|
|
|
Indian Pediatr 2021;58:729-732 |
 |
Etiology-Based
Decision-Making Protocol for Pediatric Cholelithiasis
|
|
Vikesh Agrawal, 1 Abhishek
Tiwari,1 Dhananjaya Sharma2,
Rekha Agrawal3
From 1Pediatric Surgery Division, 2Department of Surgery, and
3Department of Radiodiagnosis, Netaji Subhash Chandra Bose Medical
College, Jabalpur, Madhya Pradesh.
Correspondence to: Dr Vikesh Agrawal, Department of Surgery, Netaji
Subhash Chandra Bose Medical College, Jabalpur, Madhya Pradesh.
Email:
[email protected]
Received: July 12, 2020;
Initial review: July 07, 2020;
Accepted: September 26, 2020
Published online: January 02, 2021;
PII: S097475591600276
|
Objective: We reviewed hospital records
of pediatric cholelithiasis to develop an etiology-based
decision-making protocol. Method: This retrospective study was
conducted on consecutive pediatric cholelithiasis patients from July,
2014 to June, 2019 in a tertiary care center. Pediatric cholelithiasis
was classified according to etiology, and the outcome of
medical/surgical treatment was noted. Result: Data of 354
pediatric patients were analyzed. Commonest (56.2%) etiology was
idiopathic; followed by ceftriaxone pseudo-lithiasis (26.8%). Pigment
stones were associated with the highest rate of complications. Non-hemolytic
stones had a lower complication rate and a high rate of resolution with
medical therapy. Conclusion: Hemolytic and symptomatic stones
warrant an early cholecystectomy, whereas asymptomatic idiopathic
stones, ceftriaxone stones, and TPN-induced stones are candidates for
medical therapy under close observation.
Keywords: Ceftriaxone, Gall stone, Hemolytic anemia,
Management, Outcome.
|
|
P ediatric
cholelithiasis is increasingly being
diagnosed nowadays because of the use of
abdominal ultrasonography screening [1]. Its
prevalence in the Indian population has been reported to be rare
[2]. Common causes are idiopathic (30-54%), hemolytic disorders
(20-30%), and non-hemolytic causes (20-30%) such as ceftriaxone
therapy, total parenteral nutrition (TPN), obesity and cystic
fibrosis [3]. The treatment of choice for pigment stones is
surgery; however, guidelines and consensus are lacking for the
management of other stones, developed a simple etiology-based
decision-making protocol for pediatric cholelithiasis, after
analyzing our institutional data.
METHODS
We received hospital records from July, 2014
to June, 2019 of consecutive patients <18 years of age with
cholelithiasis/sludge in the pediatric surgical unit of a
tertiary center. Case records with incomplete data, and those
with a diagnosis of choledochal cyst were excluded.
Records were reviewed for demographic
information, symptoms (non-specific abdominal pain, right
hypochon-driac pain or biliary colic, nausea,vomiting,
jaundice), predisposing factors (body mass index, history of
fast food eating habit, acute gastroenteritis, dehydration,
hemolytic disorder, ceftriaxone injection, total parenteral
nutrition) and complications (acute cholecystitis, chronic
cholecystitis, choledocholithiasis, cholangitis, gall bladder
perforation). Fast food eating habit was defined as frequent
consumption of food containing a rich mix of refined sugars,
salt, and fats, and low in fibers. The child was considered
obese if BMI was >27 on IAP growth charts [4]. Ultrasonography
(USG) findings included floating hyperechoic lesion in gall
bladder with posterior acoustic shadow, echogenic sludge without
posterior acoustic shadow, gall bladder wall thickening (>3 mm
with 6 hours fasting), peri-cholecystic collection, common bile
duct (CBD) stone, and CBD and intrahepatic biliary radical
dilatation.
Cholelithiasis was classified according to
etiology: pigment stones (due to hemolytic disorders; positive
on hemoglobin electrophoresis), ceftriaxone pseudolithiasis
(cholelithiasis noticed within 21 days of >3 days of
intra-venous ceftriaxone therapy with a normal pre-ceftriaxone
ultrasound report), stone or sludge secondary to TPN (developing
after TPN); all others were labeled idiopathic. Hemoglobin
electrophoresis was done for all patients with cholelithiasis
diagnosed on ultrasound, and all patients with hemolytic
disorders underwent an ultra-sound to document hemolytic stones.
Cholecystectomy (open or laparoscopic;
depending on availability and patient condition) was performed
for all pigment stones (on diagnosis or presentation with a
complication). Medical therapy (Ursodeoxycholic acid (UDCA) 25
mg/kg/day for 6 months) was advised for all non-hemolytic
stones. These patients were followed up with clinical
examination and ultrasound every 3 months. The stone resolution
was defined as an anechoic gall bladder on two consecutive
three-monthly ultrasounds. Patients developing complications
were dealt with in an emergent manner. Choledocholithiasis was
managed with endoscopic stone extraction and interval
cholecystec-tomy. Treatment is given
(routine/emergent/medical/cholecystectomy) and outcomes were
recorded.
Data analysis: Data analyses were
performed using an online Graphpad analyzer. All variables were
analyzed descriptively, and chi-square test or t-test
were used for statistical analysis. A value of P<0.05 was
considered significant.
RESULTS
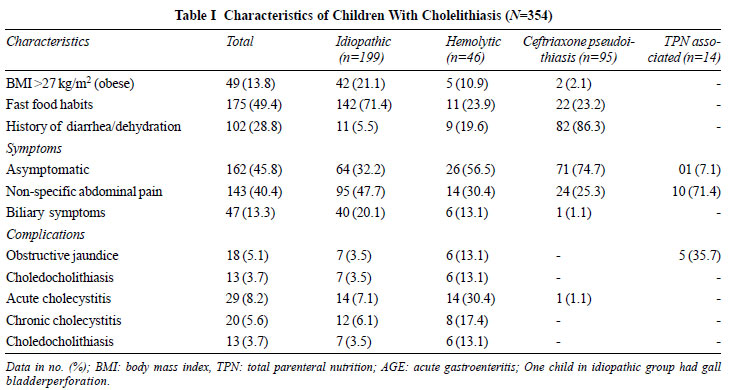
A total of 426 children (53.7% females) with
cholelithiasis fulfilled inclusion criteria, and were included
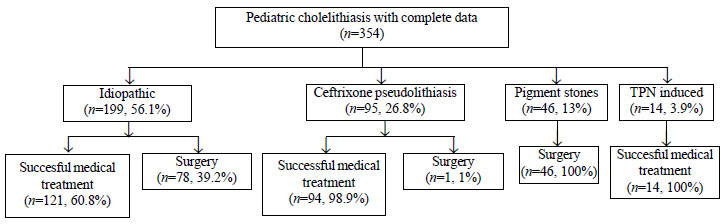
in the analysis (Fig. 1). Commonest (56.2%) etiology was
idiopathic; followed by ceftriaxone pseudolithiasis (26.83%).
The median (IQR) age was 6 (3-14) years. Incidence of obesity,
fast food habits, and biliary colic was highest in idiopathic
stones. Thirteen patients (13.7%) had a history of ceftriaxone
administration after abdominal surgery, associated with a
history of starvation for more than 48 hours. Most (45.8%)
patients were asymptomatic; non-specific abdominal pain was the
commonest (40.4%) symptom. The distribution of predis-posing
factors and symptoms among different etiologies is shown in
Table I. On ultrasound, the largest stone size was 2.5 cm,
and the mean size was not significantly different in all four
etiological types of cholelithiasis. Solitary stone was the
commonest (79.1%) presentation. Echogenic sludge without post
acoustic shadow was found in all cases of TPN-associated
cholelithiasis.
 |
|
Fig. 1 Treatment provided for
various types of pediatric cholelithiasis.
|
 |
| |
Pigment stones (n=46) were associated
with the highest rate of complications (Table I) and
underwent upfront elective cholecystectomy, planned
cholecystec-tomy, and emergent cholecystectomy (for gangrenous
cholecystitis) in 18, 22, and 6 patients, respectively. In
idiopathic pediatric cholelethiasis (39.2%) had to undergo
surgery because of biliary symptoms (37, 18.6%, elective
cholecystectomy), complications (34, 17.1%, 5 emergent
cholecystectomy), or failure of medical treat-ment in
asymptomatic pediatric cholelethiasis (7, 3.5%). Complications
viz. acute cholecystitis, chronic chole-cystitis and
choledocholithiasis were significantly higher in pigment stones
as compared to idiopathic stones (P=<0.001, P=0.02
and P=0.02, respectively). Medical management with UDCA
for 6 months was effective in 121 (60.8%) patients with
idiopathic cholelithiasis and all TPN-associated cases. TPN
stones were associated with the highest incidence of obstructive
jaundice. One patient underwent emergent cholecystec-tomy for
gall bladder perforation and biliary peritonitis. Gall-stone
pancreatitis was not seen in any patient.
DISCUSSION
Increasing prevalence of reversible
ceftriaxone-associated biliary pseudolithiasis is due to the
common use of ceftriaxone in children for abdominal infections
and peri-operatively in gastrointestinal surgery [5].
Ceftria-xone is excreted in bile where it gets 20-150 times
concentrated and readily forms a reversible insoluble salt with
calcium which precipitates into pseudo-stone formation [6].
Moreover, biliary stasis is known to occur in gastrointestinal
infection, starvation, after abdominal surgery, and
gram-negative sepsis [7]. History of admission for acute
gastroenteritis/dehydration or previous abdominal surgery with
the administration of ceftriaxone was common in our CP patients.
Compli-cations of cholelithiasis occur in 15-25% of pediatric
patients; hence, guidelines for expectant/medical/surgical
treatment are needed for its management [8,9]. Hemolytic stones
are advised cholecystectomy as the first line of treatment
because they do not respond well to medical dissolution therapy
and have a higher rate of complications due to impaction [8,10].
Ceftriaxone associated cholelithiasis and TPN induced pediatric
cholelithiasis, on the other hand, are known for their
reversible character and respond well to medical treatment [11].
UDCA is known to resolve PC in 19-37% of patients with
non-hemolytic stones [8,10,12]. Higher (60.8%) stone dissolution
with UDCA in the present study is unexplained.
Indications of cholecystectomy in idiopathic
pediatric cholelithiasis are less clear and the decision is
often based on clinical judgment, concerns for complications,
and the surgeons conviction (or lack of) in the efficacy of
UDCA [13]. In our study, 40% of idiopathic cholelithiasis
underwent surgery because of biliary symptoms or complications
or failure of medical treatment in asymptomatic patients;
supporting early surgery for symptomatic idiopathic stones. In
the present study, the majority of idiopathic and asympto-matic
idiopathic stones dissolved after medical treatment, suggesting
a specific role of medical therapy in avoiding surgery. However,
because of complications, medical treatment must be given under
close observation. An unnecessary cholecystectomy entails
needless risk and cost burden in a potentially dissolvable PC
[14]. Also, pediatric cholecystectomy is more challenging for
the surgeons because of its relative infrequency and the fact
that surgical volume might not help lower complication rates
[15]. The high incidence of ceftriaxone pseudo-cholelithiasis in
our study raises concerns about the common use of ceftriaxone in
pediatric practice. Awareness of this is important and
consideration should be given to the use of equivalent
antibiotic options.
Our algorithm (Web Fig. 1) allows a
pre-emptive approach to avert complications, the best
utilization of surgical options, and minimizes unnecessary
surgery. Formulation of our protocol is based on the analysis of
our data and lessons learned; it needs to be further tested in
different settings and in a prospective design.
Our etiology-based treatment protocol
developed with local data allows a judicious selection of
pediatric cholelithiasis patients for surgery. Hemolytic and
symptomatic stones warrant an early cholecystectomy.
Asymptomatic idiopathic stones, ceftriaxone stones, and
TPN-induced stones are candidates for medical therapy under
close observation.
Ethics approval: Netaji Subhash Chandra
Bose Medical College, Jabalpur, MP, India; No: IEC/NSCBMC/20/03,
dated September 27, 2020.
Contributors: VA, AT: concept, design,
definition of intellectual content, literature search, clinical
studies, data acquisition, data analysis, manuscript
preparation, editing and review; DS, RA: literature search,
clinical studies, data acquisition, data analysis, manuscript
preparation, editing, and review. All authors approved the final
version of the manuscript, and are accountable for all aspects
related to the study.
Funding: None; Competing interests:
None stated.
|
|
WHAT THIS STUDY ADDS?
An etiology-based decision-making protocol for
pediatric cholelithiasis is proposed based on our
experience.
|
REFERENCES
1. Poddar U. Gallstone disease in
children. Indian Pediatr. 2010;47:945-53.
2. Ganesh R, Muralinath S,
Sankarnarayanan VS, Sathiya-sekaran M. Prevalence of
cholelithiasis in children a hospital-based observation.
Indian J Gastroenterol. 2005; 24:85.
3. Frybova B, Drabek J, Lochmannova J, et
al. Cholelithiasis and choledocholithiasis in children; risk
factors for development. PLoS One. 2018;13: e0196475.
4. Khadilkar V, Yadav S, Agrawal KK, et
al. Revised IAP Growth Charts for Height, Weight and Body
Mass Index for 5- to 18-year-old Indian Children. Indian
Pediatr. 2015;52: 47-55.
5. Bor O, Dinleyici EC, Kebapci M,
Aydogdu SD. Ceftriaxone-associated biliary sludge and
pseudochole-lithiasis during childhood: A prospective study.
Pediatr. Int. 2004;46:322-4.
6. Park HZ, Lee SP, Schy AL. Ceftriaxone-associated
gallbladder sludge. Identification of calcium-ceftriaxone
salt as a major component of gallbladder precipitate.
Gastro-enterology 1991;100:1665-70.
7. Palanduz A, Yalcin I, Tonguc E, et al.
Sonographic assess-ment of ceftriaxone associated biliary
pseudolithiasis in children. J Clin Ultrasound.
2000;28:166-8.
8. Kirsaclioglu TC, Çakır CB, Bayram G,
Akbıyık F, Işık P, Tunç B. Risk factors, complications and
outcome of cholelithiasis in children: A retrospective,
single-centre review. J Paediatr Child Health.
2016;52:944-9.
9. Poffenberger CM, Gausche-Hill M, Ngai
S, Myers A, Renslo R. Cholelithiasis and its complications
in children and adolescents: update and case discussion.
Pediatr Emerg Care. 2012;28:68-76.
10. Noviello C, Papparella A, Romano M,
Cobellis G. Risk factors of cholelithiasis unrelated to
hematological disorders in pediatric patients undergoing
cholecystec-tomy. Gastroenterology Res. 2018;11:346-8.
11. Rodríguez DA, Orejarena AP, Diaz BM,
et al. Gallstones in association with the use of ceftriaxone
in children. Ann Pediatr (Barc). 2014;80:77-80.
12. Gökçe S, Yıldırım M, Erdogan D. A
retrospective review of children with gallstone: Single-center
experience from Central Anatolia. Turk J Gastroenterol.
2014;25: 46-53.
13. Gamba PG, Zancan L, Midrio P, et al.
Is there a place for medical treatment in children with
gallstones? J Pediatr Surg. 1997;32:476-8.
14. Akhtar-Danesh G, Doumouras AG, Bos C,
Flageole H, Hong D. Factors associated with outcomes and
costs after pediatric laparoscopic cholecystectomy. JAMA
Surg. 2018;153:551-7.
15. Kelley-Quon Li, Dokey A, Jen HC, Shew SB. Compli-cations
of pediatric cholecystectomy: Impact from hospital experience
and use of cholangiography. J Am Coll Surg. 2014;218:73-81.
|
|
|
 |
|

