably within 24 hours (timely birth dose) [2]. This
dose may only be delayed if the mother is known to be hepatitis-B
surface antigen (HBsAg) negative at the time of delivery. When the HBsAg
report of the mother is not known or reported incorrectly, or in case of
infants born to HBsAg positive mothers, this dose becomes a very
important safety net [3].
Four doses of hepatitis B vaccine may be administered
for programmatic reasons (e.g., 3 doses of hepatitis B-containing
combination vaccine or monovalent HBV after a single monovalent dose at
birth [2].
Diptheria, Tetanus and Pertussis Vaccines (DTwP and
DTaP)
Long-term efficacy over 10 years has been observed to
be superior with whole cell pertussis vaccine (wP) [4]. Recent outbreaks
of pertussis in various developed countries have sparked a debate on the
effectiveness of acellular pertussis (aP) vaccines. However, none of
these countries are planning to revert back to whole-cell pertussis
vaccines as that can result in an increase in the prevalence of the
disease due to poor acceptance of a vaccine that is much more
reactogenic [5]. Though the reasons for this resurgence are complex and
vary from place to place, the lesser duration of protection and
decreased impact on transmission of the disease by acellular pertussis
vaccines appears to be crucial [6]. Waning of immunity has been reported
with whole cell and acellular vaccines over a period of time. Current
evidence suggests that the efficacy of both aP and wP vaccines in
preventing pertussis in the first year is equivalent. After the first
year, the immunity wanes more rapidly with the aP vaccines and the
impact on transmission by aP vaccines is also inferior to wP vaccines
[7-9]. WHO clearly mentions that countries currently using the wP
vaccine in their national programs should continue the same for the
primary series [10,11], while those using the aP vaccine should continue
the same and consider additional boosters and strategies like
immunization of mothers in case of pertussis resurgence [10]. The
duration of protection for both the aP and wP vaccines after the three
primary doses and a booster dose at least after a year varies from 6-12
years [11]. A German study reported acellular pertussis vaccine being
quite efficacious (88.7%) (95% CI, 76.6% to 94.6%) [12].
Number of Components
In a couple of systematic reviews, it was concluded
that multi-component acellular pertussis vaccines are more efficacious
than the single- or two-component vaccines [13,14]. However,
effectiveness studies of long-term usage of two-component acellular
pertussis vaccines in Sweden [15] and Japan [16], and the mono-component
vaccine in Denmark showed high effectiveness in prevention of pertussis.
Thus the higher efficacy for the multi-component vaccine as demonstrated
in the trials should be cautiously interpreted, and at present the
evidence is insufficient to conclude categorically that the
effectiveness of the aP vaccines is related to the number of components
alone [10].
IAP ACVIP Recommendation on Pertussis-containing
Vaccines
The primary series should be completed with three
doses of either wP or aP vaccines, irrespective of the number of
components. wP vaccine is definitely superior to aP vaccine in terms of
immunogenicity and duration of protection but more reactogenic. In view
of parental anxiety and concerns for its reactogenicity, aP vaccine can
also be administered even in the primary series. The primary aim is to
increase the vaccination coverage with either of the vaccines.
Polio Vaccines
The elimination of circulating wild poliovirus from
our country and the decline worldwide in the number of cases is the
proof of efficacy of Oral polio vaccine (OPV). At the beginning of 2013,
126 countries using OPV exclusively, decided to introduce Injectable
polio vaccine (IPV), at least one dose, in their National Immunization
Schedule. This was part of WHO’s Endgame Plan to withdraw type-2 polio
virus and prepare for ‘the switch’ from trivalent OPV (tOPV) to bivalent
OPV (bOPV) in April 2016 [17,18]. However, IPV introduction in these
countries has increased the global IPV demand, to over 200 million in
2016 from 80 million in 2013 [17,18]. The attempt to meet the global
requirements for IPV by rapidly increasing the IPV production has led to
multiple challenges, resulting in a shortage worldwide. Intradermal IPV
administration with fractional doses of IPV (fIPV) (0.1 mL or one-fifth
of a full dose) offers potential cost reduction and allows immunization
of a larger number of persons with a given vaccine supply [19]. Two
fractional doses administered via the intradermal (ID) route
offer higher immunogenicity compared to one full intramuscular (IM) dose
of IPV [20-23]. As a result, a two-dose fIPV schedule has been strongly
recommended to countries that are endemic and the those with high risk
of importation of wild polio virus [24].
Private medical practitioners have irregular and
inadequate access to standalone IPV, and are thus compelled to
administer combination vaccines, and thus are not able to follow the
Indian government schedule, which consists of fIPV and standalone IPV.
It is not feasible for pediatricians in private settings to refer all
children to government facilities for the same. In addition, the recent
controversy of the contamination of OPV with type-2 Poliovirus has
resulted in the awareness of vaccine-derived paralytic poliomyelitis
(VDPP) amongst public. In this background, there is a need to recommend
a regimen containing IPV as combination vaccine in the private settings.
IAP ACVIP Recommendations
• Birth dose of OPV is a must.
• Extra doses of OPV on all Supplementary
immunization activities should continue.
• No child should leave the health facility
without polio immunization (IPV or OPV), if indicated by the
schedule.
• bOPV should be continued in place of IPV, only
if IPV is not feasible, with a minimum of 3 doses at 6,10,14 weeks
of age.
• Minimum age of administration of IPV is 6 weeks
with the best option being 3 doses of IM IPV in 6-10-14 weeks
schedule. This can be as a combination vaccine, in view of
non-availability of standalone IM IPV.
• Two doses of IM IPV, instead of 3 doses can be
administered provided the primary series is started at 8 weeks with
the minimum interval between them being 8 weeks.
• In case IPV is not available or feasible, the
child should be offered 3 doses of bOPV in a 6-10-14 weeks schedule.
In such cases, the child should be advised to receive two fractional
doses of IPV at a Government facility at 6 and 14 weeks of age or at
least one dose of IM IPV either standalone or as a part of
combination vaccine at 14 weeks.
Rotavirus Vaccines
A review of studies from 38 populations found that
all rotavirus gastroenteritis events (RVGE) occurred in 1%, 3%, 6%, 8%,
10%, 22% and 32% children by age 6, 9, 13, 15, 17, 26 and 32 weeks,
respectively. Mortality was mostly related to RVGE events occurring
before 32 weeks of age [25]. The highest risk of mortality was noted in
the children having earliest exposure to rotavirus, living in poor rural
households, and having lowest level of vaccine coverage [26]. It is
ideal if immunization schedule is completed early in developing
countries where natural infection might occur early [27].
Infants in developing countries may be at risk of
developing RVGE at an earlier age than those in developed countries.
They also tend to have a higher risk of mortality coupled with the risk
of lower vaccine coverage. No observational study has compared different
ages at first dose. A schedule of two doses at 10 and 14 weeks may
result in incomplete course of vaccination, especially in developing
countries because of restriction of upper age limit for rotavirus
vaccine administration. Such children would remain immunologically
susceptible to get rotavirus infection. Early administration of the
first dose of rotavirus vaccine as soon as possible after 6 weeks of age
has been recommended by WHO recently [27]. Administration of RV1 or RV5
vaccine at 6 weeks has also been recommended and approved even in
developed countries [28].
Two randomized controlled trials reported data on
severe rotavirus gastroenteritis with up to one year follow-up, and
directly compared children who received the first dose of RV1 at age 6
weeks vs 10 to 11 weeks. No statistically significant difference
in efficacy was found between these two schedules [29]. The South Africa
and Malawi RV1 trial [30] reported similar efficacy of vaccination
schedules beginning at 6 weeks or 10 to 11 weeks against severe RVGE
during the second year follow-up using only the Malawi cohort. Indirect
comparisons based on stratification of RV1 and RV5 trials using
different schedules showed no impact on mortality for different ages at
first dose.
Considering these factors, ACVIP recommends RV1 in a
schedule of 6 and 10 weeks. The recommendations for the schedule of
other vaccines remain the same.
Currently the following live oral rotavirus vaccines
are available in India: (i) Human monovalent live vaccine (RV1);
(ii) Human bovine pentavalent live vaccine (RV5); (iii)
Indian neonatal rotavirus live vaccine, 116 E; (iv) Bovine
Rotavirus Vaccine – Pentavalent (BRV-PV). BRV-PV is a recently
introduced pentavalent rotavirus vaccine that contains serotypes G1, G2,
G3, G4, and G9 obtained from Bovine (UK) X Human Rotavirus Reassortant
strains. It is a thermostable vaccine and can be stored below 24
0C till the duration of the shelf
life of 30 months. This vaccine remains stable for 36 months at
temperature below 25 0C
, for 18 months between 37 0C
and 40 0C
, and a short-term exposure at 55
0C
[31].
IAP ACVIP Recommendation on Rotavirus Vaccines
Any of the available rotavirus vaccines may be
routinely administered as per the manufacturer’s recommendations. All
the available vaccines have been demonstrated to be safe and
immunogenic.
• Minimum age: 6 weeks for all available brands
• Only two doses of RV-1 are recommended at 6 and
10 weeks
• If any dose in series was RV-5 or RV-116E or
vaccine product is unknown for any dose in the series, a total of
three doses of RV vaccine should be administered.
Recommendations on the age limit for the first dose
and the last dose (16 and 32 weeks) should continue in spite of
recommendation for increase in the age limit as per recent NIP
guidelines.
Typhoid Vaccine
Considering the continuation of significant burden of
typhoid fever, widespread prevalence of antibiotic-resistant strains of
S. typhi and availability of favorable evidence on the efficacy,
effectiveness, immunogenicity, safety, and cost-effectiveness of typhoid
vaccines, WHO recommends use of typhoid vaccines in national programs
for the control of typhoid fever [32,33]. Typhoid conjugate vaccine
(TCV) is preferred at all ages as it has improved immunological
properties, can be used in younger children, and is expected to provide
longer duration of protection. A meta-analysis summarized that typhoid
cases across the age groups; 14% to 29% in <5 years, 30% to 44% in 5-9
years and 28% to 52% in 10-14 years [34]. It has been observed that more
than one-fourth of all cases occur in children aged below 4 years, with
approximately 30% of cases in children aged below 2 years, and 10% in
children aged below 1 year [35]. Based on this, WHO has recommended TCV
for infants and children from 6 months of age as a 0.5 mL single dose
[36], and the same is endorsed by ACVIP.
Booster Doses/Revaccination
The need for revaccination with TCV is currently
unclear [36]. The protection with TCV may last for up to 5 years after
the administration of one dose, and natural boosting may occur in
endemic areas [37]. The evidence concerning the need for booster
vaccination is lacking currently. Until more data is generated or
available, the ACVIP recommends only a single dose of TCV from 6 months
onwards. If a child has received Typhoid polysachharide vaccine, it is
recommended to offer one dose of TCV at least 4 weeks following the
receipt of polysaccharide vaccine.
Currently, three products of TCV are licensed in
India. Two of them contain 25 µg of purified Vi PS of S. typhi,
and one of them containing 5 µg purified Vi PS of S. typhi. The
WHO position paper in 2018 has remarked that the body of evidence for
the 5 µg vaccine is very limited.
IAP ACVIP Recommendation on Typhoid Vaccines
Primary schedule
• A single dose of TCV 25 µg is recommended from
the age of 6 months onwards routinely.
• An interval of at least 4 weeks is not
mandatory between TCV and measles-containing vaccine when it is
offered at age of 9 months or beyond.
• For a child who has received only Typhoid
polysaccharide vaccine, a single dose of TCV is recommended at least
4 weeks following the receipt of polysaccharide vaccine. Routine
booster for TCV at 2 years is not recommended as of now.
Measles, Mumps and Rubella (MMR/MR) Vaccines
Standalone measles vaccine is now not available for
regular use. Measles-containing vaccine (MMR/MR) should be administered
after 9 months of age (270 days). MR (Measles-Rubella) vaccine is
currently not available in the private sector. Hence in view of
morbidity following mumps infection, it has been recommended that MMR is
administered instead of MR at 9 months, 15 months, and 4-6 years [38],
or as two doses at 12 to 15 months of age with the second dose between 4
to 6 years of age. [39]. Additional dose of MR vaccine during MR
campaign for children 9 months to 15 years, irrespective of previous
vaccination status is to be administered, keeping in mind the need to
support national programs.
Influenza Vaccine
A meta-analysis and systematic review evaluating
studies published between 1995 to 2010 estimated that children under 5
years of age had 90 million (95% CI 49-162 million) new influenza
episodes, 20 million (95% CI 13-32 million) cases of acute lower
respiratory infections (ALRI) where influenza was associated, and 1
million (95% CI 1-2 million) cases of severe ALRI (associated with
influenza). This resulted in 28,000-111,500 deaths attributed to
influenza, with 99% of them from developing countries [40]. Another
study estimated that globally 160,000-450,000 children below 5 years of
age die in hospitals each year due to all-cause ALRI [41].
A systematic literature review described that during
the peak rainy season, influenza accounted for 20-42% of monthly acute
medical illness hospitalizations in India [42]. This suggests that
influenza is a substantial contributor to severe respiratory illness and
hospitalization. The findings from the studies also show that influenza
circulation and influenza-associated hospitalization are major public
health concerns in India. There is poor uptake of the influenza vaccine
in India. IAP position paper on influenza in 2013 stated the while it
may not be practical to recommend routine influenza vaccination to
everyone in India, the vaccination for high-risk groups such as the
elderly, children below 5 years, medical practitioners and pregnant
women should be seriously considered [43]. Influenza incidence in
children below 5 years of age from developing countries is three times
higher than those from developed countries, with a 15-fold higher
case-fatality [41].
Health utilization surveys conducted in two rural
sites (Ballabgarh, Haryana and Vadu, Maharashtra) in 2010-2012 reported
adjusted all-age incidence rates of influenza-associated hospitalization
as 3.8-5.4 per 10,000 in Ballabgarh and 20.3-51.6 per 10,000 in Vadu
[44]. The age-specific influenza-associated hospitalization rates varied
from year to year. In 2010, these rates were highest among persons aged
<1 year, in 2011 among patients >59 years of age, and in 2012 in
children 1-4 years in Ballabhgarh. Whereas in Vadu, in 2010, these rates
were highest among persons aged 1-4 years, in 2011 in children <1 year,
and in 2012 in children 5-14 years. Influenza viruses were found
throughout the year and the peaks coincided with peaks in rain fall at
both the sites.
The Influenza Serotype-B is reported almost round the
year in India. A multi-site influenza study in India found that 27.8%
isolates were Influenza A (H1N1) virus, 29.8% were type A (H3N2), and
42.3% isolates were type B [45]. A global influenza study found that
during seasons, out of all influenza B isolates, Victoria and Yamagata
lineages predominated or co-circulated (>20% of total detections), and
this accounted for 64% and 36% of seasons respectively. The vaccine
virus mismatch was found in 25% of the seasons [46].
With the available data, there is enough reason to
believe that the magnitude of the problem is much higher in developing
countries (including India) vis-a-vis developed countries. India
lies within the northern hemisphere. Some parts of the country
experience a distinct tropical environment because of its location close
to the equator. These areas have a southern hemisphere seasonality with
almost round-the-year circulation of influenza viruses peaking during
monsoon. Northern parts of India experience another peak during winters
similar to northern hemisphere pattern. There is continuous influenza
activity across the nation, with seasonal peaks during monsoon and
winter, and an ever increasing number of influenza-like illnesses
affecting a large number of children who can transmit the disease to
their peers and adult counterparts.
In view of influenza activity round the year with
seasonal peaks, high morbidity and mortality in high-risk groups,
including children below 5 years, paucity of facilities for laboratory
diagnosis, high transmission rate, substantial socioeconomic burden,
limitations of oseltamivir, availability of moderately efficacious
vaccine, it would be justifiable to use Influenza vaccine routinely in
the high-risk group of children below age of 5 years.
Vaccine Strains
FDA recommended the following combinations for
2018-19 influenza vaccines.
• Trivalent vaccines-to have (i) an
A/Michigan/45/2015 (H1N1)pdm09-like virus, (ii) an
A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus; and (iii)
a B/Colorado/06/2017-like virus (Victoria lineage).
• Quadrivalent vaccines to contain the above
three, and a B/Phuket/3073/2013-like virus (Yamagata lineage) [47].
IAP ACVIP Recommendations
ACVIP recommends that quadrivalent/trivalent
inactivated influenza vaccine should be routinely offered annually to
all children between 6 months to 5 years of age. The latest available
influenza vaccine can be administered after 6 months of age, 2-4 weeks
prior to the influenza season: two doses at the interval of one month in
the first year, and one dose annually before the influenza season up to
5 years of age.
Rabies Vaccine
Recent data indicate that duration and number of
doses for post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP)
regimens can be shortened. ACVIP endorses the new schedule suggested by
WHO in 2018 [48].
Pre-exposure prophylaxis (Pre-EP) is recommended in
the following two situations.
• Children exposed to pets in home.
• Children identified to have a higher risk of
being bitten by dogs.
WHO recommends a "1-site vaccine administration on
days 0 and 7 for intramuscular administration" [48].
For post-exposure prophylaxis, recently the WHO [48]
has recommended a new 4-dose schedule of either of the following: (i)
1-site intramuscular administration of vaccine on days 0, 3, 7 and
between day 14-28, or (ii) 2-sites intramuscular administration
on days 0 and 1-site on days 7, 21 (intramuscular).
Rabies Human Monoclonal Antibody (RHMAB)
Access to Rabies immunoglobulin (RIG) is limited
resulting in high rabies mortality. RHMAB is a completely human IgG1
monoclonal antibody that binds to the ectodomain of the G glycoprotein
produced by recombinant technology. It has been demonstrated to
neutralize 25 different isolates of wild-type or street isolates of
rabies virus. A recent study found that it is not inferior to Human
rabies immunoglobulin (HRIG) in producing rabies virus neutralizing
antibody in 200 subjects with WHO category-III suspected rabies
exposures. The study subjects received either RMHAB or HRIG (1:1 ratio)
in wounds, and intramuscularly wherever necessary, on day-0. All these
patients also received five doses of rabies vaccine intramuscularly on
0, 3, 7, 14 and 28 days [49].
This newly introduced monoclonal antibody has emerged
as a safe and potent alternative to rabies immunoglobulin. The WHO
position paper on Rabies in 2018 has also suggested encouragement of use
of this product, if available, instead of RIG. The comparative
advantages include easy availability, standardized production quality,
possibly greater effectiveness, no requirement of animals in its
production, and less adverse events.
In view of the irregular availability and high cost
of Rabies immunoglobin (RIG), ACVIP endorses the use of RHMAB as an
alternative to RIG – human or equine – along with rabies vaccines in all
category-III bites. RHMAB is licensed in India (as Rabisheild, Serum
Institute of India; 40 IU/mL) since 2017. The recommended dose is 3.33
IU/kg body weight, preferably at the time of the first vaccine dose.
However, this may also be administered up to the 7th day after the first
dose of vaccine is given. If the calculated dose is insufficient (to
infiltrate all the wounds), it should be diluted in sterile normal
saline to get a volume that is enough to be infiltrated around all the
wounds.
Funding: None. Indian Academy of Pediatrics
provided the consultative meetings’ expenses.
Competing interest: Representatives of a few
vaccine manufacturing companies also presented their data in the
consultative meetings. None stated for authors.
Annexure I IAP Advisory Committee on Vaccines
and Immunization Practices, 2018-19
Office-bearers: Santosh Soans
(Chairperson), Digant Shastri (Co-Chairperson), S Balasubramanian
(Convener); Members: Abhay Shah, G Vijaykumar, Harish K Pemde,
Pallab Chatterjee, S Shivananda
Rapporteur: Abhay Shah
Indian Academy of Pediatrics:
Santosh Soans (President), Digant Shastri (President-Elect), Anupam
Sachdeva (Immediate Past President), Vineet K Saxena, Arup Roy, Kedar S
Malwatkar, Harmesh Singh, D Gunasingh (Vice-Presidents), Remesh Kumar
(Secretary General), Upendra S Kinjawadekar (Treasurer), Dheeraj Shah
(Editor-in-Chief, Indian Pediatrics), NC Gowrishankar (Editor-in-Chief,
Indian Journal of Practical Pediatrics), Sangeeta Yadav, Sandeep B Kadam
(Joint Secretaries)
Writing committee: S Balasubramanian, Abhay
Shah, Harish K Pemde, Pallab Chatterjee, S Shivananda, Vijay Kumar
Guduru, Santosh Soans, Digant Shastri, Remesh Kumar
References
1. Vashishtha VM, Choudhury P, Kalra A, Bose A,
Thacker N, Yewale VN, et al. Indian Academy of Pediatrics (IAP)
recommended immunization schedule for children aged 0 through 18 years –
India, 2014 and updates on immunization. Indian Pediatr.
2014;51:785-800.
2. Hepatitis B vaccines: WHO position paper – No 27,
2017, World Health Organization. Weekly epidemiological record. No 27,
2017, 92, 369-392.
3. Elizabeth D. Barnett, Give first dose of HepB
vaccine within 24 hours of birth: American Academy of Pediatrics August
28, 2017. Available from:
http://www.aappublications.org/news/2017/08/28/HepB082817. Accessed
Nov 6, 2018.
4. Cherry JD. Pertussis and Immunizations: Facts,
Myths, and Misconceptions. Available from: http://aap-ca.org/pertussis-and-immunizations-facts-myths-and-misconceptions.
Accessed November 6, 2018.
5. Munoz FM. Safer pertussis vaccines for children:
Trading efficacy for safety. Pediatrics. 2018;142:e20181036.
6. Jackson DW, Rohani P. Perplexities of pertussis:
Recent global epidemiological trends and their potential causes.
Epidemiol Infect. 2013;16:1-13.
7. Winter K, Harriman K, Zipprich J, Schechter R,
Talarico J, Watt J, et al. California pertussis epidemic, 2010. J
Pediatr. 2012;161:1091-6.
8. Centers for Disease Control and Prevention (CDC).
Pertussis epidemic—Washington, 2012. Morb Mortal Wkly Rep.
2012;61:517-22.
9. Pertussis vaccines: WHO Position Paper – August
2015 No. 35. World Health Organization. Weekly Epidemiological Record.
2015;90:433-60.
10. World Health Organization. Pertussis Vaccine
Evidence to Recommendations (WHO). Available from:
http://www.who.int/immunization/position_papers/Pertussis
GradeTable3.pdf. Accessed November 6, 2018.
11. WHO Position paper on Pertusis Vaccine, 2005.
World Health Organization. Weekly Epidemiological Record. 2005;4:29-40.
12. Schmitt HJ, von König CH, Neiss A, Bogaerts H,
Bock HL, Schulte-Wissermann H, et al. Efficacy of acellular
pertussis vaccine in early childhood after household exposure. JAMA.
1996;275:37-41.
13. Jefferson T, Rudin M, DiPietrantonj C. Systematic
review of the effects of pertussis vaccines in children. Vaccine.
2003;21:2003-14.
14. Carlsson R, Trollfors B. Control of pertussis-lessons
learnt from a 10-year surveillance programme in Sweden. Vaccine.
2009;27:5709-18.
15. Okada K, Ohashi Y, Matsuo F, Uno S, Soh M,
Nishima S. Effectiveness of an acellular pertussis vaccine in Japanese
children during a non-epidemic period: a matched case-control study.
Epidem Infection. 2009:137:124-30.
16. World Health Organization. WHO SAGE Pertussis
Working Group. Background Paper. SAGE April 2014. Available from:
http://www.who.int/immunization/sage/ meetings/2014/april/1_Pertussis_background_FINAL4_web.pdf?
ua=. Accessed November 15, 2018.
17. World Health Organization. Use of Fractional Dose
IPV in Routine Immunization Programmes: Considerations for
Decision-making. Available from: http://www.who. int/immunization/diseases/poliomyelitis/endgame_
objective2/inactivated_polio_vaccine/fIPV_considerations_
for_decision-making_April2017.pdf?ua=1. Accessed November 6, 2018.
18. Indian Academy of Pediatrics (IAP) Advisory
committee on vaccines and Immunization Practices (ACVIP), Vasishtha VM,
Choudhary J, Yadav S, Unni JC, Jog P, Kamath SS, et al.
Introduction of inactivated poliovirus vaccine in National Immunization
Program and polio endgame strategy. Indian Pediatr.
2016;53(Suppl.1):S65-9.
19. Bahl S, Verma H, Bhatnagar P, Haldar P, Satapathy
A, Arun Kumar KN, et al. Fractional-dose inactivated poliovirus
vaccine immunization campaign — Telangana State, India, June 2016. MMWR.
2016;65:859-63.
20. Resik S, Tejeda A, Mach O, Fonseca M, Diaz M,
Alemany N, et al. Immune responses after fractional doses of
inactivated poliovirus vaccine using newly developed intradermal jet
injectors: A randomized controlled trial in Cuba. Vaccine.
2015;33:307-13.
21. Clarke E, Saidu Y, Adetifa JU, Adigweme I, Hydara
MB, Bashorun AO, et al. Safety and immunogenicity of inactivated
poliovirus vaccine when given with measles-rubella combined vaccine and
yellow fever vaccine and when given via different administration routes:
A phase 4, randomised, non-inferiority trial in The Gambia. Lancet Glob
Health. 2016;4:e534-47.
22. Troy SB, Kouiavskaia D, Siik J, Kochba E, Beydoun
H, Mirochnitchenko O, et al. Comparison of the immunogenicity of
various booster doses of inactivated polio vaccine delivered
intradermally versus intramuscularly to HIV-infected adults. J Infect
Dis. 2015;15:1969-76.
23. Saleem AF, Mach O, Yousafzai MT, Khan A, Weldon
WC, Oberste MS, et al. Needle adapters for intradermal
administration of fractional dose of inactivated poliovirus vaccine:
Evaluation of immunogenicity and programmatic feasibility in Pakistan.
Vaccine. 2017;35:3209-14.
24. Polio vaccines: WHO Position Paper, March 2016.
World Health Organization. Weekly Epidemiological Record.
2016;91:145-68.
25. World Health Organization. Detailed Review Paper
on Rotavirus Vaccines (presented to the WHO Strategic Advisory Group of
Experts (SAGE) on Immunization in April 2009). Geneva, World Health
Organization, 2009. Available from:
http://www.who.int/immunization/sage/3_Detailed_Review_Paper_on_Rota_Vaccines_17_3_2009.pdf.
Accessed November 08, 2018.
26. Phua KB, Lim FS, Lau YL, Nelson EA, Huang LM,
Quak SH, et al. Rotavirus vaccine RIX4414 efficacy sustained
during the third year of life: A randomized clinical trial in an Asian
population. Vaccine. 2012;30:4552-7.
27. Rotavirus vaccines WHO Position Paper – January
2013. Weekly Epidemiological Record. 2013;88:49-64.
28. Rotavirus. In: Hamborsky J, Kroger A,
Wolfe S, eds. Centers for Disease Control and Prevention. Epidemiology
and Prevention of Vaccine-preventable Diseases. 13th ed. Washington DC:
Public Health Foundation, 2015. Available from:https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/rota.pdf.
Accessed November 15, 2018.
29. World Health Organization. Rotavirus Report,
February 2012. Rotavirus Vaccines Schedules: A Systematic Review of
Safety and Efficacy from Randomized Controlled Trials and Observational
Studies of Childhood Schedules Using RV1 and RV5 Vaccines. Available
from: http://www.who.int/immunization/ sage/meetings/2012/ april/Soares_K_et_al_
SAGE_April_rotavirus.pdf. Accessed November 08, 2018.
30. World Health Organization. Grading of Scientific
Evidence – Tables 1–4: Does RV1and RV5 induce protection against
rotavirus morbidity and mortality in young children both in low and high
mortality settings? Available from:
http://www.who.int/immunization/position_papers/rotavirus_
grad_rv1_rv5_protection. Accessed November 8, 2018.
31. Naik SP, Zade JK, Sabale RN, Pisal SS, Menon R,
Bankar SG, et al. Stability of heat stable, live attenuated
rotavirus vaccine (ROTASIIL®). Vaccine. 2017;35:2962-9.
32. World Health Organization. Background Paper on
Typhoid Vaccines for SAGE Meeting (October 2017). Available from:
http://www.who.int/immunization/sage /meetings/ 2017/october/1_Typhoid_SAGE_background_paper_
Final_v3B.pdf. Accessed November 08, 2018.
33. World Health Organization. Guidelines on The
Quality, Safety and Efficacy of Typhoid Conjugate Vaccines, 2013.
Available from:
http://www.who.int/biologicals/areas/vaccines/TYPHOID_BS2215_doc_v1.14_WEB_
VERSION. pdf. Accessed July 12, 2016.
34. Britto C, Pollard AJ, Voysey M, Blohmke CJ. An
appraisal of the clinical features of pediatric enteric fever:
Systematic review and meta-analysis of the age-stratified disease
occurrence. Clin Infect Dis. 2017;64:1604-11.
35. World Health Organization. Background Paper to
SAGE on Typhoid Policy Recommendations. 2017. Available from:
http://www.who.int/immunization/sage/meetings/2017/october/1_Typhoid_SAGE_background_paper_Final_v3B.
pdf?ua=1. Accessed November 08, 2018.
36. Typhoid vaccines: WHO Position Paper – March
2018. Weekly Epidemiological Record. 2018;93:153-72.
37. Voysey M, Pollard AJ. Sero-efficacy of
Vi-polysaccharide tetanus-toxoid typhoid conjugate vaccine (Typbar-TCV).
Clin Infect Dis. 2018;67:18-24.
38. Vashishtha VM, Yewale VN, Bansal CP, Mehta PJ.
Indian Academy of Pediatrics, Advisory Committee on Vaccines and
Immunization Practices (ACVIP). IAP perspectives on measles and rubella
elimination strategies. Indian Pediatr. 2014;51:719-22.
39. Centers for Disease Control and Prevention.
Measles, Mumps, and Rubella (MMR) Vaccination: What Everyone Should
Know. Available from:
https://www.cdc.gov/vaccines/vpd/mmr/public/index.html. Accessed
November 18, 2018.
40. Nair H, Brooks WA, Katz M, Roca A, Berkley JA,
Madhi SA, et al. Global burden of respiratory infections due to
seasonal influenza in young children: A systematic review and
meta-analysis. Lancet. 2011;378:1917-30.
41. Rudan I, Theodoratou E, Zgaga L, Nair H, Chan KY,
Tomlinson M, et al. Setting priorities for development of
emerging interventions against childhood pneumonia, meningitis and
influenza. J Glob Health. 2012;2:10304.
42. Venkatesh M, Doarn CR, Steinhoff M, Yung J.
Assessment of burden of seasonal influenza in India and consideration of
vaccination policy. Glob J Med Pub Health. 2016;5:1-10. Available from:
http://www.gjmedph.com/uploads/R1-Vo5No5.pdf. Accessed November
18, 2018.
43. Vashishtha VM, Kalra A, Choudhury P. Influenza
vaccination in India: Position Paper of Indian Academy of Pediatrics,
2013. Indian Pediatr. 2013;50:867-74.
44. Hirve S, Krishnan A, Dawood FS, Lele P, Saha S,
Rai S, et al. Incidence of influenza-associated hospitalization
in rural communities in western and northern India, 2010-2012: A
multi-site population-based study. J Infect. 2015;70: 160-70.
45. Chadha MS, Broor S, Gunasekaran P, Potdar VA,
Krishnan A, Chawla-Sarkar M, et al. Multisite virological
influenza surveillance in India: 2004-2008. Influenza Other Respir
Viruses. 2012;6:196-203.
46. Caini S, Huang QS, Ciblak MA, Kusznierz G, Owen
R, Wangchuk S, et al. Epidemiological and virological
characteristics of influenza B: results of the Global Influenza B Study.
Influen Other Respir Viruses. 2015;9:3-12.
47. Grohskopf LA, Sokolow LZ, Broder KR, Walter EB,
Fry AM, Jernigan DB. Prevention and control of seasonal influenza with
vaccines: Recommendations of the Advisory Committee on Immunization
Practices – United States, 2018-19 Influenza Season. MMWR Recomm Rep.
2018;67:1-20.
48. World Health Organization. Rabies vaccines: WHO
Position Paper, April 2018 Recommendations. Vaccine. 2018;36:5500-3.
49. Gogtay NJ, Munshi R, Ashwath Narayana DH,
Mahendra BJ, Kshirsagar V, Gunale B, et al. Comparison of a novel
human rabies monoclonal antibody to human rabies immunoglobulin for
postexposure prophylaxis: A phase 2/3, randomized, single-blind,
noninferiority, controlled study. Clin Infect Dis. 2018;66:387-95.
|
|
|
 |
|

