|
|
|
Indian Pediatr 2021;58: 775-779 |
 |
Competency-Based Assessment in Pediatrics for the
New Undergraduate Curriculum
|
|
Piyush Gupta, 1
Dheeraj Shah,1 Tejinder
Singh2
From Department of Pediatrics, 1University College of
Medical Sciences, Delhi; and 2Departments of Pediatrics and Medical
Education, SGRD Institute of Medical Sciences and Research, Amritsar,
Punjab.
Correspondence to: Prof Piyush Gupta, Professor and
Head, Department of Pediatrics, University College of Medical Sciences
(University of Delhi), Dilshad Garden, Delhi 110 095.
Email:
[email protected]
Published online: April 20, 2021;
PII: S097475591600315
|
|
Medical Council of India (MCI)
implemented competency-based curriculum for undergraduate medical
education nationwide in 2019, with assessment of competencies being its
integral component. The curriculum has outlined some broad principles
and components of assessment, but the process and schedule for formative
and summative assessment is to be decided by the universities and
institutions. In this document, we summarize the recommendations for the
subject of Pediatrics, and propose an assessment model for summative
assessment that can be adapted/adopted by universities and institutions.
Few basic principles of formative assessment have been shared, the
implementation of which may be the main challenge for the institutions.
It is important to develop the capacity of the faculty for conducting
the assessment under the ambit of principles of competency-based
curriculum.
Keywords: CBME, Curriculum, Medical education,
University examinations.
|
|
T
he Medical Council of India (MCI) has recently
introduced competency-based curriculum for undergraduate medical
education [1]. Robust assessment process is a vital part of its
implementation as this curriculum is outcome oriented (acquisition of
competencies) rather than process oriented. Competencies are defined as
habitual and consistent use of knowledge, skills, attitudes and
commu-nication related to a clinical problem [2]. A perusal of this
definition indicates that competency-based assessment cannot be a
one-time process or a year-end examination; rather it has to span over a
period of time to assess if the student is using them ‘habitually and
consistently.’ The MCI guidelines have rightly emphasized the role of
formative and internal assessment in acquisition and development of
competencies. We present an overview of assessment guidelines for the
subject of pediatrics by erstwhile MCI and propose a model for
competency-based assessment. We have refrained from any critique of
these guidelines. Both internal and summative assessments must be
planned and implemented by respective universities and/or colleges, with
few variations. The underpinning concepts of competency-based assessment
have earlier been described in detail [3].
INTERNAL ASSESSMENT
Internal assessment, though vital, has been a bone of
contention due to its ‘subjective’ nature. However, expert subjective
judgments can be as reliable as highly objective and standardized
assessments. A ‘Quarter model’ of internal assessment had been proposed
[4] to ensure that no test, teacher, tool or context contributes to more
than 25% to the total. MCI recommendations have also proposed a minimum
of three tests for pre- and paraclinical subjects and minimum of two
tests per professional year for the clinical subjects supplemented by
unlimited opportunities for formative ongoing assess-ments [1,5]. It is
important to involve all teachers in the department in the assessment
process to dilute subjecti-vity, to expose students to different ways of
thinking about a problem, and to train junior teachers in assessment. A
good record keeping in the form of a logbook or e-portfolio (an
electronic document that contains a log of learning activities as well
as an evidence of learning from those) is important to provide
developmental feedback to the students, especially for clinical skills
[6].
A welcome change in the new curriculum is that
internal assessment marks are shown separately in the final report and
are not added to marks of the University summative examinations. This
provides us better opportunities for using internal assessment as
multiple low stake assessment to assess acquisition of most
competencies. A satisfactory performance in internal assessment (50%
combined in theory and practical, minimum 40% in each) is still required
to be eligible for appearing for university examinations [1,5]. However,
it is simultaneously imperative to develop a feedback mechanism not only
to help students acquire the competencies but also to revisit and modify
teaching-learning methods and strategies.
There are 406 competencies listed in the subject of
Pediatrics out of which 23 are competencies that require certification
at ‘Perform’ level (Table I) [7]. As the competency-based system
focuses on integration of all domains of learning (cognitive,
psychomotor, affective) with communication skills, it is not possible to
assess the acquisition of competencies just by internal or intermittent
summative examinations. While it is relatively easy to implement the
summative component of internal assess-ment, a structured mechanism for
formative component with regular monitoring of students’ behavior and
assessment of patient records and logbooks remains a challenge. The
feasibility-criticality matrix provided in the Skill module [8] of
erstwhile MCI can be used as a guideline to classify what should be
tested during final examinations and what can be left for internal part.
As a general rule, all certifiable skills (Table I) should be
included in internal assessment while others can be included in the
formative part. Similarly, teacher to student ratio, and availability of
patients and skill labs should be considered to decide whether to use
real patients or manikins. A high level of motivation and coordination
among the teachers is required so that assessment is not taken as a
formality or burden but is utilized to monitor acquisition of
competencies as well as the department’s teaching-learning program. Up
to 20% marks in internal assessment have been allocated to logbooks and
this could be used as a handle to encourage formative assessments.
Assessment module by MCI [5], serves as a guide for development of
formative assessment which may be personalized by respective
Universities and institutions using the available resources [9].
A major issue with internal assessment has been
‘subjectivity’ and ‘bias’, which prevents us from making its full use.
An earlier proposed quarter model [4] provides useful guidelines.
Similarly, many components of programmatic assessment (PA) [10] can also
be incorporated, like utility of assessment [11] rather than attributes
of individual tool or assessment, and using every assessment to provide
liberal feedback to the students. Feasibility and educational impact are
important attributes for both formative as well as internal assessment.
To obviate the issues of subjectivity and bias, it is better to have all
teachers of the department involved in the process [4]. Since senior
residents are also considered teachers as per MCI guidelines, they can
be used for many formative events, especially those involving procedural
skills.
UNIVERSITY EXAMINATIONS
University examinations may not be the ideal way to
assess competencies due to logistic concerns. However, they are
extremely useful tools to help in quality maintenance and conducting
assessment. Graduate Medical Education Regulations (GMER) 2019 [1] and
MCI Assessment module [5] lay down the principles and broad structure
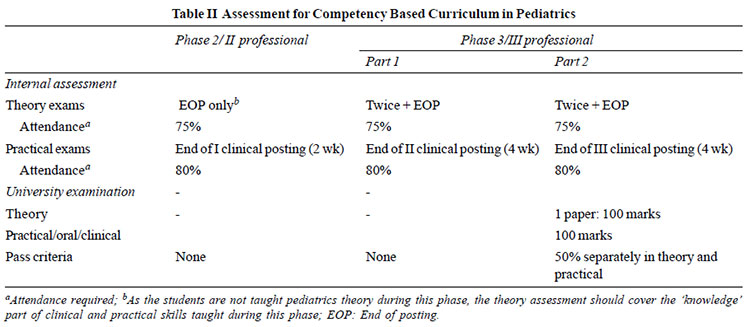
for the university examinations. Table II summarizes the
guidelines from these modules for summative assessment in the subject of
Pediatrics [1,5,7]. Different universities may adopt different
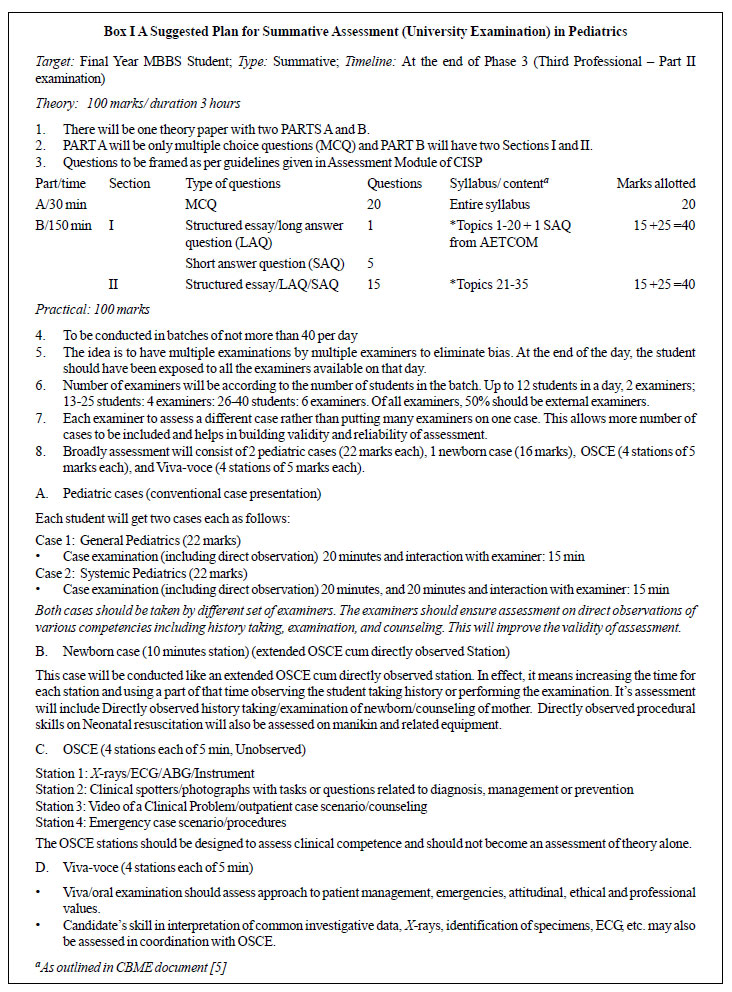
combinations of the same. A model for summative examination for
undergraduates in Pediatrics is proposed in Box I. The
scheme is in consonance with the proposals made by MCI. A key feature of
this process would be to assess higher levels of Miller pyramid [12],
aligning assessment with the competencies, and analyzing the analytical,
synthetic and problem-solving skills of the students. The MCI module on
assessment [5] has given few examples, which can be built upon. Examiner
orientation, framing scenario-based questions, and having model
questions to address various levels of Bloom Taxonomy are some inputs
which need to be provided.
 |
| |
| |
| |
 |
THE WAY FORWARD
Though introduction of competency-based curriculum
for undergraduate medical education is a desirable and long-due change,
it comes packaged with a lot of challenges. Assessment and documentation
of acquisition of competencies will require a high degree of dedication,
motivation and input in terms of time and resources, especially in busy
clinical departments with perpetual shortage of faculty. The capacity
building of the existing as well as new medical teachers is also a huge
task. MCI has mandated participation in Curriculum Implemen-tation
Support Program (CISP) for all medical teachers [5], which will only be
a sensitization. Moreover, the SARS CoV-2 pandemic in the years 2020 and
2021 has posed unique challenges and has interrupted the suggested
sequence of teaching-learning and/or assessment for at least two
successive batches of undergraduate students. Academic societies can
play a definite role in capacity building of faculty and in helping the
departments to develop appropriate teaching-learning methods and
assessment strategies. As the first step towards uniformity, Indian
Academy of Pediatrics (IAP) has already released learning objectives
based on MCI competencies [13]. These will be useful for implementation
of the competency-based curriculum for the first batch of MBBS students
admitted in 2019. The next challenge is to develop an assessment model
linked with competencies, especially the formative component in form of
its structure, tools (e.g., logbook/portfolio), settings and schedule.
Contributors: PG: conceptualized the paper. All
authors contributed to drafting and editing the article, and approval of
the final manuscript.
Funding: None; Competing Interests:
None stated.
REFERENCES
1. Board of Governors in Super-Session of Medical
Council of India. Regulations on Graduate Medical Education (Amendment),
2019. Accessed October 12, 2020. Available from:
https://www.mciindia.org/ActivitiWebClient/open/getDocu-ment?path=/Documents/Public/Portal/Gazette/GME-06.11.
2019.pdf
2. Epstein RM, Hundert EM. Defining and assessing
professional competence. JAMA. 2002;287:226-35.
3. Modi J, Gupta P, Singh T. Competency-based medical
education, entrustment and assessment. Indian Pediatr. 2015;52:415-20.
4. Singh T, Anshu, Modi JN. The quarter model: a
proposed approach for in training assessment of undergraduate students
in Indian medical schools. Indian Pediatr. 2012;49:871-6.
5. Medical Council of India. Assessment: Module-3.
Curriculum Implementation Support Program, 2019. Accessed Feb 12, 2021.
Available from: https://www.nmc.org.in/wp-content/up
loads/2020/08/Module_Competence_based_02.09.2019.pdf
6. Joshi MK, Gupta P, Singh T. Portfolio-based
learning and assessment. Indian Pediatr. 2015;52:231-5.
7. Medical Council of India. Competency Based
Undergraduate Curriculum for the Indian Medical Graduate, 2018. Vol. II.
Accessed February 12, 2021. Available from:https://www. nmc.org.in/wp-content/uploads/2020/01/UG-Curriculum-Vol-II.pdf
8. Medical Council of India. Skills Training Module
for Undergraduate Medical Education Program, 2019. Accessed December 21,
2020. Available from:
https://www.nmc.org.in/wp-ontent/uploads/2020/08/Skill-Module_23.12.2019.pdf
9. Singh T. Formative assessment: Assessment for
learning. In: Singh T, Anshu (eds). Principles of assessment in
medical education. 1st ed. Jaypee Brothers, 2012.p. 25-30.
10. Humphrey-Murto S, Wood TJ, Ross S, et al.
Assessment pearls for competency-based medical education. J Grad Med
Educ. 2017;9: 688-91.
11. van der Vleuten CPM, Schuwirth LWT. Assessing
professional competence: from methods to programs. Med Educ. 2005;39:
309-17.
12. Miller GE. The assessment of clinical
skills/competence/performance. Acad Med. 1990;65:S63–7.
13. Singh T, Gupta P. Indian Academy of Pediatrics releases uniform
learning objectives for competency-based curriculum in undergraduate
Pediatric education. Indian Pediatr. 2020;57:182-3.
|
|
|
 |
|

