|
|
|
Indian Pediatr 2017;54: 652-660 |
 |
Consensus Guidelines on Evaluation and
Management of the Febrile Child Presenting to the Emergency
Department in India
|
|
*Prashant Mahajan,
#Prerna Batra,
$Neha Thakur,
‡Reena Patel, ^Narendra
Rai, £Nitin
Trivedi, @Bernhard
Fassl, **Binita Shah, ##Marie
Lozon, $$Rockerfeller
A Oteng, ‡‡Abhijeet
Saha, #Dheeraj
Shah and @@Sagar
Galwankar;
for Academic College of Emergency
Experts in India (ACEE-INDIA) – INDO US Emergency and Trauma
Collaborative
From *Departments of Emergency Medicine and
Pediatrics, University of Michigan (Ann Arbor, MI, USA); #Department
of Pediatrics, University College of Medical Sciences and Guru Teg
Bahadur Hospital, Delhi, India; $Department of Pediatrics,
Hind Institute of Medical Sciences, Lucknow, India; ‡Department
of Pediatrics, Division of Inpatient Medicine, University of Utah, (Salt
Lake City, UT, USA); ^Department of Pediatrics, Hind
Institute of Medical Sciences, Lucknow, India; £Department of
Pediatrics, Mahatma Gandhi Medical College and Hospital, Jaipur, India;
@Department of Pediatrics; Division of Inpatient Medicine and
Department of Epidemiology and Biostatistics, University of Utah, (Salt
Lake City, UT, USA); **Departments of Emergency Medicine and Pediatrics,
SUNY Downstate Medical Center, Kings County Hospital Center (Brooklyn,
NY, USA); ##Department of Emergency Medicine, University of
Michigan, (Ann Arbor, MI, USA); $$Department of Emergency
Medicine, University of Michigan (Ann Arbor, MI, USA) and Directorate of
Emergency Medicine, KomfoAnokye Teaching Hospital (Kumasi, Ghana); ‘‡‡Department
of Pediatrics, Lady Hardinge Medical College, New Delhi, India; and
@@ Department of Emergency Medicine, University of Florida,
(Jacksonville, FL, USA).
Correspondence to: Dr Prashant Mahajan,
CS Mott Children’s Hospital, University of Michigan 1540 East Hospital
drive, Room 2-737, SPC 4260, Ann Arbor, MI 48109-4260, USA.
Email: [email protected]
Received: October 11, 2016;
Initial Review: January 11, 2017;
Accepted: May 25, 2017.
Published online: June 04, 2017.
PII:S097475591600069
|
|
Justification: India, home to
almost 1.5 billion people, is in need of a country-specific,
evidence-based, consensus approach for the emergency department (ED)
evaluation and management of the febrile child.
Process: We held two consensus
meetings, performed an exhaustive literature review, and held ongoing
web-based discussions to arrive at a formal consensus on the proposed
evaluation and management algorithm. The first meeting was held in Delhi
in October 2015, under the auspices of Pediatric Emergency Medicine
(PEM) Section of Academic College of Emergency Experts in India
(ACEE-INDIA); and the second meeting was conducted at Pune during
Emergency Medical Pediatrics and Recent Trends (EMPART 2016) in March
2016. The second meeting was followed with futher e-mail-based
discussions to arrive at a formal consensus on the proposed algorithm.
Objective: To develop an
algorithmic approach for the evaluation and management of the febrile
child that can be easily applied in the context of emergency care and
modified based on local epidemiology and practice standards.
Recommendations: We created an
algorithm that can assist the clinician in the evaluation and management
of the febrile child presenting to the ED, contextualized to health care
in India. This guideline includes the following key components: triage
and the timely assessment; evaluation; and patient disposition from the
ED. We urge the development and creation of a robust data repository of
minimal standard data elements. This would provide a systematic
measurement of the care processes and patient outcomes, and a better
understanding of various etiologies of febrile illnesses in India; both
of which can be used to further modify the proposed approach and
algorithm.
Keywords: Consensus statement, Diagnosis,
Fever, Infection, Sepsis.
|
|
A
ll over the world, fever in children is one of
the most common reasons for parents to seek medical care. It is
estimated that approximately 20% of all pediatric emergency department
(ED) visits in the United States (US) are for evaluation of fever [1].
In recent decades, an extensive amount of literature and evidence has
led to a consensus approach to the evaluation and management of febrile
children; which has evolved secondary to its changing epidemiology. The
change in epidemiology of the febrile child is the result of the
substantial impact of conjugate vaccines against capsulated bacterial
pathogens including H. influenzae and S. pneumoniae
[1].
To reduce variation, multiple guidelines have been
proposed including those from academic societies such as the American
Academy of Pediatrics (AAP) and American College of Emergency Physicians
(ACEP) [2]. Despite some differences, most guidelines advocate a
comprehensive evaluation of the very young febrile infant (28 days and
younger) and a less conservative approach for older infants. Febrile
infants undergo invasive procedures such as lumbar puncture, complete
blood counts and urinalysis. Most febrile infants, especially those less
than 28 days of age, are routinely hospitalized and treated empirically
with broad spectrum antibiotics such as third generation cephalosporins
along with ampicillin.
There continues to be practice variation also, when
applying evidence and consensus-based guidelines [3-5]. Depending upon
clinician suspicion, clinicians may evaluate for etiologies as variable
as bacterial pneumonia and bacterial enteritis. Currently available
"standardized" approaches, regardless of practice variation, remain
problematic for various reasons: (i) prediction rules and/or
guidelines have not been validated across cultural, geographic,
socio-economic environments and may not be applicable in all clinical
settings; (ii) the epidemiology of pathogens causing Serious
Bacterial Infection (SBI) has changed due to the impact of conjugate
vaccines; (iii) clinicians are not confident about the test
characteristics of various screening tools, especially the
discriminatory abilities of the complete blood counts, and finally; (iv)
newer screening tools such as procalcitonin have not been studied or
integrated into clinical decision making in a robust manner.
Evaluation and management of the febrile child in
India: Children may present with fever as an initial/isolated
symptom of a yet undifferentiated illness or with localizing signs that
suggest an etiology such as pneumonia. A majority of children with fever
without localizing signs will have a viral etiology which does not
warrant laboratory evaluation and can often be managed with instructions
for ensuring adequate hydration and use of antipyretics [6]. In one
study it is estimated that up to 10% of febrile children, especially
those 3 months of age and younger will have bacterial illnesses in the
form of occult bacteremia, septicemia, bacterial meningitis, pneumonia,
UTI, bacterial gastroenteritis, osteomyelitis, septic arthritis, and
other general endemic tropical diseases [7]. However, etiologies of
fever in the Indian ED context could vary from benign viral illnesses,
commonly reported in US and Europe (e.g. respiratory syncytial
virus (RSV), Enterovirus infections) to illnesses by organisms uncommon
in industrialized countries: bacteria (e.g. S. typhi),
viruses (e.g. measles, dengue, chikungunya) and parasites
(e.g. malaria, kala azar) as well as endemic illness outbreaks
due to meningococci and leptospira.
India is a tropical country with a distinct spectrum
of common tropical illnesses particularly seen in post-monsoon season
such as dengue, rickettsial infections, scrub typhus, malaria (usually
due to Plasmodium falciparum), typhoid and leptospirosis [8]. Thus, the
algorithmic approach utilized in the US and Europe is not applicable in
Indian EDs, especially when evaluating a child with fever without
source.
Emergency medicine is a growing medical specialty as
evidenced by the rising number of publications appearing in the
peer-reviewed literature demonstrating its growth and influence on
healthcare delivery in India [9]. In conjunction with emergency
medicine, as well as independently, pediatric emergency medicine is
rapidly evolving as a sub-specialty and efforts are underway for its
formal specialty status recognition [10]. Development of a consensus
statement that is relevant to the epidemiology of illness in the Indian
context will help reduce practice pattern variation, optimize resource
allocation as well as education, training and decision-making by both
policy makers and health care administrators in the federal, public and
private sectors.Moreover, evaluation and management of the febrile
child, continues to remain a clinical challenge in the Indian ED context
and the development of a consensus based practice guideline will serve
as a valuable resource.
Process
We held two consensus meetings of Pediatric Emergency
Medicine (PEM) Section of Academic College of Emergency Experts in India
(ACEE-INDIA) in Delhi (October 2015) and in Pune (March 2016). An
exhaustive literature review was performed and ongoing web-based
discussions were held to arrive at a consensus on the proposed
evaluation and management of febrile infants and children. We provide a
pragmatic and simple to use algorithm that will assist, but not
replace, clinician decision making for the ED evaluation and management
of the febrile child.
We have identified the key concerns regarding a
standardized approach to the evaluation and care of the febrile child in
an ED in India (Box 1).
|
BOX 1 Key Concerns in Case of the Febrile
Child in an Indian Emergency Department
• Epidemiology of the febrile child in India
is different from that of the Western Countries; published
guidelines will require further modification for them to be
applicable to the Indian ED context.
• The ill-appearing febrile child will need a
separate approach with the goal of early recognition of
impending cardiovascular and respiratory compromise regardless
of underlying etiology.
• Other aspects such as ongoing epidemics (e.g.,
dengue) or co-existing co-morbid conditions (e.g.,
malnutrition) should be part of the approach.
• There is no wide-spread, comprehensive data
available to systematically report the epidemiology of febrile
illnesses that present to the EDs across the country.
• Approach considerations for
resource-replete vs. resource-constrained settings is
important. Consensus among experts was that with respect to
medical interventions, clinical practice guidelines should
ideally be applicable in all settings.
|
Literature Review: Following the initial
consensus meeting, an exhaustive review of available literature
pertaining to each component was identified. We used structured queries
including terms such as fever, febrile child, febrile infant, fever
without source, serious bacterial infection, bacteremia, to search
databases including Pubmed, Google scholar to develop a comprehensive
database of peer reviewed literature in an Endnote file. These
manuscripts along with textbook chapters on the febrile child in
commonly accepted textbooks of pediatrics and pediatric emergency
medicine were reviewed. The literature review included topics unique to
the India based ED setting: fever in immunocompromised and/or severely
malnourished children, fever with localization, fever without
localization and etiologies specific to our country like malaria,
dengue, and enteric infections. A drafting committee was selected to
synthesize the literature and key concerns outlined at the initial
in-person meeting. Drafts were circulated electronically to engage and
further solicit input. This process resulted in specific evaluation and
management recommendations for each condition.
Recommendations
Considering the available literature and the needs
identified by the expert panel, we created an algorithm for the
evaluation and management for a febrile child presenting to the ED
within the context of healthcare in India (Fig. 1).
This algorithmic approach incorporated the following: localizing
symptoms, epidemiologic evidence, physiologic state (i.e.
immunocompromised or not; well appearing or ill appearing), duration of
fever, and age of the child. For the purposes of algorithm application,
we have outlined terms, definitions and categories below.
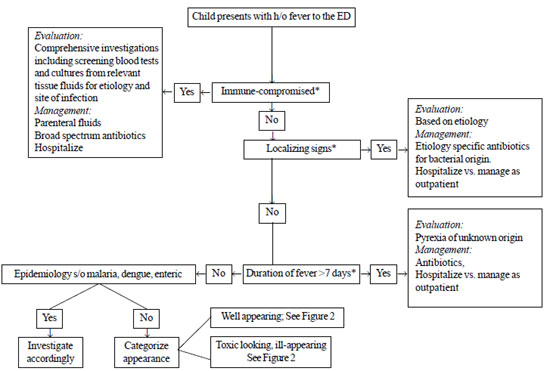
*Child could be ill or well appearing – please see Fig. 2 for
further management of ill- and well-appearing Child.
|
|
Fig. 1 Algorithm for evaluation and
management for the febrile child presenting to Emergency
department within the context ot health care in India.
|
Definition of fever: Fever is defined as a
rectal temperature ³38.0ºC
or ³100.4ºF
[1,11]. Axillary temperature is 0.3-0.6ºC
lower than the rectal temperature. Patients often present to the ED with
subjective fever at home, felt by tactile assessment only. In this
scenario, we suggest that clinicians obtain a detailed history including
association with lethargy, perspiration, irritability or other
concerning symptoms for ascertainment of clinically relevant fever and
before providing a disposition.
Method of temperature assessment: Axillary
thermometry is the most widely used method in clinical practice;
however, axillary thermometers are not reliable with regards to
measuring body temperature in infants and children [12]. Rectal
temperature was identified as the most accurate measurement as it is
closest to the core body temperature [1,13] and is the preferred method
of temperature determination in very young children. Temporal artery and
tympanic membrane thermometers can be used for quick assessment of
temperature [14], provided the clinician is aware of the limitations and
performance characteristics of each method. Further, based on the
clinical situation, one must confirm the core temperature by the rectal
route. No definite cut-offs have been given for defining fever using
tympanic and temporal thermometers.
Triage: A prompt and rapid clinical assessment by
trained providers should be performed at triage [15,16]. Vital signs
(temperature, heart rate, respiratory rate, blood pressure, and pulse
oximetry) measurement along with the use of pediatric assessment
triangle and/or Pediatric Early Warning Scores (PEWS) to quantify
severity of illness is highly recommended to help categorize the febrile
child as well- appearing or ill- appearing [17]. Providers (health
workers, nurses and physicians) should be trained in performance of
these assessments reliably and perform them in a timely manner. All
febrile children who appear to be at risk for cardio-pulmonary
compromise and septic shock should have life-saving resuscitative
procedures performed regardless of etiology of fever. These include
obtaining vascular access (either intravenous or intraosseous), managing
the airway with provision of oxygenation and placing the child on a
cardiac monitor. If such resources are available, a bedside glucose test
along with a capillary blood gas, point-of-care serum electrolytes,
ionized calcium and lactate levels should be performed to guide
resuscitation. Provision of broad-spectrum antibiotics to treat
suspected bacterial pathogens should also be provided as rapidly as
possible. If patient is in shock, management with rapid and adequate
amounts of isotonic fluids should be initiated. Table I
summarizes the identification and immediate management of emergent
patients. Immediate treatment steps should be initiated by healthcare
personnel and often can be initiated at triage.
TABLE I Identification and Immediate Management of Emergent/Life-Threatening Conditions
|
Symptoms/Signs |
Immediate treatment |
After stabilization
|
|
Airway and breathing |
|
•Airway obstruction |
1.Secure and clear airway
|
1.Blood glucose – correct immediately with D25 2cc/kg |
|
•Cyanosis |
2.Provide bag and mask ventilation |
|
|
•Respiratory distress |
3.Intubate if ongoing respiratory support is needed.
|
2.Hemogram |
|
•Respiratory failure Circulation |
4.Give oxygen:Nasal Cannula 2-3 LPM or Face Mask 5 LPM |
3.Blood gas
|
| |
|
4.Electrolytes
|
|
•Heart rate |
1.Establish intravenous (IV) or intraosseous line (IO) line |
5.Peripheral smear for malaria parasites if indicated |
|
•Capillary refill time |
2.Give isotonic fluid bolus if clinically indicated |
|
|
•Pulses(bounding or weak) |
3.Continued assessment for signs of shock and cardiovascular
compromise |
6.Specific investigatons as |
|
•Blood pressure |
|
indicated for instance blood
|
|
•Urine output
|
|
group type and cross match,
|
|
•Level of consciousness |
|
toxicologic screens in blood and
|
|
CNS |
|
urine. |
|
•Unconscious or convulsions |
|
|
Evaluation of the febrile child: After
initial stabilization, patient’s evaluation and management should be
done as per the algorithm described in Fig. 1.
Immunocompromised Children
Immune-compromised children are at high risk of
serious infections, with grave prognosis. Thus, it becomes important to
identify this group in ED at triage itself and have an aggressive
approach. Children with neutropenia, with malignancy on chemotherapy,
those on long term oral steroids like nephrotic syndrome, with human
immunodeficiency virus (HIV infection), and with primary
immunodeficiency states are the children at high risk and need extensive
evaluation in febrile state [18]. Fever in a neutropenic patient is
always an emergency, regardless of triage status and should be
categorized as a life-threatening event (E).
Fever With Focus or Localization
When a child presents to ED with fever and a
localizing symptom/sign, specific management becomes easier. Some of the
common localizing signs are seizures, cough, ear discharge, loose
stools, dysuria and rashes. History and evaluation in the ED to
determine the focus should be done after triage and initial
stabilization. Management depends upon the common organisms that prevail
in that particular age group. Many of these infections have viral
etiologies, which need only supportive treatment and a follow up.
Emerging antimicrobial resistance is a global health problem and
rational use of antibiotics in ED will go a long way in ameliorating
this issue.
Fever Without Localization
In a tropical country like India, it is not uncommon
to have febrile children without any localization, with epidemiological
evidence suggestive of a particular infectious etiology. These include
conditions like malaria, dengue, and enteric fever. Due to the
overlapping clinical presentation, it becomes difficult to pin point the
diagnosis in ED itself. Such children should be investigated for the
conditions with high index of suspicion and supportive therapy should be
provided.
 |
| |
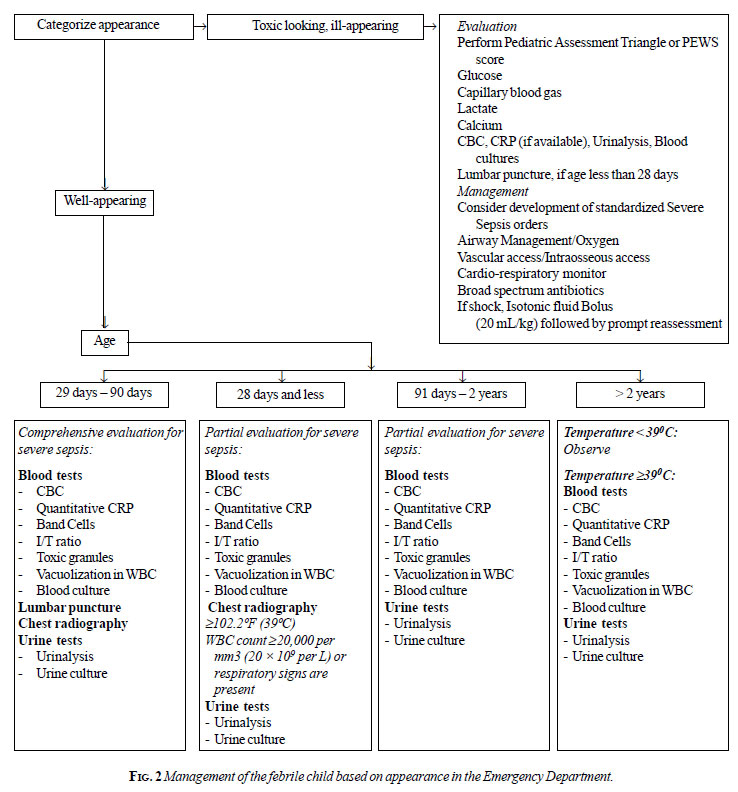
Fever without localization is a short duration
febrile illness of 5 to 7 days without an identifiable cause after
performance of history and examination [19-21]. ACEE recommends child to
be categorized into well- or ill-/toxic-appearing. Emergent
hospitalization and comprehensive evaluation is recommended in such a
child at any age (Fig. 2). Further, evaluation and
management of a well-looking child is based on the defined age groups
i.e., neonates (28 days and less), young infant (29-90 days); older
infant and young children (91 days – 2 years), and children more than 2
years (Fig. 2). There is no consensus among experts
regarding optimal cut-offs for evaluation of fever without focus. Most
have either used anecdotal or observational data as well as empiric data
to arrive at cut-offs. Furthermore, the physiologic rationale is often
missing. We chose the cut-offs as listed below:
28 days and less – most algorithms use this as a
cut-off and is a category of the febrile infants that probably has the
most consensus in the evaluation and management.
29-90 day cut-off – because this age group has
probably been the least studied as well has the most variation with
regards to a comprehensive evaluation, especially with relation to
performance of lumbar punctures. In addition, this is also the age
cut-off that is used in some febrile infant management algorithms.
91 days to 2 years – this is because most
febrile infants beyond 90 days will have a positive impact of
vaccinations as well as have a clinical examination that will allow the
clinician to selectively evaluate for fever instead of a comprehensive
evaluation that includes blood, urine and CSF studies. Specifically, the
consensus chose to limit the upper age to 2 years because UTI risk drops
substantially after the age of 2 years in female children.
These cut-offs are provided as a guide and also as a
basis to collect data in the Indian context. As more evidence is
generated, these may be modified further.
Evaluation
Evaluation should include a complete history and
physical examination. In a tropical country like India, dehydration
fever may be seen in newborns and young infants. Vaccination history
could avoid unnecessary investigation. Signs like irritability; poor
feeding, poor activity, and child not appearing well are subtle markers
for serious underlying illness [22]. Pulse rate and volume, pulse
oximetry, temperature, capillary refill time, respiratory rate (RR) and
type should be documented. A complete head to toe exam with all clothes
removed will help to find an occult cause of fever.
Newborns (< 28 days): All newborns
with fever should be admitted. A complete investigative workup which
includes complete blood count (CBC), C- reactive protein (CRP),
peripheral blood smear (PBS) (band form, toxic granules, vacuolization,
immature/total ratio ), blood and urine culture, urine analysis (UA),
lumbar puncture (LP), and chest X- ray (CXR) is mandatory. Stool
should be examined for pus cell and red blood cell (RBC) only if change
in frequency of stool is present. First negative septic screen in an
active febrile newborn is not the indication for discharge.
Young infants (29 to 90 days): Active
young infant between 29-90 days of age with fever should be observed in
the ED with vital sign measurement. Complete blood count (CBC),
peripheral blood smear (PBS), urine analysis (UA), and blood and urine
culture is necessary. Chest radiography is indicated if temperature
³102.2ºF
(39°C), leucocyte count ³20,000
per mm3 or respiratory signs
are present [23]. Urine tests recommended are microscopy and culture
from urine obtained by catheterization.
91 days to 2 years: In some instances, lumbar
puncture may be deferred in this age group. Investigative workup which
include complete blood count (CBC), C-reactive protein (CRP), peripheral
blood smear (PBS) (band form, toxic granules, vacuolization,
immature/total ratio), blood and urine culture, and urinanalysis.
Children above 2 years: If temperature <39ºC,
only obser-vation is recommended. If temperature is 39ºC or more,
investigative workup, which includes CBC, CRP, PBS (band form, toxic
granules, vacuolization, immature / total ratio), blood and urine
culture, Urinanalysis needs to be done [23]. PBS and rapid tests for
malaria, dengue and enteric may be done in endemic areas. Blood culture
may be taken in typhoid-endemic areas.
Sepsis screen parameters and serious bacterial
infection
Various sepsis screen parameters have been used with
different permutations and combinations to rule in and rule out SBI.
Markic, et al. [24] observed CBC, PCT, CRP and lab score
³3 as useful markers
for serious bacterial infections. Sensitivity and specificity was better
in age group of £90
days when compared with age group of
£180 days. In another
large study, both CRP (area under the receiver operating curve - ROC
0.77, 95% CI 0.69-0.85) and PCT (ROC area 0.75, CI 0.67-0.83) were found
to be strong predictors of serious bacterial infection[24]. Absolute
band cells and PCT were reported as the best markers of SBI in children
less than 36 months of age in another study, with PCT having the largest
ROC (0.80, 95% CI 0.71-0.89) [25, 26]. The high cost and limited
availability of PCT preclude its use as a screening tool in Indian EDs.
Management
In ill-appearing neonates and young infants,
intravenous (IV) access should be established and empiric antibiotics
should be started in the ED. Up to 28 days of age, ampicillin 100 to 200
mg/kg/day divided 8 hourly and gentamicin 7.5 mg/kg/day divided 8 hourly
should be started, whereas in older infants, intravenous Ceftriaxone 100
mg/kg/day or 75 mg/kg/day divided 12 hourly is given, depending on
presence or absence of meningeal involvement.
|
BOX 2 Indications for Hospitalization and
Discharge from Emergency Department
Indications for
Hospitalization
• All emergency patients in
need for airway stabilization, ventilation or continued O2
requirement
• Age <28 days
• Prolonged seizure/status
epilepticus
• Altered sensorium
• Electrolyte imbalance
• Signs of Severe Dehydration
• Not feeding well
• Respiratory distress
• SPO2 <90% in room air
• Drug toxicity or drug
reaction
• Unknown or undetermined
cause
• Concern for non-compliance
or inability to follow-up
Indications for Discharge
• No emergent need for
airway, ventilation or circulatory support
• Vitals stable
• Child accepting
• Definitive management plan
has been worked out
• Compliance ensured
• Follow up ensured
|
Patient disposition from the ED: After
initial stabilization and management in the ED, the patient may either
be hospitalized or be discharged home. Box 2 gives
indications for hospitalization and discharge of a febrile child from
ED. Patiet’s stable condition, definite follow up plan and compliance
become important while discharging the patient home. Table II
provides broad guidelines for admission in pediatric floor or intensive
care unit (ICU).
TABLE II Patient Disposition Guidelines
|
Disposition |
Action |
|
Observation in ED |
Reassess patient frequently, review and document vital signs
hourly |
|
Discharging home |
Provide appropriate counseling and a follow-up plan. Elicit
understanding of care plan by caretakers |
|
Admission/Transfer to Pediatric Floor |
Hemodynamically and respiratory stable patient, needs ongoing
treatment, monitoring and workup; |
|
Transfer to ICU |
Patient remains in critical condition, warrants ongoing
cardiorespiratory support to sustain life |
|
ED: Emergency department; ICU: Intensive care unit. |
Some patients may need transfer to another health
facility, due to non-availability of appropriate resources or services.
Box 3 summarizes the guidelines for referral that should
be stringently followed.
|
BOX 3 Guiedelines for Transfer* to
Another Health Facility
• Transfer, only when it is
stable to transfer.
• Appropriate stabilization
before transportation:
• Secure airway
• Intravenous or intraosseous
access
• Place on cardiac monitor
• Discuss transfer options
with the patients’ primary caregiver if available. Transfer is
dependent upon patient’s current status, the clinical concerns
of the provider, the best place for receiving adequate care, and
if caregiver/family is willing to transfer.
• Directly communicate with
receiving hospital regarding that transfer is required.
• Transport with person(s),
capable of managing any emergency en-route.
*due to non-availability of appropriate
resources or services
|
Summary
The outlined algorithmic approach on management of
fever in the ED is the first step of its kind initiated by the PEM
Chapter of ACEE-India under the aegis of INDO-US Emergency and Trauma
Collaborative. This approach is based on the current literature search
and available evidence pertaining to Indian context, aiming to
familiarize the emergency physicians to a stepwise approach for
evaluation and management of fever. This approach also includes focused
triage and patient disposition guidelines. Further steps are intended
to:
• obtain input from experts in pediatrics, EM,
PEM, infectious diseases, epidemiologists to modify the algorithm
• create a robust database to collect
retrospective and prospective data to elucidate the epidemiology of
the febrile child across various settings.
• modify the algorithm based on epidemiological
evidence.
• implement the algorithm and monitor compliance
as well as measure impact on practice pattern variation, clinical
outcomes and resource burden.
This algorithmic approach will require ongoing,
periodic revision(s) as new research emerges and is established in the
field.
Acknowledgenent: Elizabeth Duffy, MA, Department
of Emergency Medicine, University of Michigan (Ann Arbor, MI, USA) for
helping in critical editing, reviewing and formatting of the manuscript.
Contributors: PM: Guarantor of the paper with
responsibility for the integrity of the work as a whole; Substantial
contributions to the conception and design of the work, and drafted and
critically revised for important intellectual content; PB, RP, BF, BS,
SG: substantial contributions to the conception and design of the work,
and drafted and critically revised for important intellectual content;
Neha T, NR, Nitin T, AS, DS: substantial contributions to the
conception, and provided critical revisions; ML,RAO: Substantial
contributions to the design of the work, and critically revised content;
SG: Substantial contributions to the conception and design of the work;
and drafted and critically revised for important intellectual content.
All authors approved the final version to be published, and are
accountable for all aspects of the work to ensure that questions related
to the accuracy or integrity of any part of the work are appropriately
investigated and resolved.
Funding: None. Competing Interests: None
stated.
ANNEXURE I
Participants of the Consensus Meetings
I Consensus Meeting
Chairperson: Prashant Mahajan, (Michigan, USA);
Experts: Binita Shah (Brooklyn, NY, USA), Bernhard Fassl (UT,
USA), Prerna Batra, (Delhi, India), Abhijeet Saha (New Delhi, India),
Dheeraj Shah (Delhi, India), Indumathy Santhanam (Chennai, India), AP
Dubey (New Delhi, India), Devendra Mishra (New Delhi, India), Santosh
Soans (Bangalore, India), Reena Patel (UT, USA), Narendra Rai (Lucknow,
India), Neha Thakur (Lucknow, India), Nitin Trivedi (Jaipur, India).
II Consensus Meeting
Chairperson: Binita Shah (Brooklyn, NY, USA); Participants:
Prerna Batra (Delhi, India), Abhijeet Saha (Delhi, India), Reena Patel
(Salt Lake City, UT, USA), Neha Thakur (Lucknow, India), Nitin Trivedi (Jaipur,
India), and Narendra Rai (Lucknow, India).
References
1. Balmuth F, Henretig FM, Alpern ER. Fever. In:
RG Bachur& KN Shaw (eds.) Fleisher & Ludwig’s Textbook of Pediatric
Emergency Medicine, 7th edition. Lippincott Williams and Wilkins.
Philadelphia, PA, USA.2016. p. 176-85.
2. ACEP Clinical Policies Committee and Clinical
Policies Subcommittee on Pediatric Fever. Clinical Policy for Children
Younger than Three Years Presenting to the Emergency Department with
Fever. Ann Emerg Med. 2003;42:530-45.
3. Seow VK, Lin AC, Lin IY, Chen CC, Chen KC, Wang
TL, et al. Comparing different patterns for managing febrile
children in the ED between emergency and pediatric physicians: impact on
patient outcome. Am J Emerg Med. 2007;25:1004-8.
4. Phillips B, Selwood K, Lane SM, Skinner R, Gibson
F, Chisholm JC; United Kingdom Children’s Cancer Study Group. Variation
in policies for the management of febrile neutropenia in United Kingdom
Children’s Cancer Study Group centres. Arch Dis Child.2007;92:495-8.
5. Aronson PL, Thurm C, Williams DJ, Nigrovic LE,
Alpern ER, Tieder JS, et al.; Febrile Young Infant Research
Collaborative. Association of clinical practice guidelines with
emergency department management of febrile infants
£56 days of age. J
Hosp Med. 2015;10:358-65.
6. Harper MB. Update on the management of the febrile
infant. Clin Pediatr Emerg Med. 2004;5:5-12.
7. Abrahamsen SK, Haugen CN, Rupali P, Mathai D,
Langeland N, Eide GE, et al. Fever in the tropics: Aetiology and
case-fatality-A prospective observational study in a tertiary care
hospital in South India. BMC Infect Dis. 2013;13:355.
8. Singhi S, Rungta N. Tropical fever: Management
Guidelines. Ind J Crit Care Medicine. 2014;18:62-9.
9. Jatana SK. Pediatric emergencies in office
practice—an overview. Med J Armed Forces India. 2012; 68:4-5.
10. Mahajan P, Batra P, Shah B, Saha A, Galwankar S,
Aggrawal P, et al. The 2015 Academic College of Emergency Experts
in India’s INDO-US Joint Working Group white paper on establishing an
academic department and training pediatric emergency medicine
specialists in India. Indian Pediatr. 2015;52:1061-71.
11. Niven DJ, Gaudet JE, Laupland KB, Mrklas KJ,
Roberts DJ, Stelfox HT. Accuracy of peripheral thermometers for
estimating temperature: a systematic review and meta-analysis. Ann
Intern Med. 2015;163:768-77.
12. Brown PJ, Christmas BF, Ford RP. Taking an
infant’s temperature: Axillary or rectal thermometer? N Z Med
J. 1992;105:309-11.
13. Batra P, Goyal S. Comparison of rectal, axillary,
tympanic, and temporal artery thermometry in the pediatric emergency
room. Pediatr Emerg Care. 2013;29:63-6.
14. Batra P, Saha A, Faridi MM. Thermometry in
children. J Emerg Trauma Shock. 2012;5:246-9.
15. Pocketbook of Hospital Care for Children:
Guidelines for the Management of Common Childhood Illnesses – Second
Edition. WHO 2013. Available from: http://apps.who.int/iris/bitstream/10665/81170/1/9789241548373_eng.pdf.
Accessed August 25, 2016.
16. WHO Emergency Triage and Treatment (ETAT). Manual
for Participants. WHO Press. Geneva, Switzerland. 2005. Available from:
http://apps.who.int/iris/bitstream/10665/43386/1/9241546875_eng.pdf.
Accessed August 25, 2016.
17. Seiger N1, Maconochie I, Oostenbrink R, Moll
HA.Validity of different pediatric early warning scores in the emergency
department. Pediatrics. 2013;132:e841-50.
18. Holtzclaw B J. Managing fever and febrile
symptoms in HIV: Evidence-based approaches. J Assoc Nurses AIDS Care.
2013;24: S86-102.
19. Jhaveri R, Byington CL, Klein JO, Shapiro ED.
Management of the nontoxic-appearing acutely febrile child: a 21st
century approach. J Pediatr. 2011;159:181-5.
20. Brown L, Shaw T, Moynihan JA, Denmark TK, Mody A,
Wittlake WA. Investigation of afebrile neonates with a history of fever.
Canad J Emerg Med. 2004;6:343-8.
21. Ishimine P. Fever without source in children 0 to
36 months of age. Pediatr Clin North Am. 2006;53:167-94.
22. Care Process Model. Emergency Management of the
well-appearing febrile infant age 1-90 days. Intermountain Health Care.
May 2013. Available from: https://intermountain
healthcare.org/ext/Dcmnt%3Fncid%3D520441555. Accessed August 25,
2016.
23. Bressan S, Andreola B, Cattelan F, Zangardi T,
Perilongo G, Da Dalt L. Predicting severe bacterial infections in
well-appearing febrile neonates: laboratory markers accuracy and
duration of fever. Pediatr Infect Dis J. 2010;29:227-32.
24. Markic J, Kovacevic T, Krzelj V, Bosnjak N,
Sapunar A. Lab-score is a valuable predictor of serious bacterial
infection in infants admitted to hospital.Wien Klin Wochenschr.
2015;127:942-7.
25. Nijman RG, Moll HA, Smit FJ, Gervaix A, Weerkamp
F, Vergouwe Y, et al. C-reactive protein, procalcitonin and the
lab-score for detecting serious bacterial infections in febrile children
at the emergency department: a prospective observational study. Pediatr
Infect Dis J. 2014;33:e273-9.
26. Mahajan P, Grzybowski M, Chen X, Kannikeswaran N,
Stanley R, Singal B, et al. Procalcitonin as a marker of serious
bacterial infections in febrile children younger than 3 years old. Acad
Emerg Med. 2014;21:171-9.
|
|
|
 |
|

