|
|
|
Indian Pediatr 2015;52: 704 -706 |
 |
Overcoming the ABO Incompatibility Barrier in
Pediatric Renal Transplantation
|
|
Sidharth Kumar Sethi, *Pranaw Jha, *Shyam Bihari
Bansal and Vijay Kher
From Kidney and Urology Institute; and *Renal
Transplant Institute; Medanta,
The Medicity Hospital, Gurgaon, Haryana, India.
Correspondence to: Dr Sidharth Kumar Sethi, Pediatric
Nephrology, Kidney and Urology Institute,
Medanta, The Medicity Hospital, Gurgaon, Haryana 122 001, India.
Email: sidsdoc@gmail.com
Received: December 18, 2014;
Initial review: January 27, 2015;
Accepted: May 28, 2015.
|
|
Background: ABO blood type incompatibility between a donor and
recipient is generally considered a contraindication to kidney
transplantation. Case characteristics: A 12-year-old boy
presented with end stage renal disease (blood group B), with the only
healthy available donor being mother (blood group AB). The child
received renal transplant with mother as the donor, with a designed
desensitization and immunosuppressive protocol. Observation: At 6
months, child is doing well, with stable graft function. Message:
ABO-incompatible kidney transplantation is a valid alternative for
children with end stage renal disease. This is the first report from
India of a Pediatric ABO incompatible renal transplant.
Keywords: Blood group, Kidney, Renal
transplantation.
|
|
Kidney transplantation is considered an optimal
therapy for all children with end stage renal disease; there is better
longevity, quality of life and cost-effectiveness in comparison to
long-term maintainence dialysis. Due to a severe shortage of suitable
cadaveric donors, most pediatric patients receive a kidney from their
living relatives. If an appropriate living related donor is not
available, a child may have to wait for a considerable period of time
for a cadaveric donor. In such circumstances, blood group ABO
incompatibility was regarded as a major obstacle in screening potential
living donors. ABO blood type incompatibility between a donor and
recipient is generally considered to be a contra-indication to kidney
transplantation because of the risk of preformed antibody-mediated
hyperacute rejection [1]. With significant advances in technology and
improved understanding of the nature of the ABO antigens and their
distribution, several series of successful adult and pediatric
ABO-incompatible transplant have been reported [1-4]. We report a case
of 12-year-old boy, who received a successful ABO incompatible renal
transplant from his mother.
Case Report
A 12-year-old boy presented to our hospital with
Stage 5 chronic kidney disease (CKD) and severe hypertension due to
reflux nephropathy. He was started on maintenance hemodialysis and
supportive care. The options of renal transplantation were discussed.
The blood group of the patient was B+, and no family member had the
compatible blood group, despite an extensive search for 6 months. The
patient’s mother had blood group AB+.
His current weight was 36 kg, height 140 cm, and body
surface area 1.18 m 2. His
baseline viral serology status was cytom egalovirus (CMV) (IgG Mother +,
Child +) and Epstein-Barr Virus (EBV) (Mother +, Child –).
After discussing the risk and benefits of ABO
incompatible transplant, the mother was selected as the donor. A flow-cytometry
cross-match was negative. His baseline anti-A antibody titer was 1:16.
He received injection Rituximab (170mg/m 2)
two weeks prior to transplant, and regular immunosuppression (Tacrolimus
0.05mg/kg and Mycophenolate 600mg/m2/dose)
was started a week prior to tentative date of transplant. He was planned
for double filtration plasmapheresis (one plasma volume) two days before
surgery. The first session of double filtration plasma-pheresis was
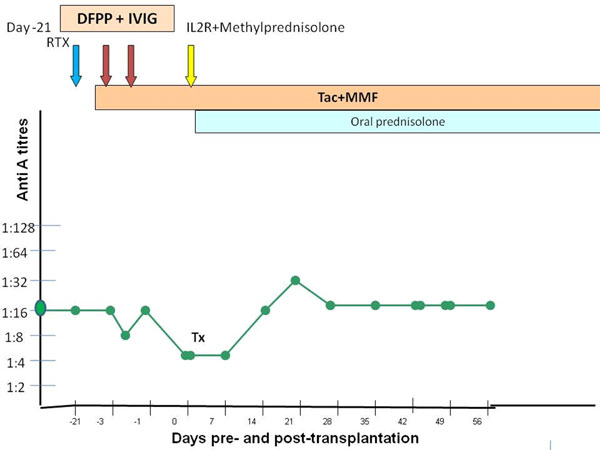
followed by intravenous immunoglobulin (IVIG) 5 g (0.2 g/kg/dose) (Fig.
1). He received another session of plasmapheresis in view of rebound
rise in anti-A titer. He required two units of fresh frozen plasma in
view of deranged prothrombin time after the second plasmapheresis.
 |
|
Fig. 1 The trend of antibodies with
immunosuppresion in the present case. DFPP double
filtration plasmapheresis; IVIG: Intravenous immunoglobulin; Tac:
Tacrolimus; MMF: Mycophenolate mofetil: TX: Date of transplant;
RTX: Rituximab; IL2R: Interleukin-2 receptor antagonist
Basiliximab. (See color image at website).
|
The dose of tacrolimus (0.1 mg/kg daily) was
increased from a day before surgery. He was transplanted in October
2014, with pre-operative anti-A titers of 1:4. He was given induction
with intravenous basiliximab 10 mg on days 0 and 4 and intravenous
methylprednisolone 400 mg on day 0 followed by oral prednisolone 40 mg
that was tapered to 20 mg daily. Target blood levels of tacrolimus in
initial three months were 9-12 ng/mL, 4-6 months 6-8 ng/mL and 4-6 ng/mL
thereafter. He is currently on twice daily dosing of Tacrolimus to
maintain the required levels, and is on tapering prednisolone and
mycophenolate mofetil.
Post-operatively, anti-A titers were monitored daily
for a week, twice weekly for 4 weeks, and then weekly for 4 weeks, and
then done only if there was a renal dysfunction. Initially, his anti-A
titers rose to 1:32 on 15th
postoperative day but then declined to 1:16 thereafter.
Post-operatively, he had a progressive decline in serum creatinine to
0.5 mg/dL. There was no episode of graft dysfunction/rejection. The
child has now completed 6 months of valganciclovir and trimethoprim
prophylaxis. Currently, he is 6-months post-transplant with a stable
graft function, serum creatinine 0.6 mg/dL with a normal urine
microscopy and no proteinuria (urine protein/creatinine ratio 0.08), and
negative for opportunistic infections.
Discussion
Until recently up to one-third of potential kidney
donors had to be excluded from living donation due to ABO
incompatibility or had to undergo aggressive pre-conditioning protocols
to overcome the immunological barrier and to enlarge the pool of
potential living donation [2,3]. After introduction of rituximab,
immunoabsorptive columns, and better understanding of biology in renal
transplantation, ABO incompatible transplantation seems a feasible
option, without the need for splenectomy, and with lower dosing of
rituximab [3-5].
Our center earlier reported an 18-yr-old adolescent
with ABO incompatible transplant [6]. Our departmental threshold of
anti-blood group antibody is 1:8, and the child achieved 1:4 anti-A
pre-transplant titers (post plasma exchange), which is considered safe
to transplant. There is no clear consensus on pre-transplant titer.
Although some use the goal of a titer of 8 or less before surgery, there
are centers that use higher-titer goals, and report excellent results.
Several investigators have demonstrated that lowering
the titer of the offending anti-ABO antibodies pretransplantation, and
maintaining such lowered levels for several weeks post engraftment,
allows allograft survival even when antibodies later return to
predepletion levels, and despite the presence of normal levels of
complement. The apparent resistance of a vascularized graft to humoral
rejection despite the presence of antibodies directed against the donor
endothelium is called accommodation. There are several mechanisms
involved in accommodation such as disruption of normal signal
transduction, reduced cellular adhesion and prevention of apoptosis [7].
It has also been proposed that this may happen due to inactivation of
glycosyltransferase enzyme during ischemia reperfusion injury. Hence,
fewer blood group antigens are expressed on donor endothelium thereby
reducing the immunogenicity [8]. Acute antibody-mediated rejection in an
ABO incompatible renal transplant, almost always occur in first two
weeks of renal transplant, which is the time taken for accommodation to
set in [7-9]. Hence, most important requisite for successful ABO
incompatible renal transplant is to achieve low antibody titer at the
time of transplant and in two weeks post-transplant [9,10]. Therefore,
the management of the child and the complications (including infections
and acute rejection) does not differ from a normal transplant, as the
body has accommodated the incompatibility.
There are reports of comparable results of ABO
incompatible and ABO compatible renal transplantation in adults and
children [1-4]. This report is to emphasize to pediatricians that ABO
incompability does not always mean loss of hope for children with end
stage renal disease.
References
1. Shishido S, Hasegawa A. Current status of
ABO-incompatible kidney transplantation in children. Pediatr Transplant.
2005;9:148-54.
2. Shishido S, Hyodo YY, Aoki Y, Takasu J, Kawamura
T, Sakai KK, et al. Outcomes of pediatric ABO-incompatible kidney
transplantations are equivalent to ABO-compatible controls. Transplant
Proc. 2012;44: 214-6.
3. Ohta T, Kawaguchi H, Hattori M, Takahashi K,
Nagafuchi H, Akioka Y, et al. ABO-incompatible pediatric kidney
transplantation in a single-center trial. Pediatr Nephrol. 2000;14:1-5.
4. Schaefer B, Tönshoff B, Schmidt J, Golriz M,
Mehrabi A, Gombos P, et al. Bleeding complications in pediatric
ABO-incompatible kidney transplantation. Pediatr Nephrol.
2013;28:327-32.
5. Takahashi K, Saito K, Takahara S, Okuyama A,
Tanabe K, Toma H, et al. Japanese ABO Incompatible Kidney
Transplantation Committee. Excellent long-term outcome of
ABO-incompatible living donor kidney transplantation in Japan. Am J
Transplant. 2004;4:1089-96.
6. Gupta PN, Pokhariyal S, Bansal S, Jain S, Saxena
V, Sharma R, et al. Renal transplantation across ABO barrier.
Indian J Nephrol. 2013;23:214-6.
7. Park WD. Accommodation in ABO-incompatible kidney
allografts, a novel mechanism of self-protection against
antibody-mediated injury. Am J Transplant 2003;3:952-60.
8. Takahashi K. Accommodation in ABO-incompatible
kidney transplantation: why do kidney grafts survive?Transplant Proc.
2004;36:193S-6S.
9. Sassi M, Maggiore U, Buzio C, Franchini M.
Immunohaematological and apheretic aspects of the first kidney
transplant from a living, ABO-incompatible donor carried out in Italy.
Blood Transfus. 2011;9:218-24.
10. Allen G, Simpkins CE, Segev D, Warren D, King K,
Taube J, et al. Rapid accommodation of an A1 renal allograft
after preconditioning for ABO incompatible transplantation. Contrib
Nephrol. 2009;162:35-46.
|
|
|
 |
|

