|
|
|
Indian Pediatr 2018;55: 699-700 |
 |
Pulmonary Metastasis in Infantile
Choriocarcinoma: Successful Outcome
|
|
Ibrahim Kartal 1,
Ayhan Dagdemir1,
Murat Elli1 and
Meltem Ceyhan Bilgici2
From 1Division of Pediatric Hematology and
Oncology, Department of Pediatrics and Adolescent Medicine; and 2Department
of Radiology; Ondokuz Mayis University Medical Faculty, Samsun, Turkey.
Correspondence to: Dr Ibrahim Kartal, Division of
Pediatric Hematology and Oncology, Department of Pediatrics and
Adolescent Medicine, Ondokuz Mayis University Medical Faculty, Samsun,
Turkey.
Email:
[email protected]
Received: January 30, 2017;
Initial Review:June 19, 2017;
Accepted: May 10, 2018.
|
Background: Infantile choriocarcinoma is usually
fatal without appropriate treatment. Case characteristics: A
3-month-old boy who presented with respiratory distress, hepatomegaly,
amemia and bilateral nodular lesions on chest X-ray.
Observation: Fine-needle liver aspiration revealed necrotic tumour
cells. The serum b-hCG
level was very high (2057 mIU/L), supporting a diagnosis of infantile
choriocarcinoma of the liver. Surgical resection after cisplatin-based
multiagent chemotherapy afforded successful remission. Message:
Early treatment of infantile choriocarcinoma can yield a successful
outcome.
Keywords: Computed tomography, Diagnosis, Metastasis.
|
|
I nfantile choriocarcinoma is an
extremely rare disease characterized by severe anemia, failure to
thrive, hepatomegaly and seizures. Less commonly hemoptysis, respiratory
distress, and/or signs of precocious puberty may be evident. A marked
elevation in the b-hCG
level is typical (often to >106
IU/L) [1]. If not treated appropriately, death usually occurs within
three weeks of initial presentation [2]. Recently, multiagent
chemotherapy combined with surgical resection has yielded successful
outcomes [3]. We report a case of respiratory distress reflecting
pulmonary involvement of infantile choriocarcinoma.
Case Report
A 3-month-old boy was admitted to emergency
department of our hospital with a history of fever, fatigue (2 days in
duration), and cough (2 months in duration). He exhibited significant
respiratory distress, but no abnormal sounds were evident bilaterally on
auscultation. His liver was enlarged 6 cm below the costal margin.
Laboratory tests revealed a hemoglobin level of 7.5 g/dL, a platelet
count of 503.000/µL, a white blood cell count of 12.5 × 10 3/µL,
and a C-reactive protein level of 120 mg/L (normal, 0-5 mg/L). Aspartate
aminotransferase level was 103 IU/L, and chest X-ray revealed
bilateral, disseminated nodular lesions (Fig. 1). The
patient was admitted to the pediatric intensive care unit and
antibiotics (ceftriaxone and clarithromycin) were started to treat the
pneumonia.
 |
|
Fig. 1 Chest X-ray: Bilateral
pulmonary nodules evident at initial presentation.
|
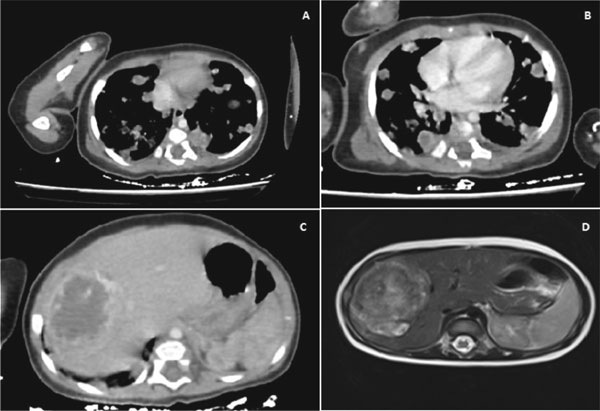
Thoracic computed tomography (CT) revealed multiple
small, bilateral pulmonary nodules (Fig. 2a, 2b)
and a mass of 49×63 mm in dimension, with indistinct cystic components,
in the right lobe of the liver (Fig. 2c). Magnetic
resonance imaging (MRI) identified an irregular heterogeneous mass
(50×60×60 mm) in the right lobe of the liver (Fig. 2d).
Fine-needle aspiration of the liver mass revealed necrotic tumor cells.
The serum a-hCG and alpha fetoprotein (AFP) levels were 2057 mIU/mL
(normal 0-25 mIU/mL) and 18 IU/mL, respectively, which suggested a
diagnosis of infantile choriocarcinoma of the liver. The mother’s
placenta was normal.
 |
|
Fig. 2 Bilateral pulmonary nodules on
computed tomography (a and b); hepatic mass in right lobe of
liver on computed tomography (c), and in magnetic resonance
imaging (d).
|
Chemotherapy was initiated with bleomycin (0.5 mg/kg;
1 day), cisplatin (0.7 mg/kg; 5 days) and etoposide (3 mg/kg; 5 days);
the BEP protocol. The patient tolerated six cycles of chemotherapy well.
Repeat testing of the a-hCG
level showed that it had decreased to <0.1 mIU/mL. Radiological
evaluation revealed no further evidence of metastatic lung disease.
Repeat CT showed a decrease in liver size; complete tumor resection was
achieved via right partial hepatectomy. Histopathological
examination revealed a few syncytiotrophoblasts and necrotic cells. The
child has been in complete remission for the past 3 years and remains
under regular follow-up. His growth and development are normal.
Discussion
Most cases of infantile choriocarcinoma are
metastases of gestational choriocarcinoma of the placenta, but primary
liver tumors have also been reported [4,5]. Choriocarcinoma can be
aggressive and destructive. Although relatively few cases have been
reported, they include cases cured with chemotherapy [3,6,7] .
The disease can rapidly become fatal if left
unrecognized. Of 30 cases reviewed by Blohm and Gobel [8], two were
diagnosed in stillborn children and 19 were diagnosed after death (on
postmortem examination). Among children who succumbed, the median time
from initial symptoms to death was 21 days. Such a rapid progression
indicates that treatment must not be delayed (to allow for histological
confirmation) in infants with a markedly elevated
a-hCG level and a
clinical presentation consistent with infantile choriocarcinoma. We
commenced multiagent chemotherapy in the absence of clear histological
evidence. It is recommended that all infants presenting with anaemia and
a hepatic mass be screened for a-hCG
levels [3].
Single-agent chemotherapy (methotrexate) usually
cures maternal gestational trophoblastic disease but has never been
curative in an infant with choriocarcinoma; multiagent chemotherapy is
required [9,10]. In the Blohm and Gobel series of 30 children [8], five
were successfully treated with a platinum compound (cisplatin or
carboplatin) combined with etoposide. In addition, because of the rapid
tumor growth, the platinum-plus-etoposide combination was often further
combined with methotrexate given for 1 week either before or after the
platinum-containing regimen. Surgical resection of the residual mass is
usually performed at the end of platinum-based therapy. Early surgical
intervention is not advisable; tumour fragility increases the risk of
uncontrolled bleeding, thus delaying chemotherapy [1]. The serum
b-hCG level is
an ideal marker for monitoring therapeutic success [8]. Although the
tumour is very aggressive, early cisplatin-based chemotherapy can yield
a successful outcome but must commence early.
Contributors: All authors were involved in
patient-management and manuscript-writing. Funding: None;
Competing Interest: None stated.
References
1. Frazier AL, Billmire D, Amatruda J. Pediatric Germ
Cell Tumors. In: Orkin SH, Fisher DE, Ginsburg D, Look AT, Lux
SE, Nathan DG, editors. Nathan and Oski’s Hematology and Oncology of
Infancy and Childhood. 8th ed. Philadelphia: Elsevier Health Sciences.
2014. p. 2082.
2. Timothy B, Nolting L. Cutaneous manifestation of
metastatic infantile choriocarcinoma. Case Rep Pediatr.
2014;2014:104652.
3. Hanson D, Walter AW, Dunn S, Rittenhouse DW,
Griffin G. Infantile choriocarcinoma in a neonate with massive liver
involvement cured with chemotherapy and liver transplant. J Pediatr
Hematol Oncol. 2011;33:e258-60.
4. Blohm ME, Calaminus G, Gnekow AK, Heidemann PH,
Bolkenius M, Weinel P, et al. Disseminated choriocar-cinoma in
infancy is curable by chemotherapy and delayed tumour resection. Eur J
Cancer. 2001;37:72-8.
5. Kim SN, Chi JG, Kim YW, Dong ES, Shin HY, Ahn HS,
et al. Neonatal choriocarcinoma of liver. Pediatr Pathol.
1993;13:723-30.
6. Szavay PO, Wermes C, Fuchs J, Schrappe M, Flemming
P, von Schweinitz D. Effective treatment of infantile choriocarcinoma in
the liver with chemotherapy and surgical resection: a case report. J
Pediatr Surg. 2000;35: 1134-5.
7. Yoon JM, Burns RC, Malogolowkin MH, Mascarenhas L.
Treatment of infantile choriocarcinoma of the liver. Pediatr Blood
Cancer. 2007;49:99-102.
8. Blohm ME, Göbel U. Unexplained anaemia and failure
to thrive as initial symptoms of infantil choriocarcinoma: a review. Eur
J Pediatr. 2004;163:1-6.
9. Johnson EJ, Crofton PM, O’Neill JM, Wilkinson AG,
McKenzie KJ, Munro FD, et al. Infantile choriocarcinoma treated
with chemotherapy alone. Med Pediatr Oncol. 2003;41:550-7.
10. Heath JA, Tiedemann K. Successful management of neonatal
choriocarcinoma. Med Pediatr Oncol. 2001;36:497-9.
|
|
|
 |
|

