|
|
|
Indian Pediatr 2016;53: 730-731 |
 |
Hansenís Chronic
Polyarthritis in a Child
|
|
Ananya Das, Rakesh Mondal,
#Kaushani Chatterjee and Dona
Banerjee
From Departments of Pediatric Medicine, Medical
College and #BC Roy PGIPS, Kolkata, West Bengal, India.
Correspondence to: Dr Rakesh Mondal, Professor and
Pediatric Rheumatologist, Department of Pediatrics, Medical College, 88
College Street, Kolkata 700 073, India.
Email:
[email protected]
Received: November 03, 2015;
Initial review: January 15, 2016;
Accepted: March 10, 2016.
Published online: June 01, 2016. PII:S097475591600003
|
Background: Musculoskeletal manifestations of leprosy are often
underdiagnosed and under-reported. Case characteristics: An
11-year old girl with leprosy presented with deforming symmetric
polyarthritis with raised inflammatory parameters and erosion on
imaging. Observation: The patient was diagnosed to have Hansenís
chronic polyarthritis and treatment started with non-steroidal
anti-inflammatory drugs and methotrexate. Message: Hansenís
chronic polyarthritis is a rare differential of juvenile chronic
arthritis in children.
Keywords: Arthritis, Complication, Leprosy.
|
|
L
eprosy (Hansenís disease) is a major public
health problems in India. It usually presents with skin lesions.
Musculoskeletal complaints are uncommon manifestations of leprosy in the
pediatric age group [1]. Among the different types of arthritis present
in leprosy, Hansenís chronic polyarthritis is the rarest variant. We
here present a case of chronic symmetrical polyarthritis which was
initially diagnosed as Erythema nodosum leprosum (ENL) and later
confirmed as Hansenís chronic polyarthritis.
Case Report
An 11-year-old girl, a diagnosed case of borderline
lepromatous leprosy (BL) on six months of multi-drug therapy (MDT), was
referred to our institution with tender erythematous nodules over the
lateral aspect of legs, shin and back, burning sensation in hands and
legs and constitutional symptoms for the last two weeks. Ulnar claw
hands were present (Fig.1). Bilateral ulnar and common
peroneal nerves were thickened. Xerosis, thickening and
hyperpigmentation of skin of the face, hands and legs were noted. There
was no urinary complaint, photosensitivity, skin rash or oral ulcer.
Organomegaly and lymphadenopathy were absent. However, the patient had
symmetrical polyarthritis involving small joints of hand, wrist, knee
and ankle for the last eight months for which she was taking
non-steroidal anti-inflammatory drugs (NSAIDs).
 |
|
Fig.1 Swelling of small joints of
hand with ulnar clawing.
|
Investigations revealed raised inflammatory
parameters (erythrocyte sedimentation rate 62 mm/h, C-reactive protein
10.8 mg/dL; normal <0.6 mg/dL). Complete haemogram showed anemia,
neutrophillic leucocytosis and thrombocytosis. Chest X-ray, liver
function test, renal function tests and urinalysis were within normal
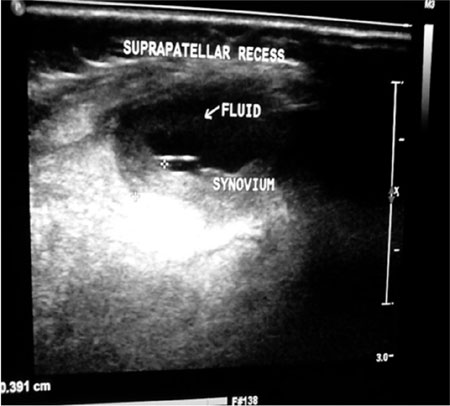
limits. Mantoux test was non-reactive. Juxta-articular erosion was
present in X-ray of wrists. Ultrasonography of knee joint showed
mild effusion with marginal erosion (Fig. 2). Serology for
hepatitis B, hepatitis C, human immunodeficiency virus (HIV) and Epstein
Barr virus (EBV) were non-reactive. Serological markers for other
connective tissue diseases such as Rheumatoid factor (RA), antinuclear
antibody (ANA), anti ds-DNA, anti-neutrophil cytoplasmic antibody
(ANCA), anti-cyclic citrullinated peptide (anti-CCP) and direct coombs
test (DCT) were negative. C3 level was 43 U/L. Nerve conduction velocity
(NCV) study showed axonal type of sensory-motor polyneuropathy in all
four limbs. A feature of panniculitis was found in skin biopsy specimen
suggestive of ENL.
 |
|
Fig.2 Ultrasound image showing
effusion and erosion of knee joint.
|
In view of skin lesions and raised inflammatory
parameters, ENL reaction was diagnosed, prednisolone started and MDT
continued. Skin lesions resolved over next four weeks. However, the
articular complaints persisted and fixed deformities noted.
Polyarthritis in this child was established as Hansenís chronic
polyarthritis. Methotrexate along with NSAID was added. The child showed
gradual improvement on follow-up over the next four months.
Discussion
Chronic polyarthritis in the index case, a feature of
leprous rheumatism was not due to lepra reaction, as deforming arthritis
of prolonged duration preceded the initiation of MDT and was steroid
non-responsive. Chronic arthritis in Charcotís joint is characterised by
dislocations, destruction of articular cartilage with debilitating
deformities, which was not the scenario in index case. Chronic arthritis
in this case cannot even be explained by co-occurrence of juvenile
idiopathic arthritis (JIA) or any other connective tissue diseases in
absence of characteristics symptomatology and related sero-markers.
Hence, our case was confirmed to be that of Hansenís chronic
polyarthritis.
Arthritis in leprosy is broadly divided into two
groups: acute arthritis and chronic arthritis. Acute arthritis seen as a
part of lepra reaction (ENL), is usually non-erosive, associated with
fever and worsening cutaneous lesions, which resolve over weeks without
deformities [2]. Hansenís chronic polyarthritis, first described by
Atkin, et al. [3] is a symmetric polyarthritis with predominantly
rheumatoid distribution. Postulated pathogenesis is direct synovial
infiltration by Mycobacterium leprae. This entity of chronic
arthritis is erosive, leading to deformities, and responds poorly to
anti-leprosy treatment. Aberrant immunological response in leprosy leads
to production of numerous autoantibodies like RA, ANA, and ANCA [4].
This may create diagnostic dilemma in patient of chronic polyarthritis
in leprosy patients, raising the possibility of co-occurrence of JIA.
However, anti-CCP is less likely to be found positive in leprosy
arthritis cases [5]. Haroon, et al. [6] described five cases of
Hansenís chronic polyarthritis out of 11740 leprosy patients in an adult
population [6]. Four of them were misdiagnosed as rheumatic disorders
initially [6].
Hansenís polyarthritis, though extremely rare, should
be kept in mind as a differential while managing a child with chronic
polyarthritis.
Contributors: AD: managed the case; RM: attending
physician; KC: wrote the manuscript; DB: help in reviewing the
manuscript. All authors approved the final manuscript.
Funding: None; Competing interest: None
stated.
References
1. Chopra A. Rheumatic and other musculoskeletal
manifestations and autoantibodies in childhood and adolescent leprosy:
Significance and relevance. J Pediatr. 2014;90:431-6.
2. Chauhan S, Wakhlu A, Agarwal V. Arthritis in
leprosy. Rheumatology. 2010;49:2237-42.
3. Atkin SL, Welbury RR, Stanfield E, Beavis D, Iwais
B, Dick WC. Clinical and laboratory studies of inflammatory
polyarthritis in patients with leprosy in Papua New Guinea. Ann Rheum
Dis. 1987;46:688-90.
4. Vengadakrishnan K, Saraswat PK, Mathur PC. A study
of rheumatological manifestations of leprosy. Indian J Dermatol Venereol
Leprol. 2004;70: 76-8.
5. Rath D, Bhargava S, Kundu BK. Leprosy mimicking
common rheumatologic entities: A trial for the clinician in the era of
biologics. Case Rep Rheumatol. Available from.
downloads.hindawi.com/journals/crirh/2014/429698.pdf. Accessed
January 26, 2016.
6. Haroon N, Agarwal V, Aggarwal A, Kumari N,
Krishnani N, Misra R. Arthritis as presenting manifestation of pure
neuritic leprosy Ė a rheumatologistís dilemma. Rheumatology.
2007;46:6536.
|
|
|
 |
|

