|
|
|
Indian Pediatr 2017;54: 678 -680 |
 |
Emergency Surgery for
Refractory Status Epilepticus
|
|
*Abhijeet Botre, *Vrajesh Udani, *Neelu Desai,
Spoorthy Jagadish and #Milind
Sankhe
From Departments of Pediatrics, *Pediatric Neurology
and #Neurosurgery, PD Hinduja Hospital and Research
Centre, Mumbai, India.
Correspondence to: Dr Neelu Desai, Pediatric
Neurologist, PD Hinduja Hospital & MRC, Veer Savarkar Marg, Mahim,
Mumbai 400 016, India. Email:
[email protected]
Received: July 12, 2016;
Initial Review: November 02, 2016;
Accepted: May 27, 2017
|
Background: Management of refractory status epilepticus in children
is extremely challenging. Case characteristics: Two children with
medically refractory status epilepticus, both of whom had lesional
pathology on MRI and concordant data on EEG and PET scan.
Intervention: Emergency hemispherotomy performed in both patients. A
complete, sustained seizure freedom obtained postoperatively. Message:
Emergency surgery is a treatment option in selected cases of drug
refractory status epilepticus with lesional pathology and concordant
data.
Keywords: Management, Outcome, Super-refractory status
epilepticus.
|
|
S
tatus epilepticus is a serious medical emergency
in pediatric practice with a potential for significant morbidity and
mortality. Almost 30-40% of SE is refractory to first and second line
treatment and needs coma producing therapy for controlling seizures
[1,2]. Subsets of these patients do not respond to coma therapy too and
are considered to be super-refractory. Treatment of this
super-refractory status epilepticus is extremely challenging with scant
literature on effective therapies. In selected cases and at experienced
centres, epilepsy surgery could be considered as a therapeutic option
once medical management has failed [3-5].
We describe two children with medically refractory
status epilepticus (RSE) due to lesional pathology in brain, who
responded well to emergency epilepsy surgery.
Case 1
A 4.5-month-old boy was referred for neonatal onset
drug-resistant epilepsy. Seizures started from 15 days of life in the
form of flexor spasms. Initially infrequent, these events later
increased to daily jerks which responded transiently to Inj. ACTH and
oral topiramate. At this time, his developmental milestones and
examination was normal. A brain MRI done elsewhere showed a right
hemispheric cortical dysplasia. An EEG showed predominantly right
hemispheric epileptiform discharges.
At one year of age, he came back with progressively
increasing flexor spasms since 7 months of age. He also had significant
left hemiparesis. An option of hemispheric surgery was declined by the
parents. He responded to the ketogenic diet and was also continued on
multiple anticonvulsants. A month later, he was referred from a local
hospital after developing status epilepticus.
The infant had generalized convulsive seizures and
was deeply comatose on admission. Seizures persisted despite multiple
antiepileptic drugs and midazolam infusion. Video-EEG showed
predominantly right sided ictal as well as interictal epileptic
discharges and right sided burst-suppression pattern. A repeat cranial
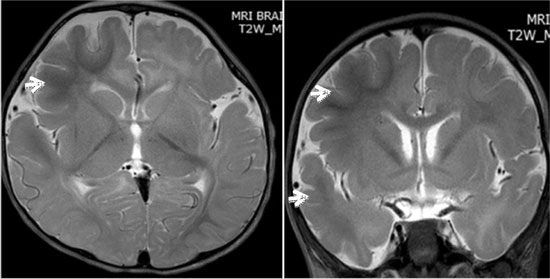
MRI confirmed the right hemispheric cortical dysplasia (Fig 1).
A FDG-PET scan showed increased metabolism in the right hemisphere
suggestive of ongoing ictal activity.
(a)
(b) |
|
Fig.1 Brain MRI T2 weighted axial (a)
and coronal images (b) of case 1 showing the right hemispheric
dysplasia seen as fronto-temporal hypermyelination (hypointense
white matter)- hallmark of dysplasia in infancy.
|
An emergency right hemispherotomy was done after 10
days of uncontrolled status epilepticus. Histopathology confirmed the
diagnosis of cortical dysplasia. Post-operative course was uneventful.
Seizures stopped completely and the child remained seizure-free for next
6 months on three antiepileptic drugs (Topiramate, Sodium Valproate and
Leviteracetam). Seizure recurred after 6 months due to presence of
incomplete disconnection at the temporal stem as revealed by the
tractography; hence, a second surgery was done for complete
disconnection. Child remains seizure-free at 24 months post-operative
follow up. He is gaining milestones and can stand independently though
his left hemiparesis persists.
Case 2
A 7-year-old boy presented with a history of
right-sided brief, focal motor seizures from the age of 4 years
following an encephalitis-like illness. The seizures occurred once in
8-10 days but frequency had increased recently to daily events
associated with transient right sided Toddís paralysis. A poor right
hand grip was noticed since last few months. He had failed trials of
multiple antiepileptic drugs.
The child was admitted in March 2015 with worsening
seizures, which later evolved during hospital stay to a status
epilepticus. His video-EEG showed clinical as well as subclinical
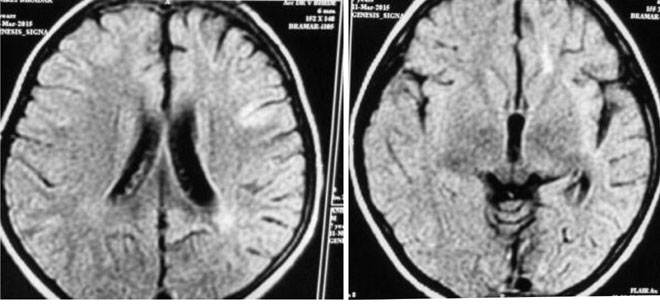
seizures arising from the left temporal region. Repeat brain MRI showed
progressive left cerebral atrophy with thinning of left putamen and
ill-defined patchy T2 hyperintensities in left frontal and peri-insular
cortex suggestive of Rasmussenís encephalitis (Fig 2). An
emergency hemispherotomy was performed after 7 days. Histopathology
confirmed the diagnosis of Rasmussenís encephalitis. Seizures stopped
completely after surgery and the child remains seizure-free at 12 months
follow up. He has started speaking and is ambulant.
 |
|
Fig. 2 Brain MRI showing progressive
left cerebral atrophy and ill-defined patchy T2 hyperintensities
in left hemisphere in second patient.
|
Discussion
In both cases, RSE with lesional etiology and
concordant data, emergency surgery was done for seizure-control. Similar
approach has also been used previously as a treatment of RSE [3,4]. The
published evidence-base consists of 36 patients reported in 15 small
series and case reports, and the surgeries included focal cortical
resection, lobar and multi-lobar resection, anatomic and functional
hemispherectomy, corpus callosotomy and multiple subpial transactions
[4].
Surgery has been carried out as early as 8 days after
the onset of RSE but generally considered only after weeks of SE [3].
Hemispherectomy and hemispherotomy are routinely used for intractable
hemispheric epilepsies, with good seizure control in 50-85% [6-9].
Seizure-free rate is highest in infantile hemiplegia syndromes and
Rasmussenís encephalitis [7].
Over the last decade, newer less invasive
disconnection techniques of hemispherotomies appear to achieve
postoperative seizure control which is comparable to anatomical and
functional hemispherectomies, with a significantly lower rate of
complications [9]. This could be potentially life-saving procedure for
RSE. In addition there is better postoperative developmental outcome
[6]. Our experience with hemispheric surgeries has been previously
detailed [10].
In conclusion, emergency epilepsy surgery is a
therapeutic option in RSE in selected cases and at experienced centres,
once medical management has failed. Hemispherotomy is a surgical
procedure of hemispheric disconnection which seems to be safe even in
infants as demonstrated in our case.
Contributors: AB: collected the case details and
prepared the initial draft; VU: managed the patient and supervised the
draft; ND: designed the concept and overviewed literature; SJ: helped in
data collection and patient management; MS: managed the patient and
supervised the discussion.
Funding: None; Competing interest: None
stated.
References
1. Gilbert DL, Gartside PS, Glauser TA. Efficacy and
mortality in treatment of refractory generalized convulsive status
epilepticus in children: a meta-analysis. J Child Neurol 1999;14:602-9.
2. Sahin M, Menache CC, Holmes GL, Riviello Jr.
Outcome of severe refractory status epilepticus in children. Epilepsia.
2001;42:1461-7.
3. Alexopoulos A, Lachhwani DK, Gupta A, Kotagal P,
Harrison AM, Bingaman W, et al. Resective surgery to treat
refractory status epilepticus in children with focal epileptogenesis.
Neurology. 2005;3:567-70.
4. Bhatia S, Ahmad F, Miller I, Ragheb J, Morrison G,
Jayakar P, et al. Surgical treatment of refractory status
epilepticus in children: clinical article. J Neurosurg Pediatr.
2013;4:360-6.
5. Ng YT, Kerrigan JF, Rekate HL. Neurosurgical
treatment of status epilepticus. J Neurosurg. 2006; 105:378-81.
6. Ramantani G, Kadish NE, Brandt A, Strobl K, Stathi
A, Wiegand G, et al. Seizure control and developmental
trajectories after hemispherotomy for refractory epilepsy in childhood
and adolescence. Epilepsia. 2013;54:1046-55.
7. Thomas SG, Chacko AG, Thomas MM, Babu KS, Russel
PS, Daniel RT. Outcomes of disconnective surgery in intractable
pediatric hemispheric and subhemispheric epilepsy. Int J Pediatr. 2012;
527891.
8. Terra-Bustamante VC, Inuzuka LM, Fernandes RM,
Escorsi-Rosset S, Wichert-Ana L, Alexandre V Jr, et al. Outcome
of hemispheric surgeries for refractory epilepsy in pediatric patients.
Childs Nerv Syst. 2007;23:321-6.
9. Kwan A, Ng WH, Otsubo H, Ochi A, Snead OC 3rd,
Tamber MS, et al. Hemispherectomy for the control of intractable
epilepsy in childhood: comparison of two surgical techniques in a single
institution. Neurosurgery. 2010;67:429-36.
10. Shah R, Botre A, Udani V. Trends in pediatric epilepsy surgery.
Indian J Pediatr. 2015;82:277-85.
|
|
|
 |
|

