|
|
|
Indian Pediatr 2018;55:
701-703 |
 |
Nebulized N-Acetylcysteine for Management of
Plastic Bronchitis
|
|
Animesh Kumar 1,
Kana Ram Jat1, M
Srinivas2 and
Rakesh Lodha1
From Departments of 1Pediatrics and 2Pediatric
Surgery, All India Institute of Medical Sciences, New Delhi, India.
Correspondence to: Dr Rakesh Lodha, Department of Pediatrics, All
India Institute of Medical Sciences, New Delhi 110029, India.
Email:
[email protected]
Received: February 03, 2017;
Initial review: June 19, 2017;
Accepted: April 23, 2018.
|
Background: Plastic bronchitis is
characterized by formation of extensive obstructive endobronchial casts
and high recurrence rates. Case characteristics: Two children
(1-year-old girl, 7-year-old boy) who had recurrent episodes of
respiratory distress with acute worsening. Bronchoscopy revealed
membrane-like casts. Both children were managed with nebulized N-acetylcysteine
in addition to management for asthma. Outcome: Symptom-free
without recurrence for more than 9 months of follow-up. Message:
Nebulized N- acetylcysteine may be helpful in prevention of recurrence
of plastic bronchitis due to asthma.
Keywords: Bronchial asthma, Bronchial casts, Foreign body,
Refractory.
|
|
P
lastic bronchitis, a condition characterized by
formation of casts in tracheobronchial tree, can lead to airway
obstruction and asphyxiation. It may affect all age groups [1] and is
mostly seen in post-cardiac surgery patients, especially Fontan
procedure [1-5]. The hallmark of the disease is expectoration of large
branching casts [5,6]. Clinical presentation is with acute onset
respiratory distress [3], productive cough [2-10], dyspnea, cyanosis,
and wheezing. Plastic bronchitis has been reported in association with
asthma [1], allergic bronchopulmonary aspergillosis, cystic fibrosis,
pulmonary tuberculosis, etc. The treatment is not well defined, and the
recurrence rates are high. We share our experience with two children who
had plastic bronchitis with asthma phenotype, and responded well to
nebulized N-acetylcysteine.
Case 1
A one-year-old girl presented with fever and cough
for 6 days followed by breathlessness for 2 days. Child had history
suggestive of recurrent episodes of acute respiratory infections since
the age of 4 months which were treated with oral antibiotics and
nebulized medications. On examination, child had tachypnea, lower chest
indrawing and reduced breath sounds in left hemithorax. Oxygen
saturation (SpO 2) in room
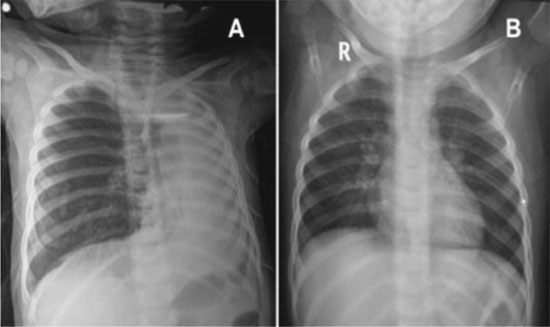
air was 84%, and Chest X-ray showed loss of lung volume on left
side (Fig. 1a). The child was administered oxygen
by a head box, and considering a possibility of foreign body aspiration,
the infant underwent rigid bronchoscopy. Procedure revealed dirty-white
membrane-like deposit fully occluding the left main bronchus. This
structure when removed had an appearance like the replica of bronchial
tree (Fig. 2). No foreign body could be found. The
post-operative chest X-ray showed some aeration of the left lung.
The child was weaned-off from ventilator after 48 hours. Chest X-ray
three weeks later showed complete expansion of left lung (Fig.
1b). Histopathology of cast revealed fibrin mucin with
numerous eosinophilic and neutrophilic infiltrates.
 |
|
Fig. 1 Chest X-ray of patient 1 at admission (a); and
at follow-up after three weeks (b).
|
 |
|
Fig. 2 Cast removed from left
bronchial tree of patient 1.
|
Sweat chloride test, bronchoalveolar lavage culture
of polymerase chain reaction for influenza virus, and lymphoscintigraphy
(for lymphatic malformations) were non-contributory. Post-procedure
child was managed with inhaled bronchodilators, N-acetylcysteine (1.5 mL,
20% solution) twice-a-day, chest physiotherapy and systemic steroids for
5 days. Child showed marked improvement with improvement in breath
sounds and SpO2 to 96% in
room air. Child was discharged on inhaled salbutamol (as and when
required), nebulized N-acetylcysteine (1.5 mL, 20% solution, twice a
day) and inhaled Budesonide 100 µg twice a day by metered dose inhaler
with spacer and face mask.
Child was followed-up every three months, and the
above mentioned treatment continued. At follow-up of 12 months, child
was asymptomatic.
Case 2
A 7-year-old boy presented with history of cough and
breathlessness for one week. He had recurrent cough, cold and
breathlessness every month since the age of 5 years. Each episode was
managed with inhaled bronchodilators, antibiotics and occasional
systemic steroids. For current episode of breathlessness, child received
inhaled bronchodilators, systemic steroids and supportive care. Due to
non-response and worsening hypoxia child underwent bronchoscopy twice
and membranous structures were removed. Child improved but continued to
have wheezing and mild respiratory distress. He presented to our
hospital at this stage; he was managed with supplemental oxygen
inhalation and nebulized bronchodilators. His X-ray and
high-resolution computed tomography of chest showed loss of left lung
volume. His blood counts, echocardiogram and immunoglobulin profile was
normal. Flexible bronchoscopy revealed membrane-like structures in left
bronchial tree; bronchoalveolar lavage (BAL) cultures were sterile.
We continued his treatment with inhaled
bronchodilator, inhaled budesonide (400 µg) with long-acting
beta-agonists and started nebulized N-acetylcysteine (2.5 mL 20%
solution) twice a day. There was significant improvement in cough,
wheezing and breathlessness. On inhaled budesonide 200 µg and nebulized
N-acetylcysteine twice a day, he was completely asymptomatic at 9-month
follow-up.
Discussion
Bronchial casts may be of two types: Type I
(inflammatory casts) characterized by acute presentation [2], associated
bronchial disease and fibrin/mucin [1] along with numerous eosinophilic
and neutrophilic infiltrates on histopathology; and Type II (Acellular
casts) associated with chronic and recurrent course, mostly seen in
cyanotic congenital heart diseases [2,3], and show mucin with few
mononuclear cells on histopathology [1].
Pathophysiology of plastic bronchitis in cardiac
patients include abnormality in lymphatic drainage, endobronchial lymph
leakage [1,5-6], elevated venous pressure, disruption of integrity of
bronchial mucosa, and leakage of proteinaceous material in the airway
[5,6]. In non-cardiac patients, the pathophysiology is constant
inflammation/irritation in the bronchial mucosa by allergens or
infective agents leading to induction of mucin hypersecretion by
inflammatory cytokines (goblet cell hyperplasia); finally thick mucinous
material casts and airway obstruction develop.
Plastic bronchitis had been treated with various
modalities along with optimal treatment of primary disease. In acute
condition, removal of casts with rigid bronchoscopy may be life-saving
[3]. Inhalational therapy using different agents – rhDNase in asthma,
rhDNase and acetylcysteine in cystic fibrosis, urokinase in cardiac
disease – has been useful in the prevention of recurrence [5,6,10].
Systemic therapy with corticosteroids and macrolides has been used in
cases where etiology is asthma/cystic fibrosis [6]. In post-cardiac
surgery cases, correction of hemodynamics and correction of lymphatics
leakage detected by dynamic contrast magnetic resonance lymphangiography
has been used successfully to treat the condition [9]. As the condition
is recurrent in nature, inhalational therapy with N-acetylcysteine may
be one modality of treatment to prevent the disease recurrence.
Acknowledgement: Dr SK Kabra for critical
revision and guidance.
Contributors: AK: literature search and wrote
manuscript draft; KRJ, MS: revised manuscript critically for important
intellectual content; RL: manuscript writing. All authors were involved
in management of the patient. All authors approved the final manuscript.
Funding: None; Competing interest: None
stated.
References
1. Seear M, Hui H, Magee F, Bohn D, Cutz E. Bronchial
casts in children: A proposed classification based on nine cases and a
review of the literature. Am J Respir Crit Care Med. 1997;155:364-70.
2. Eberlein MH, Drummond MB, Haponik EF. Plastic
bronchitis: A management challenge. Am J Med Sci. 2008;335:163-9.
3. Berlucchi M, Pelucchi F, Timpano S, Zorzi A,
Padoan R. A conservative treatment for plastic bronchitis in pediatric
age. Am J Otolaryngol. 2014;35:204-6.
4. Kim E, Park J, Kim D, Lee J. Plastic bronchitis in
an adult with asthma. Tuber Respir Dis. 2012;73:122-6.
5. Colaneri M, Quarti A, Pozzi M, Gasparini S,
Carloni I, de Benedictis F. Management of plastic bronchitis with
nebulized tissue plasminogen activator: another brick in the wall.
Italian J Pediatr. 2014;40:1-8.
6. Kunder R, Kunder C, Mark J, Berry G, Roth S,
Frankovich J, et al. Pediatric plastic bronchitis: case report
and retrospective comparative analysis of epidemiology and pathology.
Case Rep Pulmonol. 2013;2013:649365.
7. Turgut T, Ýn E, Özercan Ý, Kaplanmd M. A case of
plastic bronchitis. Arch Iranian Med. 2014;17:589-90.
8. Hasan R, Black C, Reddy R. Plastic bronchitis in
children. Fetal Pediatr Pathol. 2012;31:87-93.
9. Dori Y, Keller M, Rychik J, Itkin M. Successful
treatment of plastic bronchitis by selective lymphatic embolization in a
Fontan patient. Pediatrics. 2014;134:e590-5.
10. Mateos-Corral D, Cutz E, Solomon M, Ratjen F.
Plastic bronchitis as an unusual cause of mucus plugging in cystic
fibrosis. Pediatr Pulmonol. 2009;44:939-40.
|
|
|
 |
|

