reterm infants less than 32
weeks are incapable
of independent oral feeding and require gavage
feeds for a variable period of time after birth.
They frequently experience oral feeding difficulties due to
underdeveloped oral motor skills and lack of coordination of sucking,
swallowing and respiration [1,2]. Infant’s ability to consume all feeds
orally while maintaining physiologic stability and demonstrating weight
gain is necessary prior to discharge [3]. Beckman Oral Motor
Intervention (BOMI) is a 15-minute oral intervention for infants and
children with developmental delays and feeding difficulties but is not
suitable in preterm infants due to smaller oral cavity and longer
administration time [4]. The Premature Infant Oral Motor Intervention
(PIOMI) is a new intervention that is adapted from the BOMI to enhance
the premature infant’s ability to accept oral feeds [5]. The purpose of
this study was to determine efficacy of PIOMI as measured by a shorter
transition from gavage to full wati spoon feeds and shorter
duration of hospital stay.
Methods
This randomized controlled study was conducted in the
neonatal unit of a tertiary care centre over 3 months from March-May
2014, following approval from our institutional ethics committee. All
infants admitted to the unit and born between 28 to 32 weeks gestational
age, once medically stable with no respiratory support for atleast 48
hours and on full gavage feeds of 150cc/kg/day, were eligible for
enrollment into the study. Infants having respiratory distress and those
with chronic medical complications like BPD, IVH, PVL, NEC, chromosomal
anomalies or craniofacial malformation were excluded from the study.
Written informed consent was taken prior to enrollment.
Infants meeting eligibility criteria were randomized
to receive oro-motor stimulation using either Premature Infant Oro-Motor
Intervention (PIOMI) or sham intervention. Randomization was done using
a computer generated randomization sequence placed in sealed, opaque,
sequentially numbered envelopes. The physician on call opened the
sequentially numbered sealed opaque envelopes and randomized infants to
the respective groups. The principal investigator underwent a training
for this oro-motor intervention in the department of occupational
therapy for 15 days prior to the start of the study regarding correct
order of steps in the protocol with correct technique and time spent at
each step. Intervention in both the groups was done by the principal
investigator and duration did not exceed 5 minutes in either group.
Infants randomized to PIOMI group were subjected to 5
minutes of PIOMI intervention three times daily for 7 consecutive days
using all aseptic precautions with gloved fingers. The PIOMI is a
5-minute oral motor intervention that provides assisted movement to
activate muscle contraction and provides movement against resistance to
build strength [5]. Sham intervention consisted of unstructured stroking
procedure done in and around the oral cavity of the infants.
Baseline oromotor evaluation was done in both the
groups by a trained occupational therapist who had considerable
experience of working in the neonatal unit and handling preterm babies.
This occupational therapist was blinded to the group allocation and
evaluation was done with a scale known as Neonatal Oro motor Assessment
Scale (NOMAS) [6]. Maximum total score in NOMAS is 48 and higher score
in NOMAS indicated better oro motor skills [7]. A repeat evaluation was
again done by the same therapist after 7 days of intervention to
eliminate inter-observer bias.
Primary outcome of the study was the improvement in
the NOMAS score after 7 days of intervention. Secondary outcomes
included transition time to reach full independent wati spoon feeds,
duration of hospital stay and weight gain after intervention.
Study done by Fucile, et al. [8] had shown
improvement in oro-motor skills with pre-feeding intervention. A sample
size of 32 babies with 16 in each group was based on detecting a
difference of 5 in NOMAS score between the PIOMI and the SHAM
intervention group using a two sided alpha error of 0.05, beta error of
0.2 (power 80%) and a standard deviation of 5.
Statistical analysis: Baseline characteristics
and outcome measures on continuous scales were analyzed by using two
sample t test. Statistical analysis was performed by applying
intention to treat principle and P<0.05 was considered
statistically significant.
Results
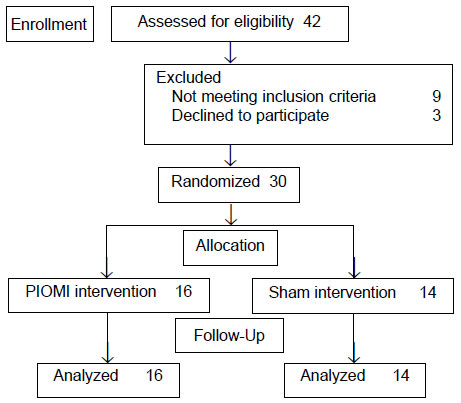
A total of 76 preterm infants less than 32 weeks were
admitted in the unit during the 3 month study period out of which 42
were assessed for inclusion. Out of them, 30 were included in the study
with 16 in PIOMI group and 14 in the sham intervention group (Fig.
1). The baseline demographic characterstics of the enrolled infants
were similar (Table I).
 |
|
Fig. 1 Flow of participants in the
study.
|
TABLE I Baseline Characteristics of Infants in Two Study Groups
|
Variables |
PIOMI |
SHAM |
|
intervention |
intervention |
|
(n=16) |
(n=14) |
|
#Gestation age (w) |
30 (0.9) |
30.5 (0.6) |
|
#Birthweight (g) |
1040.0 (120.6) |
1063.6 (79.5) |
|
Males |
8 (50.0) |
8 (57.1) |
|
Antenatal Steroids received |
13 (81.2) |
9 (64.3) |
|
Requirement of resuscitation |
5 (35.7) |
6 (42.8) |
|
RDS |
9 (64.2) |
10(71.4) |
|
Culture positive sepsis |
6 (37.5) |
4 (28.5) |
|
Mechanical ventilation |
6 (37.5) |
3 (21.4) |
|
Non-invasive ventilation |
11 (68.7) |
12 (85.7) |
|
#Trophic gavage feeds (d) |
3.7 (1.4) |
3.4 (1.6) |
|
#Full oro-gastric feeds (d) |
15.6 (4.2) |
14.8 (5.1) |
|
#Age at enrolment (d) |
17.1 (4.5) |
16.1 (4.7) |
|
#Weight at enrolment (g) |
1041.8 (108.6) |
1067.9 (76.5) |
|
NOMAS score at enrolment |
27.1 (2.2) |
28.6 (2.2) |
|
Values in n(%) except #Mean
(SD); RDS: Respiratory distress syndrome; NOMAS: Neonatal oral
motor assessment scale. |
Improvement in mean (SD) NOMAS score over 7 days from
baseline was also highly significant in the study group infants as
compared to control group [9.25 (1.73) vs 4.79 (1.52), P<0.001).
Infants in the study group reached full wati spoon feeds
significantly earlier than the infants in control group. There was a
statistically significant increase in weight gain after enrolment in
infants in study group than infants in control group. However, there was
no significant difference in terms of hospital stay after enrolment, age
at discharge, weight gain after enrolment and weight at discharge (Table
II).
TABLE II Study Outcomes in the Two Groups
|
Outcomes |
PIOMI GP(n=16) |
SHAM GP(n=14) |
Risk difference (95 % CI) |
P value |
|
Improvement in NOMAS score |
9.3 (1.7) |
4.8 (1.5) |
4.5 (3.2 to 5.6) |
<0.001 |
|
Transition time to reach full feeds (d) |
4.0 (0.8) |
6.6 (1.0) |
-2.6 (-3.3 to -1.9) |
<0.001 |
|
Hospital stay after enrolment (d) |
13.6 (4.8) |
16.1 (4.0) |
-2.5 (-5.8 to 0.8) |
0.13 |
|
Age at discharge (d) |
30.5 (8.4) |
31.3 (5.4) |
-0.8 (-6.1 to 4.5) |
0.76 |
Discussion
This randomized control trial showed that pre-feeding
intervention with PIOMI is effective in improving the oro-motor function
of the preterm infants.
The major limitation of our study was it being a
single center study with a small sample size. We have evaluated PIOMI
intervention based on NOMAS score instead of feeding efficacy assessment
based on volume and rate of total milk intake at each feed and time to
start sucking from breast. Due to infrastructure constraints, infants in
our study were discharged once they were on full wati spoon feeds
and thus, the effect of intervention on attaining full breast feeds
could not be seen.
Gaebler and Hanzlik [9] had demonstrated that infants
receiving a peri- and intra-oral stimulation just before oral feedings
scored better on the NOMAS which was also confirmed in our study.
Another study demonstrated that the PIOMI was well tolerated by 29-week
PMA infants [5]. We have not seen any unfavorable response in preterm
infants who received the thrice-daily PIOMI intervention for 5 minutes.
It is necessary to limit any form of intervention to a five minute time
frame in preterm infants to reduce the likelihood of the infant
experiencing negative physiological and behavioral effects due to a
prolonged duration of stimulation.
We found early transition from tube to full
independent oral feeds which was also reported in earlier studies
[8,10]. A recent study by Bala, et al. [11] had also shown that
oromotor stimulation decreases the duration of gavage feeding. There was
a significant increase in weight-gain per day after enrolment in infants
in PIOMI group than infants in sham intervention group. An enhanced
sucking rate with stroking of the cheeks and increase in volume intake
during an oral feeding session has also been earlier reported [12,13].
Infants in our study group had a shorter hospital stay as compared to
control group, but the difference was not statistically significant.
In conclusion, our study supports the hypothesis that
5-minute PIOMI three times daily for seven days for preterm infants
between 28 to 32 weeks of gestational age significantly improves their
oro-motor skills. It was effective in reducing transition time from
gavage to oral feeds and infants had increased weight gain with shorter
duration of hospital stay. Larger randomized controlled trials with a
longer follow-up are needed to confirm the benefits seen in our study,
and to further evaluate the effect on time to hospital discharge as a
primary outcome.

