|
|
|
Indian Pediatr 2014;51:
664-665 |
 |
Successful Conversion of Post-Cardiac Surgery
Electric Storm in a Child
|
|
Abhinav Rastogi, Ajay Gupta and Vishal K Singh
From the Department of Pediatric Critical Care,
Fortis Escorts Heart Institute, New Delhi, India.
Correspondence to: Dr Abhinav Rastogi, Pediatric
Critical Care Department, Fortis Escorts Heart Institute, Okhla,
New Delhi 110 025, India.
Email:
[email protected]
Received: February 24, 2014;
Initial review: March 31, 2014;
Accepted: June 02, 2014.
|
|
Background: The management of
ventricular electrical storm can prove to be a challenge for the
clinician given its complexity and life threatening consequences.
Case characteristics: 8-year-old boy with repeated life-threatening
polymorphic ventricular tachycardia following aortic valve replacement
surgery. Intervention: Defibrillated 45 times in addition to
multiple antiarrhythmic drugs. Outcome: Conversion to stable
sinus rhythm with normal neurological outcome. Message: Electric
storm can be controlled by combination of multiple intravenous
antiarrhythmic drugs.
Keywords: Defibrillation, Electrical storm,
Ventricular tachycardia.
|
|
E
lectrical storm has been infrequently reported in
children, and variable management strategies have been described in
literature [1]. It is defined as occurrence of three or more distinct
episodes of ventricular tachycardia (VT) or ventricular fibrillation
(VF) within 24 hours, requiring defibrillation. Sustained VT that
resumes after one or more sinus cycle and within 5 minutes of
efficacious therapeutic intervention by the defibrillator is regarded as
severe form of electrical storm [2]. We report electric storm in a child
and made a good recovery.
Case Report
An 8-year-old-boy was admitted to our hospital with
complaints of progressive breathlessness and intermittent fever for last
one month. He previously underwent aortic valve replacement (21 mm St.
Jude prosthetic valve) for congenital aortic stenosis, almost a year
back. He was treated for suspected infective endocarditis (culture
negative) elsewhere. A 12-lead electrocardiogram (ECG) revealed sinus
tachycardia with normal QTc interval (0.42 sec), normal progression of R
waves and left bundle branch block pattern. A 2D echocardiography with
color doppler revealed severe left ventricular dysfunction (left
ventricular ejection fraction (LVEF) 25%) with stuck aortic valve (no
vegetations). He developed hemodynamically stable ventricular
tachy-cardia after admission and was started on intravenous amiodarone.
His initial blood cultures were negative and baseline sepsis screen was
negative. He underwent repeat aortic valve replacement (19 mm TTK Chitra
aortic mechanical tilting disc prosthesis). Intraoperative findings
revealed stuck aortic valve with vegetations; valve tissue was sent for
histological and microbiological study, which grew carbapenem resistant
Klebsiella pneumoniae.
Postoperative trans-esophageal echocardiography
revealed biventricular dysfunction (LVEF 10-15%), and no residual
gradient across aortic valve. He had sinus bradycardia with intermittent
atrioventricular (AV) disso-ciation with slow ventricular conduction;
amiodarone was tapered over 36 hours and he was maintained on overdrive
AV sequential pacing. The patient was in low cardiac output state with
fluctuating hemodynamics on moderate inotropic support. On 2nd
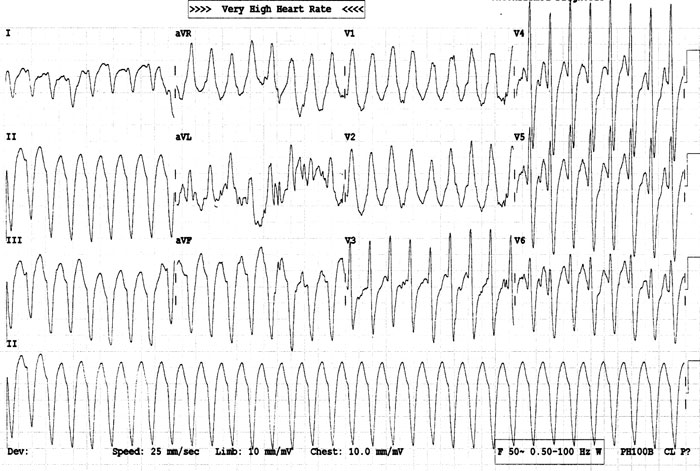
postoperative day, patient developed recurrent episodes of polymorphic
ventricular tachycardia with unstable hemodynamics on controlled
ventilation (Fig. 1). Arterial blood gas (ABG) analysis
revealed normal electrolytes and acid base physiology. In next 8 hours,
45 DC shocks (up to 8J/kg) were delivered due to recurrence of VTs after
transient reversion to sinus rhythm. He also received two boluses of
intravenous (IV) amiodarone (5 mg/kg) and repeated doses of IV lidocaine
(1 mg/kg) followed by their infusions. Since the patient was poorly
responsive, he was also started on IV esmolol infusion after bolus.
There was no significant change in QTc interval despite multiple doses
of amiodarone. Magnesium sulphate and glucose-insulin-potassium infusion
did not convert the arrhythmia. Finally, it was controlled with deep
sedation and paralysis with fentanyl, midazolam and vecuronium, with
infusions of lidocaine at 40 µg/kg/min, amiodarone at 20 µg/kg/min
and esmolol at 100 µg/kg/min.
 |
|
Fig. 1 ECG during the episode of
electric storm.
|
Post-event, he had LVEF of 10% with septal and apical
akinesis, borderline low blood pressure and high left atrial pressure.
Inotropic support was reoptimized with dobutamine and milrinone, and
ventilation was continued for next 72 hours.
His left ventricular function gradually improved and
he was extubated on 6th postoperative day with normal neurological
status. He was continued on oral amioda-rone, metoprolol and
acetyltolinesterase inhibitors. At follow-up 14 days later, he was in
sinus rhythm consistently.
Discussion
The mechanisms of electrical storm are quite complex
and not well understood. It has been postulated that cellular and
membrane alterations can increase intracellular calcium overload, with
altered action potential duration and morphology leading to its onset
[3,4]. The important role of increased sympathetic tone has been well
documented. Many conditions including ischemia, surgery [5] and
hyperthermia [6] can precipitate increased adrenergic output.
Specific antiarrhythmics indicated for electrical
storm include amiodarone, procainamide, lidocaine and bretylium. Current
Advanced Cardiac Life Support (ACLS) guidelines recommend amiodarone for
cardiac arrest in children associated with shock-refractory VT/VF.
Studies examining the effect of intravenous amiodarone in the management
of electrical storm have reported its efficacy [7].
Beta-antagonists – targeted to attenuate enhanced
sympathetic output – are also evolving as a promising modality [8]. In
our patient, we used esmolol (predominantly a β-1
antagonist), which can be used as an infusion and dose can be easily
titrated based on response. Left stellate ganglion blockade, though
effective, requires a high level of expertise, and may not be feasible.
Importance of deep sedation and even paralysis in this setting cannot be
overemphasized.
Given the unstable nature of the disease, electric
storm often requires combination therapy. Manolis, et al. [10]
reported a case using triple drug intervention with a beta antagonist,
class III antiarrhythmic, and a class IB antiarrhythmic.
Despite repeated defibrillations and severe left
ventricular dysfunction, our patient made a good recovery with
aggressive supportive treatment. It is imperative that practising
paediatricians are well versed with Pediatric Advanced Life Support
guidelines to manage these challenging resistant arrhythmias.
Contributors: All authors were involved in management
of the patient and manuscript preparation.
Funding: None; Competing interests: None
stated.
References
1. Clausen H, Pflaumer A, Kamberi S, Davis A.
Electrical storm in children. Pacing Clin Electrophysiol. 2013;36:
391-401.
2. Proietti R, Sagone A. Electrical storm: Incidence,
prognosis and therapy. Indian Pacing Electrophysiol J. 2011;11:34-42.
3. Brooks WW, Conrad CH, Morgan JP. Reperfusion
induced arrhythmias following ischaemia in intact rat heart: role of
intracellular calcium. Cardiovasc Res. 1995;29:536-42.
4. Tribulova N, Seki S, Radosinska J, Kaplan P, Babusikova
E, Knezl V, et al. Myocardial Ca2+ handling and cell-to-cell
coupling, key factors in prevention of sudden cardiac death. Can J
Physiol Pharmacol. 2009; 87:1120-9.
5. Schmidt TD, Muir AJ. A case of electrical storm in
a liver transplant patient. Transplant Proc. 2003;35:1437-8.
6. D’Aloia A, Faggiano P, Brentana L, Boldini A, Curnis
A, Bontempi L, et al. Recurrent ventricular fibrillation during a
febrile illness and hyperthermia in a patient with dilated
cardiomyopathy and automatic implantable cardioverter defibrillator. An
example of electrical storm. Int J Cardiol. 2005;103:207-8.
7. Kowey PR. An overview of antiarrhythmic drug
management of electrical storm. Can J Cardiol. 1996;12:3-8B.
8. Nademanee K, Taylor R, Bailey WE. Treating
electrical storm: sympathetic blockade versus advanced cardiac life
support-guided therapy. Circulation. 2000;102:742-7.
9. El-Sherif N. The challenge of management of
electrical storm out-of-hospital cardiac arrest. Cardiol J. 2007;
14:326-8.
10. Manolis A, Katsivas A, Vassilopoulos C, Tsatiris
C. Electrical storm in an ICD-recipient with 429 delivered appropriate
shocks: therapeutic management with antiar-rhythmic drug combinations. J
Interv Card Electrophysiol. 2002;6:91-4.
|
|
|
 |
|

