Acute hemorrhagic edema of infancy (AHEI) is a benign,
small vessel vasculitis of young children with characteristic skin
findings. The cutaneous findings are dramatic, both in appearance and
rapidity of onset; histopathology is characterized by leukocytoclastic
vasculitis(LCV). Since 1913, when AHEI was first reported, only about 100
case reports have appeared in the literature(1). The condition is also
described as Finkelstein’s disease(2), or Seidlmayer syndrome.
Case Report
This 18 month old girl presented with features of viral
upper respiratory tract infection for 4-5 days followed by edema starting
from feet and progressing to all four limbs. The patient also showed
erythematous palpable spots, first on the lower limbs that progressed to
the upper limbs, face and ears and were absent from the trunk (Fig.
1). The patient was receiving an unidentified oral antibiotic,
which was administered after the onset of rash and edema. There was no
history of pain abdomen, irritability, hematuria, refusal to feed or
recent vaccination. There was no history of similar illness in the family.
On examination, the child was active and playful with stable vitals and
mild fever; the blood pressure was normal. Skin examination showed
erythmatous, palpable, pupuric lesions over the legs, gluteal region,
upper limbs, face and ears varying in size from 0.5 to 4 cm in diameter.
There was edema of upper and lower limbs; no tenderness was elicited.
Systemic examination was normal. During hospital stay, there were multiple
crops of these purpuric lesions. Investigations showed normal blood counts
and blood levels of urea, creatinine and electrolytes; urinalysis was
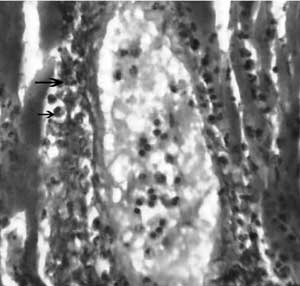
normal. Blood culture was sterile and chest x-ray was normal. Skin biopsy,
on day 3 of admission, showed mild hyperkeratosis with spongiosis in
epidermis. Dermis showed edema and periadenexal inflam-matory infiltrate.
Small blood vessels showed focal neutrophilic infiltrate and concentric
thickening of thin walls, with nuclear dust and fibrinoid changes; the
features were compatible with the diagnosis of leukocytoclastic vasculitis
(Fig.2). Immuno-fluorescence study was not done. The patient
was given symptomatic treatment and recovered within 10 days.
 |
 |
|
Fig.1 Typical erythematous, papular and
target like skin lesions characteristic of AHEI. Note the presence
of edema over both the legs.
|
Fig.2 Photomicrograph showing thickened
vessel wall with infiltration by neutrophils. Note the presence of
nuclear dust. (H&E; 400X) |
Discussion
Krause, et al.(3) reported a series of 5
patients and proposed clinical criteria for the diagnosis of AHEI as: age
less than two years, purpuric or ecchymotic target like lesions with edema
on the face, auricles and extremities with or without mucosal involvement,
lack of systemic disease and visceral involvement, spontaneous recovery
within few days or weeks(3). Our case fulfills all
above criteria along with consistent findings of skin biopsy.
On histopathological examination of skin, small blood
vessels in the dermis show perivascular neutrophilic infiltrate with
numerous scattered nuclear fragments called nuclear dust.
Histopathological findings in Henoch Schonlein purpura are similar to
AHEI. However, IgA deposition is seen in only 10-35% cases of AHEI.
Immunofluroscence studies have shown deposition of fibrinogen, C3, IgA,
IgG, IgM, IgE in and around small blood vessels.
AHEI is an uncommon disease. This may reflect either a
low incidence or underdiagnosis. Other reason for its rarity could be that
it is considered to be a variant of Henoch Schonlein purpura with only
skin involvement(4). There are few case reports from India as well(5,6).
The etiology of AHEI is not very clear. Poyrazoglu, et al.(7).
reported that 6 of 8 patients had history of recent infection, drug
administration or immunization.
Common differential diagnosis of AHEI include Henoch
Schonlein purpura, meningococcemia, erythema multiforme, urticaria with
hemorrhagic elements and drug eruptions. All these entities are not
difficult to differentiate from AHEI clinically. Spontaneous recovery
usually occurs within 1-3 weeks, without sequelae. Recurrent episodes may
occur. On follow up at one year, our patient did not have any recurrence.
Contributors: KM, RK, MR and SK were involved in
management of the patient. RK and MR reviewed the literature and prepared
the manuscript.
Funding: None.
Competing Interest: None stated.
References
1. Suehiro RM, Soares BS, Eisencraft AP, Campos LM,
Silva CA. Acute hemorrhagic edema of childhood. Turk J Pediatr 2007; 49:
189-192.
2. Morrison RR, Saulsbury FT. Acute hemorrhagic edema
of infancy associated with pneumococcal bacteremia. Pediatr Infect Dis J
1999; 18: 832-833.
3. Krause I, Lazarov A, Rachmel A, Grunwald MM, Metzker
A, Garty BZ, et al. Acute hemorrhagic edema of infancy, a benign
variant of leucocytoclastic vasculitis. Acta Pediatr 1996; 85:114-117.
4. Dubin BA, Bronson DM, Eug AM. Acute hemorrhagic
edema of childhood: an unusual variant of leukocytoclastic vasculitis. J
Am Acad Dermatol 1990; 23: 347-350.
5. Shah D, Goraya JS, Poddar B, Parmar VR. Acute
infantile hemorrhagic edema and Henoch Schonlein purpura overlap in a
child. Pediatr Dermatol 2002; 19: 92-93.
6. Kaur S, Thami GP. Urticarial vasculitis in infancy.
Indian J Dermatol Venereol Leprol 2003; 69: 223-224.
7. Poyrazoglu H M, Per H, Gunduz Z, Du sunsel R, Arslan D, Narin N,
et al. Acute hemorrhagic edema of infancy. Pediatr Int 2003; 45:
697-700.

