In the past, the development of emergency care
delivery systems was often discouraged in low- to middle-income
countries (LMICs) on grounds of cost and limited benefits [1]. Recently,
the rising burden of acute illnesses and injury, estimated to contribute
to 45% of deaths, has changed this attitude. Studies from different
parts of the world have consistently shown that children in LMICs are of
the order of three times as likely to die due to injuries as their
counterparts in high-income countries [2-4]. Studies in Bangladesh and
Iran have reported high pediatric injury rates, and in Pakistan,
injuries are the third leading cause of death in under-five children.
Most deaths occur in rural areas where emergency care is not readily
accessible [5].
There are numerous challenges in the provision of
pediatric emergency medicine even in high-income countries [6]. There
may be pediatric emergency department (PED) systems in place but their
effectiveness in meeting needs is uneven. In the US, for example, only
6% of emergency departments are resourced to the levels demanded by the
national policy statement [7-9]. Resource-poor countries, on the other
hand, suffer greatly from the disparity in provision of emergency
services to children versus adults, with some hospitals in Africa
not employing even a single pediatrician in the emergency room [6]. The
overall challenge is to develop a comprehensive program that provides
high quality, efficient and empathetic care to all children presenting
to the PED in LMICs.
Models to Improve PED Performance
Combined PED and In-patient Model
The lack of dedicated pediatric emergency care and
on-hand qualified staff is a real concern for resource-limited
healthcare settings. By implementing a combined PED and in-patient
model, there can be more efficient utilization of limited resources
dedicated to any particular service. Using such an approach with
traditional pediatric hospitalists, Krugman and colleagues were able to
demonstrate a significant improvement in throughput time from 143
minutes to 122 minutes with a concurrent rise in patient satisfaction in
the community setting. This was a change from the standard pediatric
hospitalist program consisting mainly of in-patient coverage with
partial PED coverage [10]. This also resulted in an increase in the
average billing rate of pediatric hospitalists, which could serve as an
incentive towards the adoption of this model in community hospitals and
those in LMICs lacking a dedicated PED with qualified staff. However, in
underdeveloped healthcare settings, introducing these changes will
likely require a lot of well-orchestrated interim steps because the
pediatric hospitalist model is non-existent there.
Split-flow Approach of PED Management
Another evidence-based strategy that has been
suggested is the split-flow approach to the emergency department
[11,12]. This particular approach revolves around minimizing wait times
while simultaneously administering the type of care a patient needs. In
this method, triage nurses and physicians are trained to familiarize
themselves to patient inflow stratified into categories of patients with
different care process requirements [12]. In a retrospective analysis of
over 70,000 emergency department encounters, the split-flow approach
demonstrated a 5.9% reduction, from 2.58 to 2.43 hours, in length of
stay for discharged patients [11]. Although this particular study was on
adult patients, such a model could be made flexible according to each
PED’s particular type of patient inflow. Since this model takes into
account medical personnel’s expertise in the triage area as the main
intervention, this may be a potentially cost-effective way to improve
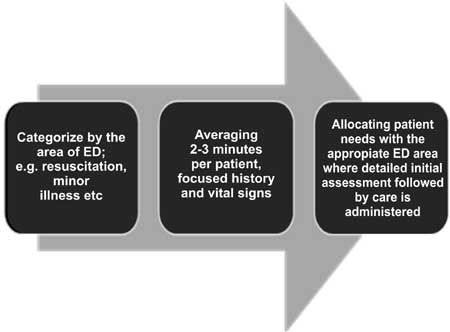
the efficiency of PEDs in LMICs (Fig. 1).
 |
|
Fig. 1 Categorizing patients based on
acuity of illness and need of resources for low- to
middle-income countries.
|
Two Tier Triage Model
Many PEDs have benefitted from a two-tier triage
where an initial triage consists of a limited information screen to
filter out patients that require urgent medical attention, followed by a
more comprehensive triage [13] (Fig. 1). Also, increasing
the number of individuals performing triage has been shown to expedite
patient-care [14]. Similarly, reducing information-gathering to certain
essential demographic factors during emergency department registration
has been shown to decrease wait times by 35% and hospital stays by a
further 10% [15]. A parallel registration process that employs data
gathering and insurance verification at the bed-side has proven to be
effective at reducing hospital stays by 10% as well [16]. This approach
may be employed in tertiary care settings of LMICs where a high volume
of patients with acute life threatening issues can be addressed prior to
a comprehensive triage and registration, albeit insurance-related time
delays are likely not of major relevance.
Fast Tracking System
Another reasonably successful strategy to hasten
patient exodus from the emergency department is the ‘fast-tracking’
system that uses triage acuity classification to distinguish critical
patients requiring urgent medical attention from patients with a less
acute presentation (Fig. 1). Low-acuity patients who had
been fast tracked out of the PED showed a significant drop in turnaround
time from 149 minutes to 107 minutes [17]. Such a system adopted for
LMICs would not only optimize use of available resources but decrease
the cost of healthcare-dispensation and unclog emergency departments in
order to make room for individuals with more pressing medical concerns.
Adjunctive Considerations
While in the emergency department, it is imperative
that the individual’s eventual disposition be decided upon as soon as
emergency care is initiated and the patient is found to be stable. To
this end, the relevant biomedical literature recommends avoidance of
interventions in the emergency department that can easily be performed
in the wards [18]. Similarly employing ancillary staff such as
interpreters and language services, and establishing a separate queue
for low acuity patients can prove to be indispensable tactics at
streamlining flow of patients in the PED [19-21].
Suggestions Towards an Efficient PED
The following PED-specific parameters need to be
considered in order to enhance PED throughput in LMICs:
1. Is there a solitary PED model that fully
accommodates the needs of LMICs or is the choice of launching a
model affected by a myriad of demographic factors?
2. How to increase the number of patients being
seen?
3. How to decrease the ‘left without being seen’
number?
4. How to decrease length of stay in the PED
without compromising quality of care by using throughput and outcome
data as surveillance tools for quality improvement?
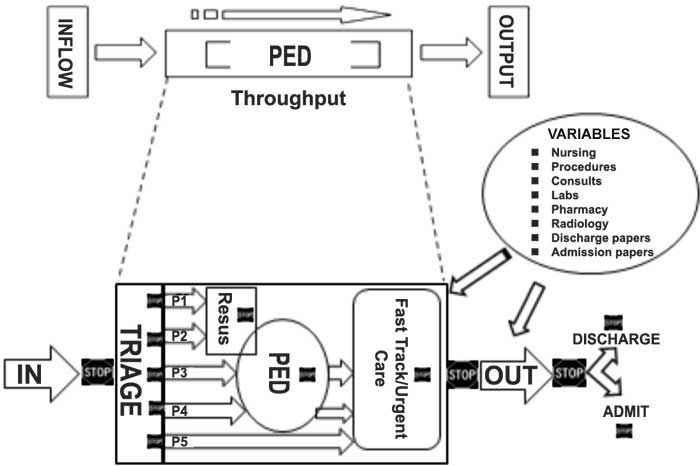
One solution may be to develop a model in which one
can match the inflow with the throughput and outflow along a continuum
of care in a flexible manner (Fig. 2). This figure
indicates potential hurdles shown as stop signs at various junctures of
the above continuum. Identifying the hurdles also paves the way to
potential solutions. What the figure also indicates is that simultaneous
interventions at various steps can potentially be more efficient and
that any model to streamline pediatric emergency medicine in LMICs might
not be very sustainable if the PED is dealt with in isolation. The
problems fall into one of three categories: systems, human resource and
communication issues. To improve efficiency without compromising
quality, the workforce can be streamlined by using PED management
protocols at each level. These though are only effective if there is a
multi-pronged approach to the PED, with stakeholders in other areas such
as pediatric surgery and allied sub-specialties. Such a systems-based
approach can utilize overlapping domains of an academic pediatric
emergency medicine program, namely, clinical service, education and
research.
 |
|
PED: Pediatric emergency department; Resus:
Resuscitation
Fig. 2 Hurdles that could impede
efficiency of pediatric emergency department at multiple levels.
Potential barriers are shown as stop signs at various junctures
along the pediatric emergency department continuum. The figure also
indicates potential solutions using a systems-based approach to
overcome some of those barriers. P1 to P5 indicate the priority
levels per the emergency severity index, with P1 being most critical
(high acuity) and P5 least critical (low acuity).
|
A number of models are being utilized for PED, but
not all of these are applicable to LMICs. Objective comparison of these
models is difficult and premature to make, as all four models have not
been experimented for similar outcomes simultaneously in a single
physical setting. However, of the approaches, one of the more
appropriate and relevant ones would be the development of a fast track
clinic and/or an urgent care center. This can be very effective to
rapidly increase the number of patients being triaged and seen,
specifically P4 and 5 (low acuity) patients per the emergency severity
index.
These models can also potentially increase individual
patient- and family-satisfaction because of the positive effect on
numbers of patients being seen; and overall better quality of care. A
separate waiting area for children with dedicated pediatric nurses
assigned to provide basic care like antipyretics and analgesics will
also factor into patient-centered compassionate care. These nurses
should have superb communication skills to help relieve undue parental
anxiety. Dedicated and adequately trained nursing staff for the
pediatric area of the emergency department, including pediatric triage,
will lead to clearly defined roles and responsibilities of the
individuals in the PED team. This becomes particularly important for
resource-limited settings. Simple distraction tools like toys may be a
worthwhile intervention to consider in improving patient-satisfaction in
high volume PEDs, like those often encountered in LMICs. Finally, early
disposition of patients in the emergency department can be facilitated
by contextually relevant evidence-based protocols for commonly
encountered problems [22].
References
1. Anderson PD, Suter RE, Mulligan T, Bodiwala G, Razzak
JA, Mock C. International Federation for Emergency Medicine (IFEM) Task
Force on Access and Availability of Emergency Care. World Health
Assembly Resolution 60.22 and its importance as a health care policy
tool for improving emergency care access and availability globally. Ann
Emerg Med. 2012;60:35-44.
2. Peden M, Oyegbite K, Ozanne-Smith J, Hyder AA,
Branche C, Rahman AKM, et al. WHO World Report on Child Injury
Prevention. Geneva: World Health Organization, UNICEF, 2008. Available
from: http://whq libdoc.who.int/publications/2008/9789241563574_eng.
pdf. Accessed June 22, 2015.
3. Deen J, Vos T, Huttly S, Tulloch J. Injuries and
non-communicable diseases: emerging health problems of children in
developing countries. Bull World Health Organ. 1999;77:518-24.
4. Bartlett SN. The problem of children’s injuries in
low-income countries: a review. Health Policy Plan. 2002; 17:1-13.
5. Razzak JA, Khan UR, Zia N, Azam I. A child
an hour: burden of injury deaths among children under 5 in Pakistan.
Arch Dis Child. 2013;98:867-71.
6. The International Federation for Emergency
Medicine: 2012 International Standards of Care for Children in Emergency
Departments. Available from: www.ifem.cc/site /DefaultSite/filesystem/documents/Policies%20and%20
Guidelines/Paeds%20standards%20full%20 document-%20final%20040912.pdf.
Accessed June 22, 2015.
7. Institute of Medicine. Committee of the Future of
Emergency Care in the U.S. Health System. Emergency Care for Children:
Growing Pains. Washington, DC: National Academy Press, 2006.
8. Middleton KR, Burt CW. Availability of Pediatric
Services and Equipment in Emergency Departments: United States, 2002-03.
U.S. Department of Health and Human Services, Centers for Disease
Control and Prevention, National Center for Health Statistics. Advance
Data. 2006;367:1-16.
9. Gausche-Hill M, Schmitz C, Lewis RJ. Pediatric
preparedness of US emergency departments: a 2003 survey. Pediatrics.
2007;120:1229-37.
10. Krugman SD, Suggs A, Photowala HY, Beck A.
Redefining the community pediatric hospitalist: the combined pediatric
ED/inpatient unit. Pediatr Emerg Care. 2007;23:33-7.
11. Arya R, Wei G, McCoy JV, Crane J, Ohman-Strickland
P, Eisenstein RM. Decreasing length of stay in the emergency department
with a split emergency severity index 3 patient flow model. Acad Emerg
Med. 2013;20:1171-9.
12. Harris M, Wood J. Resuscitate ED metrics with
split-flow design. Healthc Financ Manage. 2012;66:76-9.
13. O’Neill KA, Molczan K. Pediatric triage: A
2-tier, 5-level system in the United States. Pediatr Emerg Care.
2003;19:285-90.
14. Hoffenberg S, Hill MB, Houry D. Does sharing
process differences reduce patient length of stay in the emergency
department? Ann Emerg Med. 2001;38:533-40.
15. Chan TC, Killeen JP, Kelly D, Guss DA. Impact of
rapid entry and accelerated care at triage on reducing emergency
department patient wait times, lengths of stay, and rate of left without
being seen. Ann Emerg Med. 2005;46:491-7.
16. Gorelick MH, Yen K, Yun HJ. The effect of in-room
registration on emergency department length of stay. Ann Emerg
Med. 2005;45:128-33.
17. Simon HK, Ledbetter DA, Wright J. Societal
savings by "fast tracking" lower acuity patients in an urban pediatric
emergency department. Am J Emerg Med. 1997;15:551-4.
18. Varon J, Fromm RE Jr, Levine RL Emergency
department procedures and length of stay for critically ill medical
patients. Ann Emerg Med. 1994;23:546-9.
19. Goldman RD, Ong M, Macpherson A. Unscheduled
return visits to the pediatric emergency department – one-year
experience. Pediatr Emerg Care. 2006;22:545-9.
20. Cooke MW, Wilson S, Pearson S. The effect of a
separate stream for minor injuries on accident and emergency department
waiting times. Emerg Med J. 2002;19:28-30.
21. Rodi SW, Grau MV, Orsini CM. Evaluation of a fast
track unit: alignment of resources and demand results in improved
satisfaction and decreased length of stay for emergency department
patients. Qual Manag Health Care. 2006;15:163-70.
22. Ross MA, Hockenberry JM, Mutter R, Barrett M,
Wheatley M, Pitts SR. Protocol-driven emergency department observation
units offer savings, shorter stays, and reduced admissions. Health Aff
(Millwood). 2013;32:2149-56.

