|
|
|
Indian Pediatr 2021;58:639-642 |
 |
Developmentally
Supportive Positioning Policy for Preterm Low Birth Weight
Infants in a Tertiary Care Neonatal Unit: A Quality Improvement
Initiative
|
|
Jaya Upadhyay, Poonam Singh, Kanhu Charan Digal, Shantanu Shubham,
Rajat Grover, Sriparna Basu
From Department of Neonatology, All India Institute of Medical
Sciences, Rishikesh, Uttarakhand.
Correspondence to: Prof Sriparna Basu, Department of Neonatology, All
India Institute of Medical Sciences, Rishikesh, Uttarakhand 249203.
[email protected]
Received: January 06, 2020;
Initial review: April 07, 2020;
Accepted: September 26, 2020.
Published online: January 2, 2021;
PII:S097475591600269
|
Objective: To improve developmentally supportive
positioning practices by 50% in neonates weighing <1800 g, admitted in a
neonatal intensive care unit over 6 months. Methods: Infant
Position Assessment Tool (IPAT) scores were used for assessment of the
ideal position. Proportion of neonates with IPAT score
³8 and
improvement of average IPAT score were the process and the outcome
measures, respectively. At baseline, 16.6% of infants had optimum
position. After root cause analysis, interventions were done in multiple
Plan-Do-Study-Act (PDSA) cycles of educational sessions, positioning
audits, use of low-cost nesting aids, and training of mothers.
Results: Over 21 weeks, 74 neonates were observed at 714
opportunities. Over 6 months, mean (SD) IPAT score improved from 3.4
(1.4) to 9.2 (2.8). Optimum positioning was maintained in 83.3% neonates
during sustenance phase. Conclusions: Low-cost interventions,
awareness regarding standards of optimum positioning and involvement of
primary caregiver can effectively improve infant positioning practices.
Keywords: Conformational position, Infant Positioning
Assessment Tool (IPAT), Nursing care, Posture, Outcome.
|
|
I n developmental
supportive care (DSC), positioning is the most important
strategy that affects physiological stability and reduces stress
[1]. Optimum positioning improves sleep, reduces pain, decreases
apnea/desaturation episodes, improves ther-mal regulation, skin
integrity and neurobehavioral organization [2,3]. Several
studies have documented beneficial effects of supportive
positioning interventions including reduction in musculoskeletal
abnormalities and better neuromotor outcomes [4,5]. Frequent
position changes with the use of ‘nesting’ or ‘conformational
positioner’ have shown to improve the postural regulation with
maintenance of optimum position [6,7].
The awareness of neonatal caregivers
regarding infant positioning is scanty [8]. Improvement of
practices were documented after educational training,
positioning audits and policy formation [9]. This quality
improvement (QI) initiative was undertaken to improve the
develop-mentally supportive positioning practices in low birth
weight neonates.
METHODS
Our neonatal intensive care unit (NICU) is a
24-bedded level-III unit with >2500 deliveries/year and >100
admission/month. The nurse: patient ratio is 1:1 for neonates on
ventilator, 2:1 for sick neonates and 4:1 for relatively stable
infants. The concept of DSC in our unit was limited to the
routine use of a shoulder roll only. On a cross-sectional review
of practice, over 80% admitted neonates at our center were found
in unacceptable positions, supine with retracted
shoulders/extremities (93.4%), undue neck flexion (70%) and
excessive hip abduction due to oversized diaper (100%).
We aimed to improve developmentally
supportive positioning practices by 50% in neonates weighing
<1800 g admitted in the NICU over 6 months (April,
2019-September, 2019). This QI initiative was based on
point-of-care quality initiative (POCQI) model [10]. Ethical
clearance was obtained from Institute Ethics Committee.
Infant positioning assessment tool (IPAT;
Philips Children’s Medical Ventures), validated by several
studies [11-14] was used to improve the positioning practices.
Eligible neonates (birthweight <1800 g) were scored by a team of
‘Positioning proponents (PP)’, once in every shift and an
average daily score was assigned to each baby. Proportion of
neonates with average IPAT score
³8 was taken
as the process measure. Improvement in mean IPAT scores was the
outcome measure.
Baseline phase (4 weeks): In this phase,
the applicability of IPAT score was validated in 6 neonates at
30 oppor-tunities. A team of two doctors and six nurses
identified as PP, were trained in developmentally supportive
position-ing practices and IPAT scoring. Mean (SD) IPAT score
was 3.4 (1.4) and proportion of neonates with mean IPAT
³8 was 16.6%.
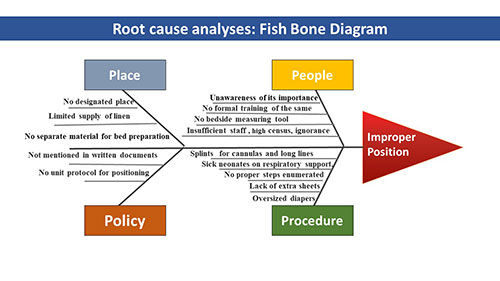
Potential causes of improper positioning identified through root
cause analysis (Fig. 1) included lack of
knowledge/skills, unavailability of positioning aids, high
patient load, respiratory support, multiple infusions and
non-availability of measurement tool.
 |
|
Fig. 1 Root cause analyses: Fish
bone diagram for improper positioning.
|
Intervention phase: After baseline phase,
Plan-Do-Study-Act (PDSA) cycles (Web Fig. 1) were
used for interventions. IPAT was introduced and one-to-one
teaching, hands-on demonstration-cum-practice session and
assessment of nurses and residents were started. Data were
recorded in excel sheet and plotted on run chart weekly. To
prevent bias, average score was disclosed weekly.
PDSA-1: Learning by doing (4
weeks): A schedule and the teaching material were
distributed among team members. IPAT print-outs were made
available at the bedside. Group teaching, informal bedside and
one-to-one teaching, position demonstration on mannequin and
baby were continued for next 2 weeks in every nursing shift.
Nurses were assessed once weekly for IPAT scoring of five
neonates with demonstration of ideal positioning. Additional
review sessions were organized for newly-posted residents and
nurses. Educational material was shared electronically. Finally,
IPAT scoring was made a part of daily nursing care with scoring
done in each shift and entered in nursing notes.
PDSA-2: Customized boundary (4
weeks): Preparation of boundaries or ‘nesting’ with rolled
linens was detected as one of the limiting factors due to
non-availability of linens and reluctance of nurses for the
labour-intensive process of preparing the nest. To resolve this,
we prepared customized low-cost, washable and autoclavable, foam
based reusable boundaries with covers by the hospital tailor (Fig. 2).
This intervention decreased the require-ment of linen rolls and
significantly reduced the time required for positioning of the
neonates without impos-ing an additional burden to prepare
nesting, boosting their enthusiasm for improving position. After
this intervention, 50% of neonates had an IPAT score
³8.
 |
|
Fig. 2 Positioning aid for
optimum positioning.
|
Two sick neonates were observed to developed
occipital bedsore due to prolonged supine positioning. In order
to maintain high IPAT score, nurses were maintaining supine
posture with fixed boundaries without changing to lateral/prone
positions. An amendment in positioning policy was made with
inclusion of compul-sory three-hourly position change.
PDSA-3: Appraisal and improvement
(12 weeks): In this phase, we started selecting ‘PP of the week’
and appreciating them with a badge, which further improved the
zeal of caregivers. Workshops on DSC with weekly refresher
sessions were conducted. Now, positioning be-came a routine
practice amongst the caregivers improving the proportion of
neonates with IPAT ³8
to 72.5%.
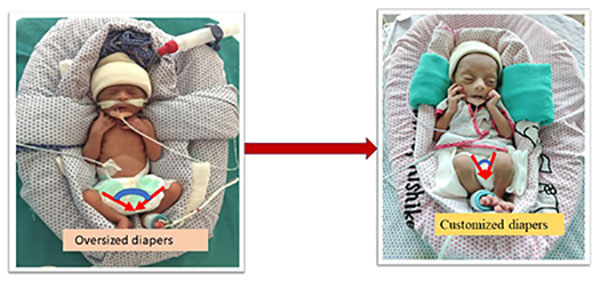
PDSA-4: Sizing the diapers (4
weeks): Following third PDSA cycle, it was analyzed that
position of hips and legs could not be maintained because of
oversized diapers. Since small diapers were not a part of
hospital supply, we started making customized diapers for
preterm with cotton and gauze (Fig. 3). After
this, the number of neonates with oversized diapers reduced from
74.5-20%.
 |
|
Fig. 3 Customized diapers for
extremely low birth weight babies.
|
PDSA-5: Training of mothers (8
weeks): After fourth PDSA cycle there was a visible improvement
in position-ing practices of the unit. Team analyzed that most
of the LBW neonates are shifted to step-down units with their
mothers soon after clinical stabilization, and decided to train
the mothers. Teaching materials and posters were prepared in the
local language. Demonstrations were done using mannequins daily
for one week. Every new mother was given a refresher tutorial.
Training mainly focussed on preparation of boundaries using
easily available home-stuff such as towels and scarfs,
preparation of shoulder rolls and its correct placement,
difference between improper and proper positions and their
long-term implications. ‘Position expert’ mothers were praised
and asked to teach other mothers. Considerable acceptance was
noted in their behavior.
RESULTS
Before starting interventions, each PP
independently scored 6 neonates at 30 opportunities. Inter-rater
reliability was analyzed with interclass correlation coefficient
(95% CI) of 0.89 (0.83-0.94) using two-way mixed model,
suggesting a strong level of agreement and high reliability of
data-recording. For the position data, we calculated the
baseline mean using the first 10 data-points and recalculated
the mean whenever a shift in data was identified. In the
baseline phase, 18 neonates with mean (SD) birthweight and
gestational age of 1230 (265) g and 30.5 (2.6) weeks,
respectively were observed over 4 weeks. Mean (SD) IPAT score
was 3.4 (1.4) and 16.6% of eligible neonates had IPAT score
³8.
Throughout this project, 74 neonates were
observed at 714 opportunities. Forty-four nurses, 10 senior
residents, 15 junior residents and 52 mothers were trained in
standard positioning practices. Total 23 teaching sessions were
conducted including 12 sessions of hands-on demons-tration, 2
institutional workshop and 9 assessment sessions. For training
of mothers, 12 teaching sessions and 20
demonstration-cum-hands-on training were conducted.
After first PDSA, mean (SD) IPAT score
improved to 5.2 (1.6) with biggest limitation being lack of
positioning aids. After third and fourth PDSA, introduction of
nesting rolls and appropriate size diapers had significantly
improved mean (SD) IPAT score to 9.2 (2.8) with sustenance for
next 6 weeks. The chart showed less than expected number
of runs signalling for an improved practice. In the last PDSA
cycle, the baseline data was recorded again when the baby was
shifted to step-down unit with the mother. Baseline mean (SD)
IPAT scores of 3.5 (1.3) improved over next 5 weeks to 8.3 (0.2)
(Web Fig. 2).
DISCUSSION
This short-term QI project aimed to improve
the practice of infant positioning. A significant improvement
was noted in the proportion of admitted neonates with IPAT score
³8
from the baseline of 16.6-83.3%. In coherence with other
projects on position improvement [12-14], nursing teaching and
demonstration sessions were found to be most impactful.
Inclusion of mothers in the loop was the most important factor
for sustenance policy.
Compared to previous reports [12-14], the
major difference in this project was the achievement of targeted
improvement within a short time-span. The quick response was
attributed to multiple PDSA cycles, adopting the changes and
policy formation in each step. Advent of customized nesting
boundary was a cost-effective intervention with minimal
consumption of linen. The biggest strength of this project was
involvement of mothers as an addition to the concept of family-centred
care. The major limitation was that we did not assess long-term
developmental outcome.
To conclude, this QI project, using simple
cost-effective interventions through multiple PDSA cycles and
team effort, led to a considerable improvement in positioning
practices of our unit. Involvement of mothers in the project was
an important addition for better sustenance.
Ethics clearance: Institutional ethics
committee, AIIMS, Rishikesh; AIIMS/IEC/19/698; dated
April 12, 2019.
Contributors: JU, PS, SB:
conceptualized and designed the study, coordinated and
supervised data collection, drafted the initial manuscript; KCD,
SS, RG: coordinated and supervised data collection, and reviewed
and revised the manuscript. All authors approved the final
manuscript.
Funding: None; Competing
interests: None stated.
| |
|
WHAT THIS STUDY ADDS?
•
Compliance with
developmental supportive positioning can be improved by
standardizing positioning policy, staff education, low
cost interventions to ease the process of positioning,
and involvement of primary care giver to ensure long
term benefits.
|
REFERENCES
1. Blackburn S. Environmental impact of
the NICU on de-velopmental outcomes. J Podiatry Nurs.
1998;13:279-89.
2. Altimier L, Phillips R. The neonatal
integrative develop-mental care model: Advanced clinical
applications of the seven core measures for neuroprotective
family-centered developmental care. Newborn Infant Nurs Rev.
2016;16: 230-44.
3. Madlinger-Lewis L, Reynolds L, Zarem
C, Crapnell T, Inder T, Pineda R. The effects of alternative
positioning on preterm infants in the neonatal intensive
care unit: A randomized clinical trial. Res Dev Disabil.
2014;35:490-7.
4. Vaivre-Douret L, Ennouri K, Jrad I,
Garrec C, Papiernik E. Effect of positioning on the
incidence of abnormalities of muscle tone in low-risk,
preterm infants. Eur J Paediatr Neurol. 2004;8:21-34.
5. Hughes AJ, Redsell SA, Glazebrook C.
Motor development interventions for preterm infants: A
systematic review and meta-analysis. Pediatrics.
2016;138:e20160147.
6. Ferrari F, Bertoncelli N, Gallo C, et
al. Posture and movement in healthy preterm infants in
supine position in and outside the nest. Arch Dis Child
Fetal Neonatal Ed. 2007;92:F386-90.
7. Visscher MO, Lacina L, Casper T, et
al. Conformational positioning improves sleep in premature
infants with feedingdifficulties. J Pediatr. 2015;166:44-8.
8. Jeanson E. One-to-one bedside nurse
education as a means to improve positioning consistency.
Newborn Infant Nurs Rev. 2013;13:27-30.
9. Zarem C, Crapnell T, Tiltges L, et al.
Neonatal nurses’ and therapists’ perceptions of positioning
for preterm infants in the neonatal intensive care unit.
Neonatal Netw J Neonatal Nurs. 2013;32:110-6.
10. POCQI-Learner-Manual.pdf [Internet].
Accessed Septem-ber 25, 2020. Available from: https://
www.newborn whocc.org/POCQI-Learner-Manual.pdf
11. Coughlin M, Lohman MB, Gibbins S.
Reliability and effectiveness of an infant positioning
assessment tool to standardize developmentally supportive
positioning practices in the neonatal intensive care unit.
Newborn Infant Nurs Rev. 2010;10:104-6.
12. Masri S, Ibrahim P, Badin D, Khalil
S, Charafeddine L. Structured educational intervention leads
to better infant positioning in the NICU. Neonatal Netw.
2018;37:70-7.
13. Spilker A, Hill C, Rosenblum R. The
effectiveness of a standardized positioning tools and
bedside education on the developmental positioning
proficiency of NICU nurses. Intensive Crit Care Nurs.
2016;35:490-7.
14. Charafeddine L, Masri S, Ibrahim P, Badin D, Cheayto S,
Tamim H. Targeted educational program improves infant
positioning practice in the NICU. Int J Qual Health Care.
2018;30:642-8.
|
|
|
 |
|

