|
|
|
Indian Pediatr 2021;58:765-770 |
 |
Impact of Air Pollution on Allergic Rhinitis
and Asthma: Consensus Statement by Indian Academy of Pediatrics
|
|
KR Bharath Kumar Reddy, 1
Neeraj Gupta, 2 Barnali G
Bhattacharya, 3 Nayan Mani
Deka,4 Parmarth Chandane,5
Rashmi Kapoor,6 Sarika
Gupta,7 Sowmya A Nagarajan,8
GV Basavaraja,9 Bakul Jayant
Parekh10
From Department of 1Paediatric Pulmonology and Sleep, Shishuka
Children’s Hospital, Bangalore; Departments of Pediatrics, 2Sir Ganga
Ram Hospital, Delhi; 3Childrens Clinic, Pune, Maharashtra; 4Asthma and
allergy Centre, Pratiksha Hospital, Guwahati, Assam; 5Bai Jerbai Wadia
Hospital for Children, Mumbai, Maharashtra; 6Regency Hospital, Kanpur,
Uttar Pradesh; 7King George Medical University, Lucknow, Uttar Pradesh;
8Sanjeevini Allergy and Immunology Centre and Kangaroo Care Hospitals,
Bengaluru, Karnataka; 9Indira Gandhi Institute of Child Health,
Bengalure, Karnataka; and 10President 2020, Indian Academy of
Pediatrics.
Correspondence to: Dr KR Bharath Kumar Reddy, Shishuka Children’s
Hospital, Kalyan Nagar, HRBR Layout, Bengalure, Karnataka 560 043.
Email: [email protected]
Published online: May 03, 2021;
PII: S097475591600321
|
Justification: Rising air pollution is an
ever-growing threat to many human diseases. Poor air quality has been
directly correlated with respiratory allergies with a disproportionate
affection among the pediatric age group. A clear understanding of common
air pollutants and their potential contribution in allergic rhinitis and
asthma is lacking. Objective: To formulate a consensus statement
for appropriate understanding among pediatricians and general
practitioners about the effects of air pollution on respiratory
allergies and their prevention. Process: A group of experts
(Pediatric pulmonologists and allergy specialists) from across India
were appointed by the Indian Academy of Pediatrics (IAP) to formulate a
consensus statement on ‘Allergy and Air pollution’. A virtual meeting
was conducted on 6th April 2020 to discuss in detail regarding various
issues related to the subject and a writing committee was formed with
broad consensus. After extensive literature review and multiple virtual
sessions, the current document was prepared and circulated via email to
the representatives from central IAP and IAP environment chapter. All
the experts approved the consensus with minor modifications after a
detailed discussion on 29th September 2020 on a virtual platform.
Recommendations: Air pollution is the emerging contributor to
respiratory allergies due to various mechanisms including oxidative
stress and compromised mucociliary clearance. Children are more
vulnerable to both outdoor and indoor pollution, due to their unique
physiological characteristics. Knowledge about pollutant particle size
and air quality index will help in demarcating level and extent of
airway involvement. Relevant environmental history in difficult allergic
rhinitis and asthma cases, along with conventional pharmacological
measures, is warranted. Multipronged approach, targeted at community,
physician and individual levels, needs to be emphasized to improve air
quality and reduce economic and psychological burden of respiratory
allergies.
Keywords: Air quality index, Allergy, Asthma, Pollution,
Rhinitis.
|
|
I
ncreasing levels of
air pollution and its impact on
health has emerged as an area of immense concern
across the world. Air pollution was found to be
responsible for 16% of global deaths, of which 92% were in low-
and middle-income countries (LMICs) [1]. There is ample evidence
emerging on the role that poor air quality could adversely
affect child health. Children remain a vulnerable group to the
effects of air pollution due to their outdoor play activity,
breathing higher concentration of pollutants, more mouth
breathing behaviour, higher minute ventilation, an ineffective
nasal filtering capacity, and an underdeveloped detoxification
and antioxidant defence systems [2]. There is a simultaneous
increase in the prevalence of respiratory allergies worldwide
[3], with the prevalence of wheeze ranging from 7-20% and
allergic rhinitis between 11-24% [4]. This increase correlated
with demographic changes of the cities including urbanization,
air pollution and environmental tobacco smoke [5]. Hence, a
pediatrician needs to be aware about the impact of air pollution
on allergic rhinitis and asthma, the two most common chronic
conditions that one addresses in daily clinical practice. By
understanding the interaction between air quality and allergy,
patient management can be improved with targeted preventive and
therapeutic measures.
PROCESS
A group of experts (pediatric pulmonologists
and allergy specialists) from across India were appointed by the
Indian Academy of Pediatrics (IAP) to formulate a consensus
statement on ‘Allergy and Air pollution’. A virtual meeting was
conducted on 6 April, 2020 to discuss in detail regarding
various issues related to the subject and a writing committee
was formed with broad consensus. After extensive literature
review and multiple virtual sessions, the current document was
prepared and circulated via email to the representatives from
central IAP and IAP environment chapter. All the experts
approved the consensus with minor modifications after a detailed
discussion on 29 September, 2020 on a virtual platform.
Terminology
Commonly used terms, which a pediatrician
needs to know, in the context of air pollution and allergy are:
Allergen: An allergen is a protein
component which produces an immunologically potent reaction in
which the immune system perceives a threat in susceptible
individuals, which otherwise is harmless to a majority of
people. An allergen is responsible for initiating an allergic
reaction.
Pollutant: Pollutants contaminate the
environment and render the natural resources toxic or unsuitable
for use when it crosses permissible limits. Air pollutants have
been known to augment the allergenicity of certain pollens and
fungal spores, but are directly non-immunogenic.
Irritant: An irritant is a substance,
mainly chemical, which may cause injury to mucosal tissues even
after a single exposure. Prolonged exposure may result in airway
diseases like asthma or skin disorders like contact
dermatitis/eczema.
Trigger: Trigger is a stimulus, which
when comes in contact with the immune system, initiates a
physiological exaggerated response, which can be a manifestation
of a disease. Allergens, pollutants and irritants can be
triggers of an allergic reaction.
Inducers: Inducers are agents which
enable the complex interaction of a pollutant and the
immunological mechanism. These may be i) exogenous,
either microbial (pathogen-associated molecular patterns, that
function through dedicated receptors, and virulence factors) or
non-microbial (allergens, irritants, toxic compounds), and ii)
endogenous such as signals produced by stressed or damaged
tissues [6].
Particulate matter (PM): It is a
predominant air pollutant which is frequently used as a proxy
indicator of air pollution. In urban areas, it includes dust,
smoke, and liquid droplets emitted into the air mainly by
vehicles, factories, and construction activities. Coarse
particles are PM ł2.5
microns (µm) to 10 µm (PM10) in aerodynamic diameter, while fine
particles are <2.5 µm (PM2.5). Ultrafine particles have sizes up
to 100 nanometers (nm) (PM0.1). Collectively, the PM less than
10 µm are called respirable PM. Coarse particles get deposited
in the upper airway, whereas fine and ultrafine PM can reach up
to the alveoli.
Air Quality Index (AQI): This
index has been developed for disseminating easy information
about complex parameters of air quality as a single number.
Calculation of AQI is usually computed from the concentration of
six major pollutants – ozone (O 3),
PM, nitric oxide (NO2),
sulphur dioxide (SO2),
carbon monoxide (CO) and lead (Pb), Further data availability,
averaging period, monitoring frequency and measurement methods
are used. However, PM (PM10, PM2.5) used in AQI is the
most commonly used marker of exposure to air pollution.
Sources of Air Pollution
Pollutants can be classified into household
air pollution (HAP) or ambient air pollution (AAP), primary (if
directly emitted into the atmosphere), or secondary (if these
react or interact therein, e.g., ozone-O 3)
based on their source and derivation. Table 1 enumerates
various sources of air pollutants. The AQI derived from these
pollutants is categorized as per their ill effects on human
health. The Indian standards for 24-hour air quality is;
however, relaxed when compared to United States Environmental
Protection Agency (USEPA) or WHO standards because of underlying
higher background pollution (i.e. is dust and natural sources)
which poses a challenge to achieve USEPA air quality standards
in a very short time [7]. An updated knowledge of AQI and its
impact on health can help a clinician to provide quality care to
his patients.
Pathophysiology
Exposure to air pollutants enhances the
airway responsiveness to aeroallergens via several mechanisms as
shown in Fig. 1. The pathophysiological mechanisms [12]
include: i) Traffic related pollutants and global warming
triggered pollen allergens release, ii) enhancement of
antigenic properties of biological aerosols (e.g. plant-derived
components and pollens) by air pollutants after adhering to
their surface, iii) increased penetration of allergens
and subsequent airway sensitization by the compromised
mucociliary clearance, iv) transport of free allergens to
lower airways after binding to particulate pollutants like
smoke, dust, and diesel exhaust particles (DEP), v)
changes in the epithelial structure and micro-flora through
oxidative stress and inflammatory reactions leading to allergic
immune response, vi) co-localization of adjuvants and
allergens on PM creating multivalent epitopes to cross-link
several IgE receptors, and triggering an exaggerated IgE
response, vii) chemical modification and oligomerization
of allergens by reactive oxygen and nitrogen species (ROS/RNS),
thus enhancing their immunogenicity with biological aging, and
viii) epigenetic changes causing DNA methylation in the
promoter region of immune effector genes by cigarette smoke.
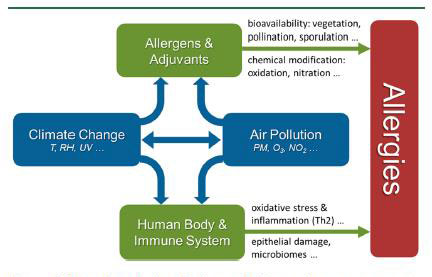
Reproduced with permission [11]. UV-Ultraviolet,
PM-Particulate matter, O3-Ozone, NO2-Nitrous oxide,
Th2-Type 2 Helper cells, T- Temperature, RH-Relative
Humidity.
|
|
Fig. 1 Pathophysiology of the
interplay of air pollution and allergies
|
How does air pollution affect asthma and
allergic rhinitis?
In more than 27 studies, it has been shown
that an acute increase in air pollution plays a significant role
in asthma flare-ups [13,14]. Nearly 15% of flare-ups in
asthmatic children were found to be attributed to TRAP
(Traffic-related air pollution) [15], especially in those whose
homes were close to roadways with a heavy truck density [16].
Hence, children exposed to higher levels of NO 2,
Ozone, PM 2.5 and PM 10 for a longer duration have lower lung
function and lung growth [17]. With increased life expectancy,
they might unmask asthma in the future and also have the
potential of developing chronic obstructive pulmonary disease
(COPD) [18]. Further-more, prenatal exposure to NO2,
SO2, PM 2.5, and PM
10 can affect the lung growth in a fetus, which can be
associated with an increased risk of asthma in childhood.
Other contributing factors include exposure
to mosquito coil, incense sticks and environmental tobacco smoke
(ETS). Burning of one mosquito coil produces as much PM 2.5 as
100 cigarettes and as much hydrocarbon as 50 cigarettes [19].
Incense sticks burning produces polyaromatic hydrocarbons,
benzene, carbon monoxide and PM 2.5. In a study in Cardiff
during Easter, the pollution inside a church due to incense
burning showed a marked increase in ultrafine PM, PM2.5 and PM
10. The oxidative stress was 25-30 times higher than that of
cigarette smoking [20]. Exposure to cigarette smoke can trigger
asthma symptoms, can lead to a flare up and even affect a
prenatal fetus. Prevalence of infant passive smoking is 10% in
Sweden, 60% in Greece, 40% in USA and 50-70% in South East Asia.
Second hand smoke (SHS) is as detrimental to health as active
smoking. It contains more than 4000 chemicals, of which 250 are
harmful. In addition, there is a strong correlation with
childhood obesity, asthma and ambient air pollution [21]. Higher
exposure to early life TRAP increased the rate of change of
childhood BMI [22], a known co-morbidity of difficult to control
asthma in children.
Many epidemiological and clinical trials
reveal that patients with allergic rhinitis, when exposed to
pollutants, have worsening of their symptoms [23]. In a
randomised controlled trial involving 253 adults with seasonal
allergic rhinitis (SAR) to ragweed pollen, it was observed that
controlled exposure to DEP and ragweed pollen in a special
exposure unit, significantly increased SAR symptoms compared to
ragweed exposure alone. This effect persisted beyond the end of
the DEP + pollen exposure period [24].
CONSENSUS STATEMENT
Evaluation of Impact of Air Pollution in a
Child
A pediatrician must take a detailed
environmental history (Box 1) in every child with asthma
or allergic rhinitis during the initial contact. Investigations
are needed in select situations and currently documented in
research settings only. Measures of inflammation like Fractional
Excretion of Nitric Oxide (FENO) or functional assessment with
spirometry or Impulse Oscillometry (IOS) should be monitored
[25]. Airway FENO level is a surrogate marker of eosinophilic
inflammation and corticosteroid sensitivity in bronchial asthma
[26]. It was found that annual increase in PM2.5, PM 10 and NO2
level were associated with significantly higher FENO
level [27]. The impact of air pollution on
lung function testing needs more evidence to establish
correlation. Measurements of metabolites of polycyclic aromatic
hydrocarbons (PAH) and cotinine/creatinine ratio in urine may
guide to the amount of air pollution and second hand smoke
exposure [28].
|
Box 1 Evaluation by Environmental
History – Questions to be asked by a Pediatrician
Indoor Home Environment
• Does the home have a separate
kitchen? What fuel is used for cooking?
• Is there any smoker at home?
• Do you use mosquito coil,
agarbatti or insecticide spray?
• Was there any recent
renovations at home, civil work, painting or wood
work? What is the type of wood used?
Home Surroundings
• How far is the home located
from main road?
• Is there any construction work
near home?
• Any garbage dump, weeds or farm
fields with post-harvest burning
• Are there any industries or
mills close to home?
• Does the child have aggravation
of symptoms during Diwali or Holi?
School related
• How does the child travel to
school?
• How far is the school located
from main road?
• Is there any construction work near school or any
renovations in school?
|
Prevention and Counselling
A multipronged strategy should be applied at
various levels of the healthcare infrastructure to prevent the
effects of air pollution on children. Medical organisations need
to make efforts in the field of research and publication to
disseminate knowledge among healthcare professionals,
colleagues, students and the community on air pollution and its
effects. Pediatricians must counsel and advice caregivers about
various measures which can be utilised to prevent the effects of
air pollution on child health.
Measures to Reduce Outdoor Air Pollution
and/or Its Effects
Face mask: For the community at large,
wearing any mask is recommended when the AQI score exceeds 200
or at PM2.5 concentrations of 150 mcg/m 3
and above [36]. Although, N95 mask is most effective for
filtering PM2.5 particles, a reusable 3-layer cotton cloth mask
can suffice for many children.
Clean fuels for vehicles: Encourage use
of newer and lesser polluting fuels, with less exposure to
diesel fumes [29]. Electric vehicles can be a welcome
initiative.
Restriction of outdoor activities:
Advice to keep children indoors when AQI is poor or pollen count
is high [30].
Measures to Reduce Indoor Air Pollution
Reduce molds, dust and dust mites
concentration: This can be achieved by washing
bedding on weekly intervals using hot water at 54 OC
or by employing commercially available mite-proof bedding.
Feather dusters disperse dust and allergens and thus should be
avoided. Moist cloth should be preferred over dry ones for
wiping dirt [31]. Vacuum cleaners should be sealed tightly to
avoid a dust leak. Cleaning products with a high composition of
volatile organic compounds (VOC), scents, or odours should be
avoided.
Home ventilation and use of air purifiers:
An air purifier can be used in cases where significantly poor
air quality is documented. To help choose an air purifier, the
patient can be advised to choose one with a Clear air delivery
rate (CADR) of more than 600, and with a Minimum efficiency
reporting value (MERV) of the High efficiency particulate air
(HEPA) filter more than 14. One must; however, replace and clean
filters periodically and install the machine away from walls or
furniture.
Cooking fuels: Use of clean fuels
for cooking like LPG should be encouraged at home. Biomass fuels
and stoves should be avoided.
Cessation of smoking (both active and
passive): Exposure to ETS should be reduced in all forms.
Public health measures like bans on smoking in public places and
media education campaign on benefits of cessation are useful
[32].
Cessation of use of mosquito coils, agarbatti
and dhup sticks in households [33].
Furniture with pressed wood need to be
avoided : These types of
furniture can emit high levels of VOC, formaldehyde and
carbamide (urea) [34]. Formaldehyde is commonly used to bond the
adhesives in pressed wood products. It is a hazardous pollutant
that can pose a serious threat to health if exposed for a long
period of time. The rate at which formaldehyde is released into
the air is accelerated by heat and humidity, so avoid placing
new pieces of furniture over or near a heat source.
Renovation and painting of the house needs to
be done during a holiday break when children are out of home.
Selecting a school or building a new house
needs to be considered very carefully so that it is at least 100
meter away from the main road.
Measure to Build Lung Capacity
Yoga and relaxation therapy: These have
been found to increase the peak expiratory flow rate in children
as well as improve the lung function and
quality of life in adults.
Exercise and other physical activities:
Regular aerobic activity has the potential to improve lung
capacity and reduce bronchial hyper responsiveness
Management of Asthma and Allergic Rhinitis in
the Presence of Pollution
Although the principles of management in
children with asthma and allergic rhinitis remain the same,
focus needs to be laid on exposure to air pollution as a trigger
of flare-ups and cause for poorly controlled symptoms. In
addition to avoidance of exposure of pollutants on high
pollution days, asthma flare-ups can be prevented by using
maintenance dose of inhaled corticosteroid therapy (ICS) on a
regular basis [35]. Studies suggest that this approach has shown
to decrease an adverse response to pollutant exposure [36]. Some
additional measures like use of reliever medication or stepping
up of ICS for few days during poor air quality monitored by AQI
and pollen calendar is advisable, although there are limited
studies to support this. Stepping down of ICS and outdoor
activities should be discouraged on days with a high AQI or high
pollen count.
Management of allergic rhinitis with
intranasal corticosteroids (INCS) and antihistamines should be
based on the severity of symptoms and treatment should be
continued on days of poor air quality as per the AQI. Despite
recent discoveries on mechanistic biomarkers and signal pathways
of cellular oxidative stress injury secondary to pollutant
exposure, efficacy studies on pharmacological therapy of AR
patients exposed to specific pollutants is currently lacking
[37]. In adults, fexofenadine demonstrated efficacy and a
well-tolerated safety profile in ragweed AR patients exposed to
ragweed associated to Diesel exhaust particles (DEP) in an
environmental exposure unit. There was improved nasal symptom
scores following ragweed plus DEP exposure when pre-treated with
fexofenadine compared to the placebo group [38,39]. However,
paediatric focused clinical studies are needed to address the
need of managing allergies caused or aggravated by air
pollution. In children with poorly controlled asthma or allergic
rhinitis despite high doses of conventional medication, the
contribution of air pollution needs to be considered and
evaluated in detail.
CONCLUSION
Air pollution has a significant impact on
respiratory allergies in children through various mechanisms.
Physicians managing children with allergic rhinitis and/or
asthma regularly need to be well versed with the pathophysiology,
evaluation and management, and be able to suggest targeted
preventive measures. More research in pediatric patients is
needed to enhance our knowledge and practices in this field.
Note: A detailed version is available at
www.iapindia.org
Contributors: HP,VHR,TUS,RB:
contributed, designed and approved the manuscript. All authors
approved the final version of manuscript.
Funding: None; Competing interest:
None stated.
References
1. Landrigan PJ, Fuller R, Acosta NJR, et
al. The Lancet Commission on pollution and health. Lancet.
2018;391:462-512.
2. Goldizen FC, Sly PD, Knibbs LD.
Respiratory effects of air pollution on children. Pediatr
Pulmonol. 2016;51:94-108.
3. Lai CK, Beasley R, Crane J, et al.
Global variation in the prevalence and severity of asthma
symptoms: Phase three of the International Study of Asthma
and Allergies in Childhood (ISAAC). Thorax. 2009; 64: 476–83
4. Asher MI, Montefort S, Bjorksten B, et
al. Worldwide time trends in the prevalence of symptoms of
asthma, allergic rhinoconjunctivitis, and eczema in
childhood: ISAAC phases one and three repeat multicountry
cross-sectional surveys. Lancet. 2006; 368:733-43.
5. Paramesh H. Epidemiology of asthma in
India. Indian J Pediatr. 2002;69:309-12.
6. Medzhitov. Origin and Physiological
roles of inflammation. Nature. 2008;454:428-35.
7. Central pollution control board of
India. CUPS/82/2014-15 National Air quality Index.
Oct 2014.www.cpcb.nic.in.
8. Sharma M, Bhattachrya A, Gargava P.
Developing national air quality index. Ann Indian National
Acad Engineering. 2018;13:5-35
9. Goldizen FC, Sly PD, Knibbs LD.
Respiratory effects of air pollution on children. Pediatric
Pulmonol. 2016;51:94-108.
10. Schwartz J. Air Pollution and
Children’s Health. Pediatrics. 2004;113:1037-43.
11. Gorai AK, Tuluri F, Tchounwou PB. A
GIS based approach for assessing the association between air
pollution and asthma in New York state, USA. Int J Environ
Res Public Health. 2014;11:4845-69.
12. Ritz B, Wilhelm M. Air pollution
impacts on infants and children. Los Angeles (CA): UCLA
Institute of the Environment; 2008
(https://www.ioes.ucla.edu/publication/air-pollution-impacts-on-infants-and-
children/, accessed August 2018).
13. Molini M Patel, Rachel L. Miller. Air
pollution and childhood asthma: recent advances and future
directions. Curr Opin Pediatr. 2009;21:235-42.
14. Tzivian L. Outdoor Air Pollution and
Asthma in children. J Asthma. 2011;48:470-81.
15. Perez L, Declercq C, Ińiguez C, et
al. Chronic burden of near-roadway traffic pollution in 10
European cities (APHEKOM network). Eur Respir J.
2013;42:594-605.
16. Perez L, Lurmann F, Wilson J, et al.
Near-roadway pollution and childhood asthma: implications
for developing "win-win" compact urban development and clean
vehicle strategies. Environ Health Perspect.
2012;120:1619-26.
17. Burbank AJ, Peden DB. Assessing the
impact of air pollution on childhood asthma morbidity: How,
When and What to do. Curr Opin Allergy Clin Immunol.
2018;18:124-31.
18. Schultz ES, Halberg J, Bellander T,
et al. Early life exposure to traffic related air pollution
and lung function in adolescence. Am J Resp Crit Care Med.
2015;2:171-77.
19. Liu W, Zhang J, Hashim JH, et al.
Mosquito coil emissions and health implications. Environ
Health Perspect. 2003;1110: 1454-60.
20. Chuang HC, Jones T, Berube K.
Combustion particles emitted during church services:
Implication for human respiratory health. Environ
International. 2012;40:137-142
21. de Bont J, Casas M, Barrera-Gómez J,
et al. Ambient air pollution and overweight and obesity in
school aged children. Environ Int. 2019;125:58-64.
22. Kim JS, Alderete TL, Chen Z, et al.
Longitudinal association of in utero and early life near
airway air pollution with trajectories of childhood body
mass index. Environ Health. 2018;17:64.
23. Van Gerven L, Boeckxstaens G,
Hellings P. Up-date on neuro-immune mechanisms involved in
allergic and non-allergic rhinitis. Rhinology.
2012;50:227-35.
24. Ellis AK, Murrieta-Aguttes M, Furey
S, Carlsten C. Phase 3, single-center, sequential and
parallel group, double-blind, randomized study evaluating
the efficacy and safety of Fexofenadine Hydrochloride 180 mg
(Allegra/Telfast) versus placebo in subjects suffering from
Allergic Rhinitis with symptoms aggravated in presence of
pollutants: Analysis of individual symptom scores. World
Allergy Organ J. 2020; 13:100137:92.
25. Pijnenburg WH, De Jongste JC. Exhaled
nitric oxide in childhood asthma: A review. Clinical and
Experimental Allergy. 2008;38:246-59.
26. Berry A, Busse WW. Biomarkers in
asthmatic patients: has their time come to direct treatment?
J Allergy Clin Immunol. 2016;137:1317-24.
27. Zhang Y, Berhane K, Eckel SP, et al.
Adverse effects of annual fluctuations in air pollution on
feno in children: A longitudinal study. Am J Respir Crit
Care Med. 2018;197:A1020.
28. Pope CA, Turner MC, Burnett RT, et
al. Relationships between fine particulate air pollution,
cardiometabolic disorders, and cardiovascular mortality.
Circ Res. 2015;116:108-15.
29. Xing YF, Xu YH, Shi MH, Lian YX. The
impact of PM2.5 on the human respiratory system. J Thorac
Dis. 2016;8:E69-E74.
30. Levetin E, Van de Water PK. Pollen
count forecasting. Immunol Allergy Clin North Am.
2003;23:423-42.
31. Naclerio R, Ansotegui IJ, Bousquet J,
et al. International Expert Consensus on the Management of
Allergic Rhinitis (AR) Aggravated by Air Pollutants Impact
of Air Pollution on Patients with AR: Current knowledge and
future strategies. World Allergy Organ J. 2020;13:100106.
32. Rosen LJ, Myers V, Winickoff JP, Kott
J. Effectiveness of interventions to reduce tobacco smoke
pollution in homes: A systematic review and meta-analysis.
Int J Environ Res Public Health. 2015;12:16043-59.
33. Liu W, Zhang J, Hashim JH, et al.
Mosquito coil emissions and health implications. Environ
Health Perspect. 2003;111: 1454-60.
34. Mendell MJ. Indoor residential
chemical emissions as risk factors for respiratory and
allergic effects in children: a review. Indoor Air.
2007;17:259-77.
35. Indinnimeo L, Chiappini E, Miraglia
del Giudice M, et al. Guideline on Management of the Acute
Asthma Attack in Children by Italian Society of Pediatrics.
Italian J Pediatrics. 2018;44:46.
36. Delfino RJ, Zeiger RS, Seltzer JM,
Street DH, McLaren CE. Association of asthma symptoms with
peak particulate air pollution and effect modification by
anti-inflammatory medication use. Environ Health Perspect.
2002;110:A607-17
37. Naclerio R, Ansotegui IJ, Bousquet J,
et al. International Expert Consensus on the Management of
Allergic Rhinitis (AR) Aggravated by Air Pollutants: Impact
of Air Pollution on Patients with AR: Current Knowledge and
Future Strategies. World Allergy Organ J. 2020;13:100106.
38. Ellis AK, Murrieta-Aguttes M, Furey
S, et al. Phase 3, single center, sequential and
parallel-group, double-blind, randomized study evaluating
the efficacy and safety of fexofenadine hydrochloride 180 mg
(Allegra/Telfast) versus placebo in subjects suffering from
seasonal allergic rhinitis with symptoms aggravated in
presence of pollutants. World Allergy Organ J. 2020.
abstract #00257.
39. Ellis AK, Murrieta-Aguttes M, Furey S, et al. Phase 3,
single center, sequential and parallel-group, double-blind,
randomized study evaluating the efficacy and safety of
fexofenadine hydrochloride 180 mg (Allegra/Telfast) versus
placebo in subjects suffering from seasonal allergic rhinitis
with symptoms aggravated in presence of pollutants: Analysis of
individual symptom scores. World Allergy Organ J. 2020. abstract
#00258.
|
|
|
 |
|

