|
|
|
Indian Pediatr 2013;50: 771-773 |
 |
Comparison of New Ballards Score and Parkins
Score for Gestational Age Estimation
|
|
Kavita Sreekumar, Annely d’Lima, Saudamini Nesargi,
Suman Rao and Swarnarekha Bhat
From the Division of Neonatology, Department of
Pediatrics, St. Johns Medical College,
Bengaluru, India.
Correspondence to: Dr Kavita Sreekumar, Lecturer,
Department of Pediatrics, Goa Medical College, Bambolim, Goa 403 202.
Email: [email protected]
Received: January 09, 2012;
Initial review: February 08, 2012;
Accepted; November 04, 2012.
|
|
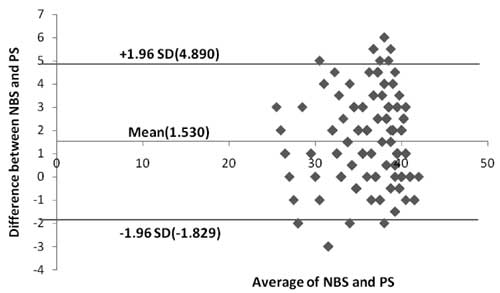
This prospective analytical study was
done to compare the accuracy of New Ballards score (NBS) and Parkins
score (PS) in assessing the gestational age (GA) in newborns. The GA of
284 babies was assessed by the NBS and PS within 24 hours of birth. The
two methods of assessment were compared using the Bland Altmann Plot.
The mean difference between the two measurements was 1.530576. 95% of
the values lay within the limits of agreement which are -1.82982 and
4.890974. The two methods are found to be in acceptable agreement.
Parkins score enables us to easily assess the gestational age of babies
within ±12 days, especially in sick and preterm babies.
Key Words: New Ballards score,
Gestational age, Parkins score.
|
|
In the newborn infant, it is essential to know the
correct gestational age, so as to evaluate the risk of morbidity and
mortality. In all newborn units, the New Ballards Scores (NBS) is
primarily used to assess the gestational age. Many of the neurologic
criteria are difficult to assess in sick infants or those in incubators.
The Parkins Score (PS) uses only four external characteristics i.e. skin
texture, skin colour, ear firmness and breast size, thus making it easy
for practical use [1]. In this study, we attempt to determine the
accuracy of the physical criteria in assessing the gestational age of
the babies, so that the errors caused by Ballards Score due to impaired
neurological states is avoided.
Methods
This was a prospective analytical study conducted in
the level III NICU and postnatal wards of St. Johns Hospital, Bengaluru,
for a study period of 6 months, from March to September 2009. Babies
whose GA estimate was available by last menstrual period (LMP) and/or
first trimester ultrasonography scan were included. Babies whose
obstetric estimate differed from NBS by more than 2 weeks were excluded.
350 babies needed to be assessed assuming that there is a correlation of
0.75 between the NBS and the PS [1]. The assessments were done by two
different investigators: one for NBS and the other for the PS, within 24
hours of life. The investigators were blinded to the GA estimate of the
mother. One independent assessor did the NBS and confirmed that NBS and
Obstetric score match. These subjects were included in the study and
were assessed by the PS by the other investigator.
The study protocol was approved by the Institutional
ethics committee of the St. Johns Medical College and Hospitals. Data
were entered and analyzed in SPSS version 11.5. The two different
methods were compared using the Bland Altmann Plot [2]. The mean
difference between the two methods was calculated and the standard
deviation of the mean was found. The limits of agreement was calculated
using the formula: mean ± 1.96SD. The average of the two scores was
plotted against the difference between the two readings for each sample.
Results
The number of subjects enrolled in the study was 284,
which gives the study a power of 80%. The characteristics of study
subjects can be seen in Table I. All neonates were
examined within 1 to 29 hours of life (mean 14.7 hours). The mean
gestational age by dates/usg was 36.2 weeks, by NBS was 36.1 (SD-3.31)
and by PS was 37.6 (SD-4.06). The mean difference between Obstetric GA
and NBS was 0.04 weeks (<1 day), Obstetric GA and PS was 1.5 weeks (12
days) and GA by NBS and Parkins was 1.5 weeks (12 days). The standard
deviation of the mean difference was 1.68. The limits of agreement were
-1.82982 and 4.890974. When the average of the NBS and PS scores were
plotted, 95% of the values were found to lie within the limits of
agreement. The mean difference between the NBS and PS in sick babies was
1.5 weeks.
TABLE I Characteristics of Subjects (N=284)
|
Characteristics
|
No. (%) |
Range |
|
Birth weight (g)* |
2262 |
440-4200 |
|
GA by dates/USG (wks)* |
36.2 |
24-41.2 |
|
Males |
145(51) |
|
|
Females |
139(4) |
|
|
Intramural |
271(95) |
|
|
Small for gestational age |
85(30) |
|
|
Appropriate for gestational age |
195(68.6) |
|
|
Large for gestational age |
4(1.4) |
|
|
Extremely low birth weight |
16(5.6) |
|
|
Very low birth weight |
40(14) |
|
|
Low birth weight |
102(35.9) |
|
|
Normal birth weight |
130(45.7) |
|
|
Macrosomia
|
1(0.35) |
|
|
Spontaneous vaginal
|
147(51.6) |
|
|
Forceps extraction
|
3(0.6) |
|
|
Cesarean section
|
138(48.5) |
|
|
1 min APGAR score <7 |
60(21.1) |
|
|
5 min APGAR score <7 |
5(1.7) |
|
|
Normal newborns |
188(66.1) |
|
|
Sick newborns |
96(33.8) |
|
|
*Mean (range). |
Discussion
There clearly is a need for a method of estimating
gestational age which should not upset ill babies, and in order to
distinguish between preterm and small for dates babies it should not be
affected by the quality of intrauterine growth [3]. Parkins, et al.
assessed the accuracy of various physical characteristics in comparison
to the neurological criteria used in the Dubowitz score. They
recommended a score consisting of four physical characteristics to
assess the gestational age of babies. In 1979, Ballards, et al.
[4] modified the Dubowitz score to develop a simplified score for
assessment of fetal maturation of newly born infants. In this study, we
compared the accuracy of the PS with the NBS in assessing the
gestational age in normal and sick babies.
 |
|
Fig.1 Bland Altmann plot of the
average and difference between the NBS and PS along with the
limits.
|
GA assessment was performed at mean time of 14 hours
7 minutes, thus avoiding factors that decrease the accuracy of physical
criteria [5]. In this study, GA assessment by NBS was found to be more
accurate than PS. Another study done by Erman, et al. [6]
also found NBS more accurate compared to Dubowitz score. Moreover, to
examine preterms less than 28 weeks, NBS gives a more accurate estimate
of gestational age. In our study, there were 16 babies with GA less than
30 weeks when assessed by NBS, but when assessed by the PS there were
only 9 babies less than 30 weeks. This limitation was also observed by
Parkin, et al. [1]. Since two is the lowest score in the
PS, which corresponds to a GA of 30 weeks, the confidence with which GA
can be assessed in a baby who scores two or less is uncertain. 95%
confidence limits for prediction of GA from the sum of the scores for
the 4 most reliable characteristics in the study done by Parkin, et
al. [1] was ±15 days, which is similar to the mean difference
obtained in the present study. The results obtained by applying the
Bland Altmann plot showed that there is a similarity between the NBS and
PS. Most of the values were within the limits of agreement. Hence, the
PS can be used to assess gestational age easily in babies, especially in
preterm and sick babies, but with an accuracy of ±12 days.
Contributions: SRB conceived and designed the
study, SR and SN supervised the data collection and reviewed the
manuscript, KS and AD collected the data, KS reviewed the literature and
prepared the manuscript. The final manuscript was approved by all
authors.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
• The Parkins score
correlates well with the gestational age and can be used for
assessment, particularly in sick newborns.
|
References
1. Parkin JM, Hey EN Clowes JS. Rapid assessment of
gestational age at birth,. Arch Dis Child. 1976;51:259-63.
2. Bland JM, Altman DG. Measuring agreement in method
comparison studies. Stat Methods Med Res. 1999;8: 135–60.
3. Farr V, Kerridge DF, Mitchell RG. The value of
some external characteristics used in the assessment of gestational age
at birth. Dev Med Child Neurol. 1966;8:657-60.
4. Ballard JL, Novak KK, Driver M, A simplified score
for assessment of fetal maturation of newly born infants. J Pediatr.
1979;95:769-74.
5. Lepley CJ, Gardner SL, Lubchenco LO. Initial
nursery care: Assessment of gestational age. In: Merenstein GB,
Gardner SL, editors. Handbook of Neonatal Intensive Care. 3rd ed. St.
Louis: Mosby Year Book; 1993. p.76-99.
6. Erman, Wayan R, Soetjiningsih. Clinical
gestational age assessment in newborns using the new Ballard
score. Paediatr Indones. 2006;46:97-102.
|
|
|
 |
|

