|
|
|
Indian Pediatr 2014;51:
991-995 |
 |
Parenting in Children and Adolescents with
Psychosis
|
|
S Srivastava, *I Sharma and MS Bhatia
From Departments of Psychiatry, University College of Medical
Sciences and Guru Teg Bahadur Hospital, Delhi; and *Institute of Medical
Sciences, Banaras Hindu University, Varanasi, UP; India.
Correspondence to: Dr Shruti Srivastava, Assistant Professor,
Department of Psychiatry, University College of Medical Sciences and
Guru Teg Bahadur Hospital, Delhi 110095, India.
Email:
[email protected]
|
Need and Purpose of review: Psychotic symptoms
appear in children and adolescents in the most crucial years, during the
individual’s career development. The challenges faced by parents of
psychotic children are in dealing with their disruptive behaviours,
negative symptoms, cognitive deficits, delusions and hallucinations.
This paper presents an overview of the childhood psychosis and how
parenting can be done effectively for this population.
Methods: Articles were retrieved from the
Medline, Cochrane database, Google Scholar, Medscape; using the search
terms ‘parenting and childhood psychosis’, and ‘childhood psychoses; and
standard textbooks were consulted.
Main conclusions: Educating parents how to
recognize early symptoms, explaining treatment adherence, side effects
of medications along with non-pharmacological measures like dealing with
expressed emotions, lowering expectations, enhancing social supports,
healthy lifestyle, and making patients independent. Awareness, early
identification and effective parenting for psychosis may help bridge the
wide gap between scarce skilled mental health professionals, inefficient
resources and large paediatric population.
Keywords: Childhood psychosis, Childhood schizophrenia,
Parenting, Severe mental illness.
|
|
S
chizophrenia and other psychotic illnesses, being
the third largest cause of disability worldwide, have major public
health importance [1]. Schizophrenia disorders are rare, especially in
children. Only about 4% of total cases of schizophrenia occur in
children <15, and only 0.1-1% occur in children under the age of 10. The
rate of onset increases sharply during adolescence, with the peak ages
of onset generally ranging from 15 to 30 [2]. In a meta-analysis done by
Kelleher, et al. [3] in 2012, prevalence of psychotic symptom
among children aged 9 to 12 was found to be 17% and among adolescents
aged 13 to 18 to be 7.5% [3].
Psychosis occurring in children and adolescents
persists for long before it is brought for treatment [4].There is
considerable data to show that if treated early, course and outcome of
psychosis will be better [5]. Parents/caregivers remain unaware of the
odd behaviors/social withdrawal /delusions/hallucinations. The scenario
becomes even worse when they do not know where to contact mental health
professionals, whose number is limited. They often have to travel long
distances in order to avail mental health services. Stigma associated
with mental illnesses also acts as a deterrent for the
parents/caregivers to seek information about mental illnesses or take
advice. Thus, children and adolescents remain in the psychotic state for
several years causing considerable burden to the parents/caregivers and
society at large.
Methods
The methodology involved review of articles retrieved
on Medline (using "parenting and childhood psychosis", "parenting and
psychosis", "childhood psychosis"), Google Scholar (relevant articles),
Cochrane database, and Medscape, restricted to English language, and
standard textbooks. In addition, we searched the references given in
these articles.
Etiology/risk factors
Schizophrenia and other childhood psychosis have a
multi-factorial etiology involving genetic and environmental factors
[6]. Genetics seem to play an important role in etiology of
schizophrenia. First-degree relatives of children with schizophrenia
have a higher prevalence rate of schizophrenia and schizophrenia
spectrum disorders. Family, twin and adoption studies support that
schizophrenia has a strong genetic component.
Neurodevelopmental model of schizophrenia emphasizes
that the illness is the end stage of abnormal neuro-developmental
processes that began years before the onset of the illness [7].
Perinatal complications, alterations in brain structure and size, minor
physical anomalies, and disruption of fetal neural development,
especially during the second trimester of pregnancy, have been
correlated with the illness. Risk factors associated with childhood
psychosis include viral infections [8], childhood adversities [9],
famine [10], urban environment [11], cannabis [12], and migration [13].
Using magnetic resonance scans, Greenstein, et al.
[14] found out cortical thickness loss in childhood-onset schizophrenia
over 19-year follow up becomes localized with age to prefrontal and
temporal cortices, and the pattern of loss is more like that seen in
adult forms of the illness [14].
The neurotransmitter implicated in the patho-physiology
of schizophrenia is dopamine. Glutamate, serotonin and the N-methyl-D-aspartate
(NMDA) receptor dysfunction has also been implicated for production of
psychotic symptoms.
Early Diagnosis
Psychotic symptoms are present in children and
adolescents for extended period even before diagnosis [15]. Therefore,
it is important to recognize the prodromal symptoms for early
intervention. A follow-up study reported 35% risk of conversion to
psychosis in youth with prodromal symptoms (unusual thought content,
suspicion/paranoia, perceptual anomalies, grandiosity, and disorganized
communi-cation) [16]. The study found that the five features assessed at
baseline that contributed uniquely to the prediction of psychosis are
genetic risk for schizophrenia with recent deterioration in functioning,
higher levels of unusual thought content, higher levels of
suspicion/paranoia, greater social impairment, and a history of
substance abuse.
The symptomatology of childhood psychosis differs
from that in adults [17]. Symptoms frequently reported in psychotic
children are: speech disturbances, inability to distinguish dreams from
reality, visual and auditory hallucinations, vivid and bizarre thoughts
and ideas, diminished interest, confused thinking, extreme moodiness,
odd behavior, stereotypy, dis-inheriting ideas that others are out to
get them, confusion of television with reality, severe problems in
making and keeping friends. Hallucinations and delusions have typically
been viewed as symptoms of psychosis [18]. Cognitive deficits are
reported in childhood psychosis similar to adults, which include
deficits in attention, learning and abstraction [19].
For diagnosing schizophrenia, DSM-5 criteria lays
down that two (or more) out of the following should be present during a
one-month period (or less if successfully treated) (a) delusions
(b) hallucinations, (c) disorganized speech, (d)
grossly disorganized or catatonic behavior, and (e) negative
symptoms. It should further qualify for Symptoms either a, b or c must
be present out of the two to make diagnosis of Schizophrenia. Continuous
signs of disturbance must persist for at least 6 months, which includes
both periods of prodromal and residual symptoms. Attenuated psychosis
syndrome is included in the appendix for future research [20].
Challenges Faced by Parents of Childhood Psychosis
Taking care of a psychotic child is a challenging
task for the family members, especially parents. Parental support during
ongoing treatment predicts the prognosis of the psychotic illness in
children. Direct support provided by the mental health professionals to
the family members through information sharing, and indirect support
provided by the other family members and support groups is found to have
positive associations with family members‘experience of care-giving.
Care-giving gains in the form of becoming more sensitive to persons with
disabilities, and improving relationships with the patients should be
emphasized [21].
Faulty communication patterns have been described in
families of psychotic patients. Communication deviance that compromises
the development and sharing of meaning between the parent and the
offspring and leading to the consequent breakdown in communication has
long been suggested as a potential risk factor for the development of
psychosis [22]. The expressed emotion which includes criticism,
hostility and emotional over-involvement is considered to be an adverse
family environment. High degrees of expressed emotions is linked to the
relapse of the illness and puts the patient in stress [23].
Treatment
Antipsychotics are used in the treatment of children
and adolescents suffering from psychosis. No antipsychotic is superior
to other in terms of efficacy. The chance of relapse is high if the
medication is stopped one to two year following relapse. Routine
monitoring of the following parameters have been recommended like
weight, height, waist and hip circumference, pulse, blood pressure,
fasting blood glucose levels, glycosylated hemoglobin, blood lipid
profile, prolactin levels, movement disorders, diet, nutrition, physical
activity, side-effects, adherence, and efficacy. Treatment-resistant
schizophrenia in children and adolescents requires clozapine [24].
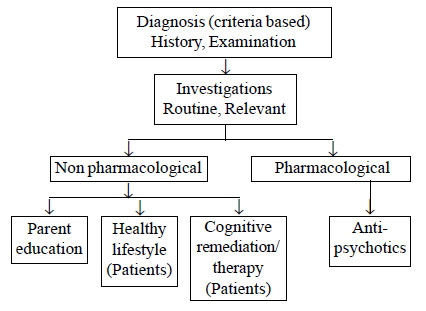
Fig.1 shows an algorithm for the management of children and
adolescents suffering from psychosis.
 |
|
Fig. 1 Management of children and
adolescents suffering from psychosis.
|
Both pharmacological and non-pharmacological
interventions are required for effective and early treatment of children
and adolescents. Early treatment is of paramount importance.
Antipsychotics are very useful in the treatment of psychosis. After the
acute symptoms of psychosis subside with these medications, the child
may benefit from counseling and psychosocial interventions.
The following non-pharmacological interventions have
been found to be efficacious [25].
Cognitive remediation (CR): It aims to arrest or
reverse the cognitive impairments in attention, concentration and
working memory. A combination of ‘procedural’ and ‘effortless learning’,
‘targeted reinforcement’ and massed practiced appears to facilitate
cognitive flexibility and memory in patients with schizophrenia [26].
Parents are advised to break down information and tasks into small
manageable parts to reduce demands on working memory.
Cognitive Behavior therapy (CBT): The therapeutic
techniques used for patients with psychosis are based on the general
principles of CBT. Links are established between thoughts, feelings, and
actions in a collaborative and accepting atmosphere. Agendas are set and
used but are generally more flexibly developed than in traditional CBT.
What is Needed?
Children and adolescents constitute 40% of the
population of India. First and foremost is the need to ease access to
care. Appropriate care and necessary information should be available at
the doorstep of the service users. For this, an infrastructure of proper
referral and care system should be in place. The proposed model of care
involving interventions at primary, secondary and tertiary levels are
required for our country in the following way:
Primary level: Following professionals can
provide care at the primary level. There is evidence to suggest the
involvement of Non specialist health workers in bridging the gap between
the scarcity of trained psychiatrists and limited resources for low and
middle income countries [27].
Health professionals can provide following services
at primary level:
• Create awareness about psychosis.
• Removing myths and misconceptions about mental
illness in general and psychosis in particular.
• Awareness about pre-morbid indicators of
psychosis.
• Psycho-education about psychosis.
• Early Identification and distribution of parent
education materials.
• Referral to higher center for timely treatment
after early identification.
District level
• Psychiatrists (under District Mental Health
Program) trained in the early diagnosis/ treatment.
• Availability of Generic psycho tropics which
are distributed free of cost.
• Referral to tertiary care center in case of
Severe Mental Disorder which requires specialty management in a
mental health Institute.
Tertiary level: Multidisciplinary teams of mental
health professionals for early identification and intervention as
already exist in all teaching hospitals should be further strengthened
like other Asian countries e.g., Singapore [28]. Allocation of
funds to improve the quality and standards of research on psychosis
should be allocated.
Guidelines for Parents
Having a child or an adolescent with psychosis is a
difficult situation and a life-long challenge. Parents who are the
primary caregivers most of the time feel overwhelmed and unprepared for
facing this situation. It is thus of paramount importance that parent
education material should be made available in the local languages (Box
I).
Box 1: Guidelines for Parents of Children and Adolescents Suffering From Psychosis
|
• |
Psychosis is a severe form of mental disorder in which contact
with the reality is lost. It is associated with abnormalities
and oddities of behavior, where children just do not seem like
themselves. |
|
• |
What causes it?
|
|
It is multifactorial involving genes, infections, cannabis,
stress, neurotransmitters etc.
|
|
• |
How do we (parents/caregivers) recognize it?
|
|
It may begin with changes in behavior like social withdrawal,
decline in school performance. The child may have active
symptoms like he/she may hear or see something which is
perceived in the absence of stimulus or may develop false, fixed
belief that “people want to harm me’’. Deterioration in previous
functioning with disturbance in sleep and appetite.
|
|
• |
What is the treatment?
|
|
Antipsychotic drugs are the mainstay of treatment. Several
non-pharmacological measures are also useful. Early treatment is
of paramount importance; adherence to treatment is
essential. |
|
• |
What can we do?
|
|
Reduce expressed emotions like criticism, hostility and
over-involvement. Encourage-ment, praise for desired behaviors,
increase social support, inculcate hobbies, reduce burden of
studies thereby minimize stress, try to make them independent. |
|
• |
What is the future of my child?
|
|
With long term treatment, full recovery is possible. With timely
help, many youth grow up to lead healthy, productive lives. |
The key point to remember is that psychosis and
schizophrenia occurring in children and adolescents have poor outcome
[29].The best way to minimize its impact is early identification and
treatment. While relapses may occur from time to time, the effects of a
psychotic episode are decreased if symptoms are identified within the
first six months of onset. There is research evidence to suggest better
course and outcome of schizophrenia in developing countries as compared
to developed countries [30].
High levels of parental involvement (parental
understanding of their children’s problems, and parental knowledge of
their children’s free-time activities) is associated with decreased
outcome of poor mental health in India’s Nationally representative
global survey done on 6721 school going adolescents in 2007
[31].Traditionally, in India, the responsibility of care and protection
of children is provided by the families and the communities. Both the
prevention and promotion of child mental health in a country with low
socio-economic status can be achieved by supporting parenting [32].
Authoritative parenting and parental warmth, especially in Indian
families, are the most adaptive parenting styles that act as protective
factors for the development of psychopathology and positive adjustment
among adolescents [33]. Health education of parents and parental
counseling play a key role in early intervention and promotion of
positive mental health of children and adolescents [34].
Conclusions
Child and adolescent mental health services are
hardly available in a low income country like India. The need for the
hour is to strengthen the mental health services through innovative
strategies that are cost-effective. Awareness, early identification and
effective parenting of pediatric psychosis may help bridge the wide gap
that exists between scarce skilled mental health professionals,
inefficient resources, and large population of children and adolescents
in developing countries.
Contributors: SS: literature search, designed and
prepared the initial draft; IS: conceived, designed, revised the draft;
MSB: designed, revised the draft. All authors approved the final
version. All authors agree to be accountable for all aspects of the
work.
Funding: None; Competing interests: None
stated.
References
1. World Health Organization (WHO). World Health
Report 2001. Mental Health: New Understanding, New Hope. Geneva: WHO;
2002.
2. Remschmidt HE, Schulz E, Martin M, Warnke A, Trott
GE. Childhood onset schizophrenia: History of the concept and recent
study. Schizophr Bull. 1994;20:727-45.
3. Kelleher I, Connor D, Clarke MC, Devlin N, Harley
M, Cannon M. Prevalence of psychotic symptoms in childhood and
adolescence: a systematic review and meta-analysis of population-based
studies. Psychol Med. 2012;42:1857-63.
4. Dominguez MD, Fisher HL, Major B, Chisholm B,
Rahaman N, Joyce J , et al. Duration of untreated psychosis in
adolescents: Ethnic differences and clinical profiles. Schizophr Res.
2013;150:526-32.
5. Amminger GP, Henry LP, Harrigan SM, Harris MG,
Alvarez-Jimenez M, Herrman H, et al. Outcome in early-onset
schizophrenia revisited: findings from the Early Psychosis Prevention
and Intervention Centre long-term follow-up study. Schizophr Res.
2011;131:112-9.
6. Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan
K, Tarrant J, et al. Heterogeneity in incidence rates of
schizophrenia and other psychotic syndromes: findings from the 3-center
AeSOP study. Arch Gen Psychiatry. 2006;63:250-8.
7. RapoportJL, Giedd JN, Gogtay N. Neurodevelopmental
model of schizophrenia: update 2012. Mol Psychiatry. 2012;17:1228-38.
8. Rantakallio P, Jones P, Moring J,Von Wendt L.
Association between central nervous system infections during childhood
and adult onset schizophrenia and other psychoses: a 28-year follow-up.
Int J Epidemiol. 1997;26:837-43.
9. Varese F, Smeets F, Drukker M, Lieverse R,
Lataster T, Viechtbauer W, et al. Childhood adversities increase
the risk of psychosis: a meta-analysis of patient-control,
prospective-and cross-sectional cohort studies. Schizophr Bull.
2012;38:661-71.
10. Xu MQ, Sun WS, Liu BX, Feng GY, Yu L,Yang L,
et al. Prenatal malnutrition and adult schizophrenia: further
evidence from the 1959-1961 Chinese famine. Schizophr Bull.
2009;35:568-76.
11. Van Os J, Hanssen M, Bijl RV, Vollebergh W.
Prevalence of psychotic disorder and community level of psychotic
symptom. Arch Gen Psychiatry. 2001;58:663-8.
12. Arseneault L, Cannon M, Poulton R, Murray R,
Caspi A, Moffitt TE. Cannabis use in adolescence and risk for adult
psychosis: longitudinal prospective study. BMJ. 2002;325:1212-3.
13. Veling W. Ethnic minority position and risk for
psychotic disorders. Curr Opin Psychiatry. 2013;26:166-71.
14. Greenstein D, Lerch J, Shaw P, Clasen L, Giedd J,
Gochman P, et al. Childhood onset schizophrenia: cortical brain
abnormalities as young adults. J Child Psychol Psychiatry.
2006;47:1003-12.
15. Sikich L. Diagnosis and evaluation of
hallucinations and other psychotic symptoms in children and adolescents.
Child Adolesc Psychiatr Clin N Am. 2013;22:655-73.
16. Cannon TD, Cadenhead K, Cornblatt B, Woods SW,
Addington J, Walker E, et al. Prediction of psychosis in youth at
high clinical risk: a multisite longitudinal study in North America.
Arch Gen Psychiatry. 2008;65:28-37.
17. Tolbert HA. Psychoses in children and
adolescents: a review. J Clin Psychiatry. 1996; 57 (Suppl 3):4-8;46-7.
18. Polanczyk G, Moffitt TE, Arseneault L, Cannon M,
Ambler A, Keefe RS, et al. Etiological and clinical features of
childhood psychotic symptoms: results from a birth cohort. Arch Gen
Psychiatry. 2010; 67:328-38.
19. Courvoisie H, Labellarte MJ, Riddle MA. Psychosis
in children: diagnosis and treatment. Dialogues Clin Neurosci.
2001;3:79-92.
20. American Psychiatric Association (APA).
Diagnostic and Statistical Manual of Mental Disorders, 5th ed. DSM-5.
Arlington, VA: American Psychiatric Association; 2013.
21. Chen FP, Greenberg JS. A positive aspect of
caregiving: the influence of social support on caregiving gains for
family members of relatives with schizophrenia. Community Ment Health J.
2004;40:423-35.
22. de Sousa P, Varese F, Sellwood W, Bentall RP.
Parental communication and psychosis: A meta-analysis. Schizophr Bull.
2014;40:756-68.
23. Hooley, JM. Expressed emotion and relapse of
psychopathology. Annu Rev Clin Psychol. 2007;3: 329-52.
24. Kranzler HN, Cohen SD. Psychopharmacologic
treatment of psychosis in children and adolescents: efficacy and
management. Child Adolesc Psychiatr Clin N Am. 2013;22:727-44.
25. Schimmelmann BG, Schmidt SJ, Carbon M, Correll
CU. Treatment of adolescents with early-onset schizophrenia spectrum
disorders: in search of a rational, evidence-informed approach. Curr
Opin Psychiatry. 2013;26:219-30.
26. Wykes T, Reeder C, Corner J,Williams C, Everitt
B. The effects of neurocognitive remediation on executive processing
inpatients with schizophrenia. Schizophr Bull. 1999;25:291-7.
27. van Ginneken N, Tharyan P, Lewin S, Rao GN, Romeo
R, Patel V. Non-specialist health worker interventions for mental health
care in low-and middle-income countries. Cochrane Database Syst
Rev.2011; CD009149.
28. Verma S, Poon LY, Subramaniam M, Abdin E,Chong
SA. The Singapore Early Psychosis Intervention Programme (EPIP): A
programme evaluation. Asian J Psychiatr. 2012;5:63-7.
29. Deakin J, Lennox B. Psychotic symptoms in young
people warrant urgent referral. Practitioner. 2013;257:25-8.
30. Kulhara P, Shah R, Grover S.Is the course and
outcome of schizophrenia better in the ‘developing ‘world?Asian J
Psychiatry. 2009;2:55-62.
31. Hasumi T, Ahsan F, Couper CM, Aguayo JL, Jacobsen
KH. Parental involvement and mental well-being of Indian adolescents.
Indian Pediatr. 2012;49:915-8.
32. Shastri PC. Promotion and prevention in child
mental health. Indian J Psychiatry. 2009;51:88-95.
33. Patel V, Flisher AJ, Nikapota A, Malhotra S.
Promoting child and adolescent mental health in low and middle income
countries. J Child Psychol Psychiatry. 2008; 49:313-34.
34. Shrivastava SR, Shrivastava PS, Ramasamy J.
Childhood and adolescence:Challenges in mental health. J Can Acad Child
Adolesc Psychiatry. 2013;22:84-5.
|
|
|
 |
|

