|
|
|
Indian Pediatr 2015;52:
669-673 |
 |
Normative Blood Pressure Data for Indian
Neonates
|
|
Moumita Samanta, Rakesh Mondal, Somosri Ray, Tapas
Sabui, *Avijit Hazra, #Chanchal
Kundu, Debolina Sarkar and Dibyendu Roychowdhury
From Departments of Pediatric Medicine, Medical
College Kolkata; #Cardiology, *Pharmacology, IPGME&R and SSKM Hospital;
Kolkata, West Bengal, India.
Correspondence to: Dr Rakesh Mondal, Balarampur,
Mahestala, Kolkata 700141, West Bengal, India.
Email: ivanrakesh2001@gmail.com
Received: September 01, 2014;
Initial review: January 02, 2015;
Accepted: May 29, 2015.
|
Objective: To establish the normative blood pressure (BP) values in
healthy Indian neonates using oscillometric method, and to develop BP
percentile charts.
Design: Prospective observational study.
Setting: Neonatal unit of a teaching hospital in
Eastern India.
Participants: 1617 hemodynamically stable inborn
neonates without birth asphyxia, major congenital anomaly, maternal
complications (e.g. preeclampsia, hypertension, diabetes) or
critical neonatal illness.
Procedure: Quite state measurements of systolic
BP (SBP), diastolic BP (DBP) and mean arterial pressure (MAP) were
recorded by oscillometric method on day 4, 7 and 14 of postnatal life.
The averages of three readings at 2-minute intervals were used.
Results: Percentile charts (providing 5th, 10th,
25th, 50th, 75th, 95th, and 99th percentile values) have been developed.
SBP, DBP and MAP showed a steady rise from day 4 to day 14, and were
comparable between males and females, but were significantly lower in
preterms than in term neonates
Conclusions: Normative neonatal BP data along
with gestational age-wise percentile charts shall be of help for
decision-making and planning for sick newborns.
Keywords: Blood pressure, Hypertension, Neonate, Normogram.
|
|
N
eonatal hypotension and hypertension require
early detection and timely management due to possible association with
short and long term adverse outcomes [1]. Blood pressure (BP) increases
with birth weight, and gestational and chronological age [2]. However,
there is paucity of studies documenting normative blood pressure values
in healthy term and preterm neonates in India. Invasive BP monitoring,
even though more accurate; is associated with complications such as
infection, vasospasm and thrombus formation [3-5]. Indirect methods have
been shown to be reliable and consistent if conducted under standardized
conditions [6]. Studies evaluating normal BP ranges for normal, low
birth weight (LBW) and very low birth weight (VLBW) infants have
drawbacks of small sample size, retrospective data collection,
infrequent measurements, or inclusion of infants on inotropes or with
cerebral injury [1,7,8]. We planned this study to generate normative
BP readings of healthy Indian neonates.
Methods
This prospective observational study was conducted on
healthy term and preterm newborns delivered in a teaching hospital from
September 2013 to April 2014 in Kolkata, India. The study protocol was
approved by the Institutional Ethics Committee.
Enrolment was done on 3 days in a week (Monday,
Wednesday and Friday). All healthy newborns were enrolled after birth on
the scheduled days after obtaining written informed consent from the
parent. Exclusion criteria included birth asphyxia; infants of mothers
with hypertension, preeclampsia, gestational diabetes, type 1 diabetes
mellitus or illicit substance use; major congenital anomaly; and sepsis
or other problems requiring admission to neonatal intensive care unit
(NICU), except for those preterm neonates admitted only for
establishment of feeding. Each neonate was studied on day 4, 7, and 14
of birth. If discharged prior to day 14, the mother was asked to come
for follow-up on the scheduled day.
Multichannel monitor (Larson and Turbo make; Star 55)
was used to determine systolic BP (SBP), diastolic BP (DBP), and mean
arterial pressure (MAP) by oscillometric method. Disposable infant BP
cuffs (sizes 6-11 cm, 4-6 cm and 1-4 cm) were used. The smallest cuff
size that covered at least two- thirds of the right upper arm length and
encompassed the entire arm circumference was selected. One investigator
performed all BP measurements using a standardized protocol [9]. The
appropriate-sized cuff was applied to the right upper arm with baby in
prone position. Three successive BP recordings were taken at 2-minute
intervals. The average of these three readings, rounded off to the
nearest mmHg, was calculated and recorded for further analysis. The
tasks of feeding the babies, applying an appropriate BP cuff and keeping
them in prone position were done by the trained nursing staff. The
doctor was involved in checking the preparatory work and recording the
BP. Mean, standard deviation (SD),95% confidence interval (CI), and 5th,
10th, 25th, 50th, 75th, 95th and 99th percentile values were calculated
for the whole group. Statistica version 6 (Tulsa, Oklahoma: StatSoft
Inc., 2001) and MedCalc version 11.6 (Mariakerke, Belgium: MedCalc
Software 2011) softwares were used for statistical analysis.
Results
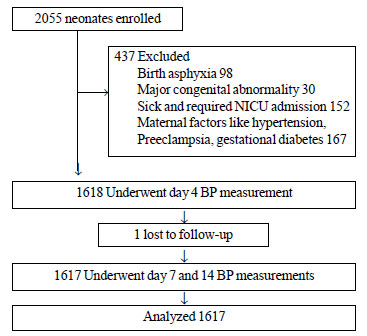
From the 2055 neonates screened, data of 1617 (916
males) were available for analysis. Fig. 1 shows the flow
chart for the study participants. Of the 1617 analyzed, 97 had some
missing data (86 babies present on day 7 but absent on day 14; 11 absent
on day 7 but present on day 14). There were 1427 term (1412 appropriate
for gestational age [AGA]) and 190 preterm (186 AGA) newborns. The of BP
recordings on days 4, 7 and 14 for term and preterm neonates have been
presented in Table I along with the percentile values on
the respective days. There were no statistically significant difference
in mean SBP, DBP and MAP recordings between males and females. However,
all three parameters were significantly lower in preterms compared to
term neonates on each of the three days.
TABLE I Oscillometric Neonatal Blood Pressure (mmHg) Stratified by Gestational Status (N=1617)
|
Parameter |
Status |
Mean (SD) |
5th |
10th |
25th |
50th |
75th |
90th |
95th |
99th |
|
Day 4-SBP |
Term |
74 (7) |
62 |
64 |
68 |
74 |
78 |
82 |
84 |
88 |
|
Preterm |
62 (7) |
46 |
54 |
58 |
62 |
66 |
72 |
74 |
78 |
|
DBP |
Term |
54 (7) |
42 |
43 |
50 |
54 |
60 |
62 |
62 |
66 |
|
Preterm |
43 (6) |
32 |
34 |
40 |
42 |
47 |
50 |
52 |
56 |
|
MAP |
Term |
61 (6) |
48 |
50 |
56 |
60 |
66 |
68 |
70 |
73 |
|
Preterm |
49 (6) |
38 |
41 |
46 |
48 |
53 |
56 |
58 |
62 |
|
Day 7-SBP |
Term |
78 (6) |
66 |
70 |
74 |
78 |
82 |
84 |
87 |
90 |
|
Preterm |
66 (7) |
54 |
58 |
62 |
66 |
70 |
74 |
77 |
82 |
|
DBP |
Term |
58 (6) |
50 |
50 |
55 |
60 |
62 |
64 |
66 |
72 |
|
Preterm |
47 (6) |
38 |
40 |
42 |
48 |
50 |
55 |
56 |
62 |
|
MAP |
Term |
64 (5) |
54 |
56 |
61 |
66 |
68 |
70 |
72 |
75 |
|
Preterm |
53 (5) |
44 |
46 |
50 |
54 |
57 |
60 |
63 |
66 |
|
Day 14-SBP |
Term |
81 (5) |
72 |
74 |
78 |
82 |
84 |
88 |
90 |
90 |
|
Preterm |
70 (7) |
60 |
61 |
66 |
70 |
75 |
78 |
80 |
85 |
|
DBP |
Term |
61 (6) |
52 |
54 |
60 |
60 |
64 |
68 |
70 |
74 |
|
Preterm |
51 (6) |
40 |
42 |
50 |
50 |
55 |
60 |
60 |
62 |
|
MAP |
Term |
68 (5) |
58 |
61 |
66 |
68 |
71 |
74 |
75 |
79 |
|
Preterm |
58 (6) |
47 |
49 |
56 |
57 |
61 |
66 |
66 |
68 |
|
SBP = Systolic blood pressure; DBP = Diastolic blood
pressure; MAP = Mean arterial pressure. |
 |
|
Fig. 1 Flow chart for the study
participants.
|
Table II presents BP data for days 4, 7 and
14 by gestational age, from 32nd to 40th week.
TABLE II Oscillometric Neonatal Blood Pressure Recordings Stratified by Gestational Age (Weeks) at Birth
|
Week |
BP |
Day-4 |
Day-7 |
Day-14 |
|
Percentile |
SBP |
DBP |
MAP |
SBP |
DBP |
MAP |
SBP |
DBP |
MAP |
|
32 |
10 |
50 |
32 |
41 |
55 |
40 |
45 |
60 |
40 |
48 |
|
50 |
58 |
40 |
46 |
62 |
42 |
50 |
68 |
50 |
56 |
|
90 |
68 |
50 |
54 |
72 |
52 |
59 |
75 |
55 |
61 |
|
95 |
77 |
50 |
56 |
74 |
55 |
59 |
75 |
56 |
62 |
|
99 |
78 |
56 |
58 |
74 |
56 |
61 |
76 |
58 |
64 |
|
33 |
10 |
54 |
35 |
43 |
61 |
40 |
48 |
62 |
42 |
49 |
|
50 |
64 |
42 |
48 |
68 |
45 |
52 |
68 |
50 |
56 |
|
90 |
74 |
51 |
56 |
74 |
52 |
59 |
78 |
58 |
64 |
|
95 |
77 |
52 |
56 |
78 |
55 |
60 |
78 |
58 |
64 |
|
99 |
82 |
58 |
66 |
80 |
60 |
66 |
82 |
58 |
66 |
|
34 |
10 |
55 |
30 |
41 |
60 |
40 |
48 |
62 |
44 |
50 |
|
50 |
62 |
42 |
48 |
65 |
48 |
53 |
68 |
50 |
56 |
|
90 |
70 |
48 |
53 |
72 |
52 |
58 |
76 |
55 |
62 |
|
95 |
78 |
50 |
56 |
74 |
54 |
59 |
78 |
58 |
64 |
|
99 |
78 |
55 |
61 |
78 |
58 |
64 |
82 |
60 |
67 |
|
35 |
10 |
59 |
38 |
45 |
62 |
42 |
50 |
68 |
48 |
55 |
|
50 |
64 |
44 |
50 |
68 |
50 |
56 |
73 |
52 |
59 |
|
90 |
69 |
51 |
56 |
74 |
54 |
60 |
78 |
58 |
64 |
|
95 |
72 |
52 |
56 |
76 |
55 |
61 |
78 |
60 |
66 |
|
99 |
74 |
58 |
62 |
78 |
62 |
66 |
78 |
62 |
67 |
|
36 |
10 |
55 |
40 |
46 |
62 |
42 |
50 |
65 |
50 |
56 |
|
50 |
66 |
44 |
51 |
68 |
50 |
57 |
74 |
55 |
60 |
|
90 |
75 |
52 |
59 |
78 |
56 |
63 |
80 |
62 |
66 |
|
95 |
76 |
55 |
61 |
78 |
58 |
64 |
82 |
62 |
68 |
|
99 |
77 |
55 |
62 |
82 |
62 |
66 |
86 |
65 |
68 |
|
37 |
10 |
62 |
42 |
49 |
68 |
50 |
56 |
74 |
52 |
60 |
|
50 |
72 |
52 |
58 |
76 |
56 |
62 |
78 |
60 |
66 |
|
90 |
80 |
60 |
66 |
82 |
62 |
68 |
88 |
62 |
69 |
|
95 |
82 |
62 |
66 |
85 |
62 |
68 |
88 |
68 |
73 |
|
99 |
84 |
64 |
70 |
87 |
68 |
74 |
90 |
72 |
77 |
|
38 |
10 |
64 |
47 |
53 |
70 |
52 |
58 |
74 |
54 |
61 |
|
50 |
73 |
53 |
60 |
78 |
58 |
65 |
80 |
60 |
67 |
|
90 |
79 |
62 |
66 |
84 |
62 |
69 |
86 |
66 |
72 |
|
95 |
82 |
62 |
67 |
84 |
64 |
70 |
88 |
68 |
74 |
|
99 |
84 |
66 |
72 |
88 |
68 |
74 |
90 |
72 |
76 |
|
39 |
10 |
66 |
44 |
51 |
70 |
50 |
58 |
74 |
55 |
61 |
|
50 |
76 |
54 |
61 |
78 |
60 |
66 |
82 |
60 |
68 |
|
90 |
82 |
62 |
67 |
84 |
62 |
69 |
88 |
68 |
73 |
|
95 |
84 |
62 |
68 |
86 |
66 |
72 |
90 |
70 |
75 |
|
99 |
88 |
66 |
72 |
90 |
72 |
74 |
92 |
75 |
80 |
|
40 |
10 |
68 |
50 |
56 |
72 |
53 |
60 |
78 |
58 |
64 |
|
50 |
77 |
58 |
64 |
82 |
60 |
68 |
84 |
64 |
70 |
|
90 |
84 |
62 |
70 |
87 |
66 |
72 |
90 |
70 |
75 |
|
95 |
87 |
64 |
70 |
88 |
68 |
74 |
90 |
70 |
76 |
|
99 |
88 |
68 |
74 |
90 |
72 |
77 |
90 |
76 |
81 |
Discussion
These gestational age-wise percentile charts for
Indian newborns are likely to be of help in NICU settings for bedside
decision-making, and for management of sick neonates. The limitations of
the study include small sample size for preterm and SGA neonates. All
the recordings were done by a single observer. Although single observer
eliminates the possibility of interobserver variation, it increases the
chances of erroneous result if this observer keeps on making a
systematic error.
In our study, the median values of SBP, DBP and MAP
on day 4 of life were comparable to those found by Kent, et al.
[10] in Australian term newborns. The day-wise increment in MAP as seen
in our study was also reported by Cunningham, et al. [11]. Kent,
et al. [12] in 2009 reported normative BP data in 147
non-ventilated preterm neonates, and showed that the BP in preterm
neonates was comparable to that of term infants, after two weeks.
However, analysis of data from 566 preterm neonates in southern
Cleveland [13] showed that BP is preterms continues to rise after 10
days of life, and stabilizes by a postconceptional age of 44-48 weeks. A
higher value of DBP recorded in our study could be possibly due to the
influence of higher rates of vaginal delivery, intrauterine growth
retardation and maternal steroid injections, which were taken into
consideration [14-16]. Higher DBP at the end of 2nd week with drop in
DBP in the subsequent weeks has been reported earlier [17]. Follow-up
blood pressure data in these neonates was not collected.
We conclude that the data derived from this study can
be used to diagnose hypotension and hypertension in Indian newborns and
monitor blood pressure of sick neonates.
Contributors: MS, SR, RM, DS, TS, DRC:
diagnosis and management of the patients; RM, MS, CK, TS: searched
the literature; RM, MS, AH: drafted the manuscript; MS, CK, AH, RM:
critical review. All the authors approved the final version.
Funding: None; Competing interests: None
stated.
|
What is Already Known?
• Normal blood pressure data for neonates are
available from other countries.
What This Study Adds?
• Normative blood pressure data with
gestational age-wise percentile charts from Indian newborns is
provided.
|
References
1. Nuntnarumit P, Yang W, Bada-Ellzey HS. Blood
pressure measurements in the newborn. Clin Perinatol. 1999;26:981-96.
2. Gulati A, Srivastava RN. Hypertension. In:
Srivastava RN, Bagga A, editors. Pediatric Nephrology,5thed. New
Delhi: Jaypee Publishers. p. 337-59.
3. Langbaum M, Eyal FG. A practical and reliable
method of measuring blood pressure in the neonate by pulse oximetry. J
Pediatr. 1994;125:591-5.
4. Jones DW, Appel LJ, Sheps SG, Roccella EJ, Lenfant
C. Measuring blood pressure accurately: new and persistent challenges. J
Am Med Assoc. 2003; 289:1027-30.
5. Dasgupta SJ, Gill AB. Hypotension in the very low
birthweight infant: the old, the new, and the uncertain. Arch Dis Child
Fetal Neonatal Ed. 2003;88:F450-4.
6. National High Blood Pressure Education Program
Working Group on High Blood Pressure in Children and Adolescents. The
fourth report on the diagnosis, evaluation and treatment of high blood
pressure in children and adolescents. Pediatrics. 2004;114:555-76.
7. Watkins AM, West CR, Cooke RW. Blood pressure and
cerebral haemorrhage and ischaemia in very low birthweight infants.
Early Hum Dev. 1989;19:103-10.
8. Versmold HT, Kitterman JA, Phibbs RH, Gregory GA,
Tooley WH. Aortic blood pressure during the first 12 hours of life in
infants with birth weight 610 to 4,220 grams. Pediatrics.
1981;67:607-13.
9. Nwankwo MU, Lorenz JM, Gardiner JC. A standard
protocol for blood pressure measurement in the newborn. Pediatrics.
1997;99;e10
10. Kent AL, Kecskes Z, Shadbolt B, Falk MC.
Normative blood pressure data in the early neonatal period. Pediatr
Nephrol. 2007;22:1335-41.
11. Cunningham S, Symon AG, Elton RA, Zhu C, McIntosh
N. Intra-arterial blood pressure reference ranges, death and morbidity
in very low birth weight infants during the first seven days of life.
Early Hum Dev. 1999;56:151-65.
12. Kent AL, Meskell S, Falk MC, Shadbolt B.
Normative blood pressure data in non-ventilated premature neonates from
28-36 weeks gestation. Pediatr Nephrol. 2009;24:141-6.
13. Northern Neonatal Nursing Initiative. Systolic
blood pressure in babies of less than 32 weeks gestation in the first
year of life. Arch Dis Child Fetal Neonatal Ed. 1999;80:F38-42.
14. LeFlore JL, Engle WD. Clinical factors
influencing blood pressure in the neonate. NeoReviews. 2002;3:e145-50.
15. Holland WW, Young IM. Neonatal blood pressure in
relation to maturity, Mode of delivery, and condition at Birth.Br Med J.
1956;8:1331-3.
16. Zinner SH, Lee YH, Rosner B, Oh W, Kass EH.
Factors affecting blood pressures in newborn infants. Hypertension.
1980;2:I99-201.
17. Blood pressure disorders – neonates. Available
from:http://www.health.vic.gov.au/neonatalhandbook/procedures/blood-pressure.htm.
Accessed on January 10, 2015.
|
|
|
 |
|

