Naegleria fowleri is a rare cause of
meningoencephalitis in humans. It is capable of producing a fatal
fulminant primary amebic meningoencephalitis, which usually results in
death in 5-10 days(1). Very few patients are reported to survive after
acquiring this infection(2,3). We report a rare case of an 8 month old
infant who survived Naegleria meningoencephalitis.
Case Report
An 8-month old male baby weighing 6 kg presented with
high grade fever for 4 days, one episode of convulsion and altered
sensorium. There was history of giving bath in pond water many times in
last 1 month. On admission, the child was febrile with tachycardia and
tachypnea. Anterior fontanel was level and patient had mild pallor.
Glasgow coma scale was 8 and there was generalized hypertonia without any
neurological deficits. Pupils were normal and there was no cranial nerve
palsy. Liver was palpable 4 cm below the costal margin and the spleen was
palpable 2 cm below the costal margin. A provisional diagnosis of pyogenic
meningitis was made, a lumbar puncture was done and the patient was
started on antibiotics along with intravenous fluids and supportive
therapy. Investigations revealed: hemoglobin 8g/dL, total leukocyte count
12,800/mm3 with 58% neutrophils and 37% lymphocytes,
platelet count 3.8lacs/mm3, serum sodium 133.8 meq/L
and serum potassium 3.4 meq/L. Urine examination was normal, and renal and
liver functions were normal. The cerebrospinal fluid (CSF) examination
showed a sugar of 109.8 mg/dL, protein of 63.9 mg/dL with a cell count of
50 cells/mm3 (90% lymphocytes and 10% poly-morphs).
Gram stain and culture of the CSF did not reveal any bacteria. An India
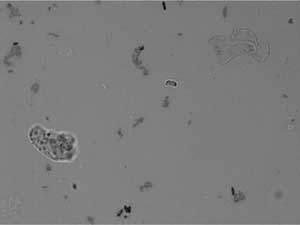
ink preparation was made to look for fungus which incidentally showed
flagellate form of the motile Naegleria fowleri (Fig.1).
The child was started on amphotericin B (1.5mg/kg/day) and intravenous
chloramphenicol (100mg/kg/day) and oral rifampicin (20mg/kg/day) from day
2 of admission. The patient’s sensorium gradually improved and he became
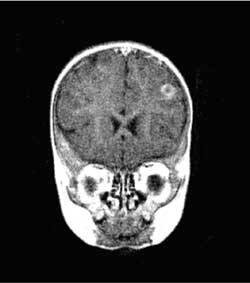
afebrile and fully conscious by day 7. MRI revealed a small focal well
defined rounded lesion (9mm) in the left frontal lobe with peripheral
hypointense rim and central hyperintensity (Fig.2). There
was also a focal ill defined T2 hyperintense lesion
seen in the left cerebellar hemisphere. Treatment was continued for 21
days and the patient was discharged. The patient came for follow up and
was well 2 months after discharge.
 |
 |
|
Fig. 1 Motile form of Naegleria fowleri
in cerebrospinal fluid.
|
Fig. 2 MRI Brain showing well-defined
lesion with a peripheral hypointense rim and cental hyperintensity. |
Discussion
Many free living small ameba like Naegleria fowleri,
Acanthamoeba and Balamuthia are capable of causing disease in
humans. They infect the central nervous system and cause 2 types of
infections. One is the more acute form which is almost universally fatal
and occurs in previously healthy individual. This form is known as PAME
and is caused by Naegleria. The other form is a more chronic form
known as chronic granulomatous amebic meningo-encephalitis. This is caused
by Acanthameba and balamuthia(4). These free living amebas
can be found in natural bodies of water and usually there is history of
bathing in a river or a pond.
The incubation period of PAME is 5-15 days. The
clinical picture is similar to that of pyogenic meningitis. Routine
laboratory tests are not helpful in distinguishing it from other causes of
meningo-encephalitis. The cerebrospinal fluid shows raised proteins,
normal or decreased glucose, pleocytosis with high count of white as well
as red blood cells. Naegleria can be identified on a wet mount
examination of the CSF by its morphology and motility(5). PAME caused by
Naegleria is a medical emergency. Only few patients have survived
till date. Early diagnosis and treatment may have played a role in their
survival. Several drugs like amphotericin B, miconazole, and rifampicin
have been used(6). Amphotericin B at a dose of 1-1.5mg/kg/day alone or in
combination with miconazole, rifampicin, and sulpha drugs may be used(7).
Contributors: RR was involved in concept, design
and drafting of manuscript and will act as a guarantor. DKS was involved
in analysis and interpretation of data. AKS and AB were involved in
revising of manuscript and final approval.
Funding: None.
Competing Interest: None stated.
References
1. Seidel JS. Naegleria, Acanthamoeba, and
Balamuthia. In: Feigin RD, Demmler GJ, Cherry JD, Kaplan SL, eds.
Textbook of Pediatric Infectious Diseases. 5th ed. Pennsylvania: Saunders:
2004. p. 2748-2755.
2. Jain R, Prabhakar S, Modi M, Bhatia R, Sehgal R.
Naegleria meningitis: a rare survival. Neurol India 2002; 50: 470-472.
3. Brown RL. Successful treatment of primary amebic
meningoencephalitis (PAM). Arch Intern Med 1991; 151: 1201-1202.
4. Martinez AJ. Free living amoebas: Infection of the
central nervous system. Mt Sinai J Med 1993; 60: 271-278.
5. Poungvarin N, Jariya P. The fifth nonlethal case of
primary amoebic meningoencephalitis. J Med Assoc Thai 1991; 74: 112-115.
6. Carter RF. Sensitivity to amphotericin B of a
Naegleria species isolated from a case of primary amebic
meningoencephalitis. J Clin Pathol 1969; 22: 470-474.
7. Loschiavo F, Ventura-Spagnolo T, Sessa E, Bramanti P. Acute primary
meningoencephalitis from entamoeba Naegleria fowleri: Report of a
clinical case with a favourable outcome. Acta Neurol (Napoli) 1993; 15:
333-340.

