|
|
|
Indian Pediatr 2010;47: 1063-1065 |
 |
Overlap Syndrome: Autoimmune Sclerosing
Cholangitis |
|
Arpita Thakker and Sunil Karande
From Department of Pediatrics, Lokmanya Tilak Municipal
Medical College and General Hospital, Sion,
Mumbai 400 022, India.
Correspondence to: Dr Arpita Thakker, Developmental and
Epilepsy Clinic, Department of Pediatrics, Lokmanya Tilak Municipal
Medical College and General Hospital, Sion, Mumbai 400 022, India.
Email: arpitathakker@gmail.com
Received: April 6, 2009;
Initial review: April 20, 2009;
Accepted: August 11, 2009.
|
A 9-year-old-girl presented with clinical features of autoimmune
hepatitis and associated signs of cholestasis in the form of itching and
elevated levels of serum alkaline phosphatase. There was histologic
evidence of bile duct injury. Hence a clinical diagnosis of "overlap
syndrome" of autoimmune hepatitis with primary sclerosing cholangitis
was considered.
Key words: Cholangitis, Cholestasis, Child.
|
|
Overlap syndromes are autoimmune conditions
with mixed immunological, clinical and histological features. They include
combinations of autoimmune hepatitis (AIH) and primary biliary cirrhosis (PBC),
primary sclerosing cholangitis (PSC), or chronic viral hepatitis(1). There
are a few reports of AIH and PSC from India(2,3). We report a 9-year-old
girl with autoimmune sclerosing cholangitis, an overlap syndrome of AIH
and PSC.
Case Report
A 9-year-old girl presented with history of fluctuating
jaundice for 1 year. Each episode of jaundice lasted for a duration of 20
days. She also had itching, fever, fatigue and arthralgia. Clinical
examination revealed a malnourished child (weight of 17.4 kg and height of
116 cm, both were below 5th percentile for her age) with
hepatosplenomegaly. The liver was palpable 5 cm below the right costal
margin and was firm, nodular with a span of 9.5 cm. The spleen was
palpable 6 cm below the left costal margin and was firm. There was no
clinical evidence of ascites. Abdominal veins were prominent but were not
tortuous. There were no other stigmata of chronic liver disease.
Ophthalmologic examination for KF rings with a slit lamp was normal.
The child’s complete hemogram revealed pancytopenia
with a Hb of 6 g/dL, WBC 2.2×10 3/µL
and platelets 88×103/µL. Her serum alkaline phoshatase (970 U/L) was
markedly elevated and serum bilirubin (2.1 mg/dL) and transaminases (SGOT
116 U/L, SGPT 73 U/L) were mildly elevated. There was
hypergammaglobulinemia (gamma globulins of 65.6% of the total), decreased
serum albumin (1.8 g/dL) and prolonged prothrombin time (31.6 s; control
14 s). The gamma glutamyl transpeptidase levels were minimally raised (66
U/L). HBsAg and anti-HCV antibody were negative. Antinuclear antibody was
positive at a titer of >1:80.The serum ceruloplasmin level and urinary
copper levels were normal.
Abdominal ultrasound examination showed coarse hepatic
echotexture with nodularity, splenomegaly and ascites. Upper GI endoscopy
revealed minimal erosive gastritis without any varices. Barium meal follow
through showed no evidence of ulcerative colitis. A percutaneous liver
biopsy yielded a small fragmented piece of tissue which, histologically
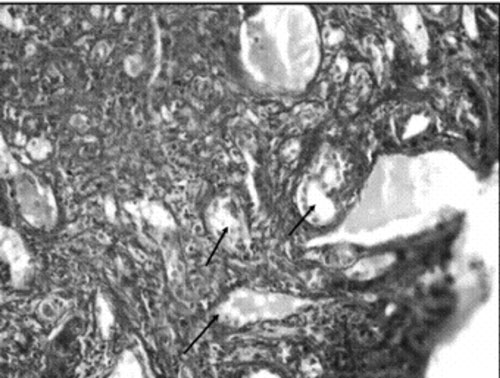
showed proliferation of bile ductules (Fig. 1), interface
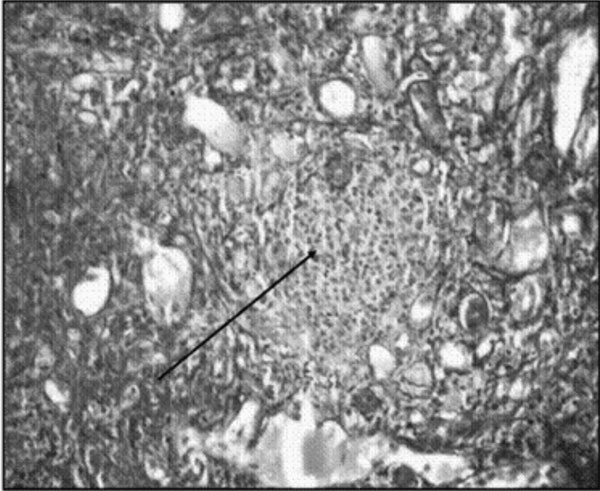
hepatitis (Fig. 2) and marked cholestasis. MRCP was normal
and ruled out large duct PSC. A diagnosis of an overlap syndrome of small
duct PSC with AIH (autoimmune sclerosing cholangitis) was made.
 |
|
Fig. 1 Liver biopsy specimen (hematoxylin
and eosin x200) revealing bile ductular proliferation (compatible
with primary sclerosing cholangitis). |
 |
|
Fig. 2 Liver biopsy specimen (hematoxylin
and eosin x 200) revealing plasma cells infiltrate (compatible with
autoimmune hepatitis). |
The child was given supportive treatment for
decompensated liver disease. Corticosteroids could not be started due to
neutropenia. Empirical treatment with ursodeoxycholic acid (15mg/kg/day)
was started in view of marked cholestatic symptoms and continued for
duration of three months. Regular follow up was advised to monitor the
clinical response and improvement in liver function tests.
On follow up after 6 weeks, oral corticosteroids were
started in the dose of 2mg/kg/day for duration of 4-6 weeks. Colonoscopy
was done which showed no evidence of inflammatory bowel disease. To assess
the severity of the disease, perinuclear Antineutrophil Cytoplasmic
Antibody (pANCA) was done which was negative.
Discussion
Autoimmune hepatitis (AIH), an unresolving inflammation
of the liver of unknown cause(4,5),
may present in atypical forms that lack established criteria, official
nomenclature and standard treatment(1). Such patients have features
associated with both AIH and another type of chronic liver disease
‘overlap syndromes’ or have findings that are incompatible with the
diagnosis of AIH according to the criteria codified by the international
panels ‘outlier syndromes’. Overlap syndromes include combinations of AIH
and PBC, or PSC, or chronic viral hepatitis(1). In our patient the
diagnosis of an overlap syndrome of AIH with PSC, also called Autoimmune
Sclerosing Cholangitis (ASC) was made(6). This syndrome has been reported
only in 6 to 8% of children, adolescents, and young adults(7).
In patients with AIH, the most common findings that
suggest an overlap variant are features asso-ciated with cholestasis and
histologic findings of bile duct injury(8).
Our patient had cholestatic changes i.e. itching and atypical elevation of
serum alkaline phosphatase. Also there was bile duct proliferation with
cholestasis on histology suggestive of bile duct injury.
In such patients, further assessment with
cholangiography should be considered to confirm the diagnosis of PSC(1).
Cholangiographic changes associated with PSC, however, are absent in 14%
of patients with typical histologic disease(9). This discordance suggest
that overlap syndrome can involve only the intrahepatic bile ducts (
small-duct PSC) as in our case(9,10).
Treatment strategies are empirical in all instances,
but they must be logical and carefully monitored(1). In an overlap of
AIH-PSC, corticosteroids should be started (prednisone 2mg/kg/day) if
autoimmune symptoms are predominant. Patients who do not respond to
corticosteroids are candidates for investigational protocols, treatment of
symptoms, or empirical therapy with ursodeoxycholic acid (13-15mg/kg/day),
if cholestatic symptoms are marked(1).
Alterations in treatment are dictated by the changes in the predominant
character of the disease and by the adequacy of the patient’s response.
Liver transplantation is required for children who progress to biliary
cirrhosis and hepatic decompensation.
In conclusion, a child presenting with features of
autoimmune hepatitis such as hypergamma-globulinemia or autoantibodies in
the serum and associated signs of cholestasis i.e. itching or elevated
levels of serum alkaline phosphatase and histologic evidence of bile duct
injury, should be considered to have a clinical diagnosis of "overlap
syndrome" of autoimmune hepatitis with primary sclerosing cholangitis and
appropriate investigations should be initiated to confirm the diagnosis.
Acknowledgment
We thank our Dean, Dr Sandhya Kamath, for granting us
permission to publish this case report.
Contributors: Both authors were involved in the
management and diagnosis of the patient, literature review, and drafting
of the manuscript.
Funding: None
Competing interest: None.
References
1. Czaja AJ. The variant forms of autoimmune hepatitis.
Ann Intern Med 1996; 125: 588-598.
2. Kochhar R, Goenka MK, Das K, Nagi B, Bhasin DK,
Chawla YK, et al. Primary sclerosing cholangitis: an experience
from India. J Gastroenterol Hepatol 1996;11: 429-433.
3. Yachha SK, Sharma BC, Khanduri A, Srivastava A.
Current spectrum of hepatobiliary disorders in northern India. Indian
Pediatr 1997; 34: 885-890.
4. Czaja AJ. Autoimmune hepatitis: evolving concepts
and treatment strategies. Dig Dis Sci 1996; 40: 435-456.
5. Johnson PJ, McFarlane IG. Meeting Report:
International Autoimmune Hepatitis Group. Hepatology 1993; 18:998-1005.
6. Gregorio GV, Meil-Vergani G. Autoimmune liver
disease in childhood. Indian J Gastroenterol 1997; 16: 60-63.
7. Rust C, Beuers U. Overlap syndromes among autoimmune
liver disease. World J Gastroenterol 2008; 14: 3368-3373.
8. Boberg KM, Fausa O, Haaland T, Holter E, Mellobye OJ,
Spurkland A, et al. Features of autoimmune hepatitis in primary
sclerosing cholangitis: an evaluation of 114 primary sclerosing
cholangitis patients according to a scoring system for diagnosis of
autoimmune hepatitis. Hepatology 1996; 23: 1369-1376.
9. Perdigoto R, Carpenter HA, Czaja AJ. Frequency and
significance of chronic ulcerative colitis in severe
corticosteroid-treated autoimmune hepatitis. J Hepatol 1992; 14: 325-331.
10. Wee A, Ludwig J. Pericholangitis in ulcerative
colitis: primary sclerosing cholangitis of the small bile ducts? Ann
Intern Med 1985; 102: 581-587.
11. Kaplan GG, Laupland KB, Butzner D, Urbanski SJ, Lee
SS .The burden of large and small duct primary sclerosing
cholangitis in adults and children: a population-based analysis. Am
J Gastroenterol 2007; 102: 1042-1049.
12. Roberts EA. Primary sclerosing cholangitis in children. J
Gastroenterol Hepatol 1999; 14: 588-593.
|
|
|
 |
|

