|
|
|
Indian Pediatr 2011;48: 633-636 |
 |
An Observational, Health Service Based Survey
for Missed Opportunities for Immunization |
|
Mamta Muranjan, Chhaya Mehta and *Abhijit Pakhare
From the Departments of Pediatrics and *Preventive and
Social Medicine, Seth GS Medical College and KEM Hospital, Parel, Mumbai,
India.
Correspondence to: Dr Mamta Muranjan, 3rd floor, Suman
Apartments, 16 B, Naushir Bharucha Road,
Tardeo, Mumbai 400 007, India.
Email: [email protected]
Received: September 22, 2010;
Initial review: September 24, 2010;
Accepted: December 03, 2010.
Published online: 2011 May 30.
PII: S09747559INPE000272-2
|
|
Abstract
Studies cite missed opportunities for immunization (MOI)
as a contributor to under-vaccination. The present prospective survey
aimed at determining the magnitude of MOI, its contribution to
under-vaccination, and identifying risk factors for MOI. Mothers of 1384
indoor patients £6 years were
interviewed. There were 266 (19.2%) children with MOI, accounting for
79.6% of under-vaccination and 93% of under-vaccination time. MOI
occurred significantly more often with home delivery (P <0.001,
Odds ratio 5.1), incomplete or incorrect maternal knowledge of
immunization (P=0.001, Odds ratio 4.8) and, general practice and
non-Pediatric/ non-Medical college based practice (P=0.001, Odds
ratio 4.0). The impact of sociodemographic factors on likelihood of MOI
was not significant.
Key words: Causes, India, Missed, Under-vaccination,
Opportunities.
|
|
M
issed opportunities for immunization (MOI) is defined as missing
the benefit of getting immunized by the partially or unimmunized child,
during a visit to the health facility for check up or illness, when there
is no particular contraindication for that particular immunization as per
the National Policy [1]. The global magnitude of MOI is 0 to 99% [2] and
9-81% in India [1,3-5]. Reducing MOI is the easiest and immediate remedy
to improve vaccine coverage at no extra cost, by exploiting existing
resources [2]. There is, therefore, an urgent need to examine the
magnitude and factors responsible for MOI, to rapidly achieve the National
immunization targets. We conducted this study to determine the magnitude
and risk factors at a tertiary care institution.
Methods
Over a period of one year, consecutive indoor patients
who fulfilled the inclusion criteria (age
£6 years, availability
of the mother and road to health card, Government of India card or private
physician’s card or verbal recall of the mother as proof of immunization,
and proof of a previous visit to a health care facility) were recruited
after approval by the Institutional Ethics Committee and obtaining
informed consent. Patients dying during admission and under-vaccinated
children without a prior health care visit were excluded. The mother was
interviewed within 24 hours of admission to avoid bias caused by
immunization related intervention. Demographic data and information about
the health care facility visit (type of service and qualifications of the
attending physician, reason for the visit, previous visits with dates if
available for present or prior complaints and diagnosis at those visits)
were recorded. The interview also assessed whether the immunization card
had been reviewed or immunization history elicited at a prior visit,
whether any contraindication to vaccination was present then and in
absence of a contraindication, whether the child had been vaccinated or
immunization related information given to the parent. Data recorded for
Universal Immunization Program (UIP) vaccines was dates of immunization
and age at administration of the vaccine. Difference between the recommended
age and the actual age of immunization and the number of weeks past due
was determined for each under-vaccinated child for every vaccination. For
under-vaccinated children with MOI, the number of weeks accounting for MOI
was calculated by the total time overdue for each child with MOI. An
estimate of the number of weeks of under-vaccination accounted by MOI and
the proportion of under-vaccination attributable to MOI was calculated.
Children detected to have MOI were referred to the immunization clinic for
the due vaccination. The data was analyzed using the Chi square test for
univariate analysis and logistic regression for multivariate analysis (SPSS
software version 15). All analysis was carried out at 5% significance (P<0.05).
Results
Inclusion criteria were fulfilled by 1401 amongst 4196
indoor admissions. Seventeen children less than 8 weeks of age were
excluded (not yet beyond time when eligible). Thus, 1384 children were
analyzed (60.5% males). The mean age was 100.7 ±88 weeks (range 3.7-312.9
weeks). At least one vaccine was received by 1296 (93.6%), 88 (6.4%) were
unimmunized and 1050 (76%) children were fully immunized (UIP schedule)
[877 (63.5%) age appropriate immunization, 173 (12.5%) up to date but not
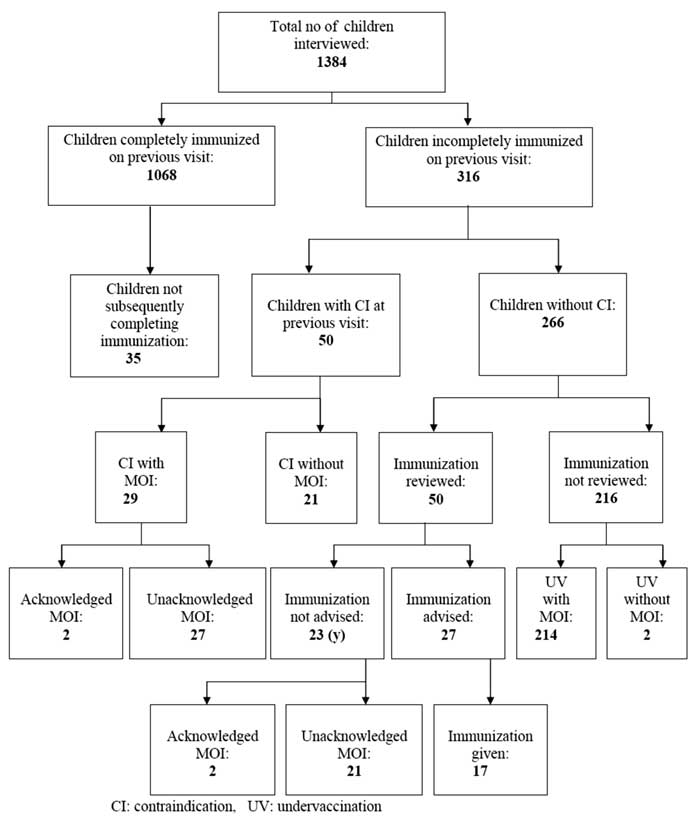
age appropriately immunized]. The immunization status is presented in
Fig.1.
 |
|
Fig. 1 Immunization status of the study population.
|
Under-vaccination was observed in 24% of children
(334). MOI accounting for 79.6% of under-vaccination was present in 266
(19.2%). Almost all MOI (98.5%) were unacknowledged. Sixty-eight cases
(4.9%) were under-vaccinated but without a MOI. For a child with MOI, if
each vaccine missed was considered as a missed opportunity, then 1243
vaccinations were missed (4.67 missed vaccinations child). If each visit
when vaccination was missed was considered a missed opportunity, 702
visits were associated with MOI (2.64 missed opportunities child).
Median age at vaccination and the difference between
recommended and actual age of vaccination could be determined in 96
children with MOI having records with date of vaccination (Table
I). Of 2473.1 weeks of under-vaccination, MOI accounted for 2299
weeks. The proportion of under-vaccination weeks attributable to MOI was
92.9%.
Table I
Median Age and Difference Between Recommended and Actual Age of Vaccination in
Children with MOI (n=96)
|
Vaccine |
Median age (weeks) |
Difference (weeks) |
|
BCG |
1.7 |
5.5 |
|
OPV/DPT1 |
8 |
0.8 |
|
OPV/DPT2 |
13.7 |
2.2 |
|
OPV/DPT3 |
18.4 |
2.5 |
|
Measles |
42.7 |
1.1 |
|
MOI: Missed opportunities for immunization |
The demographic parameters of children with MOI (n=266)
were comparable to those who were under-vaccinated (n=68) in terms
of gender, religion, birth order, residence, maternal age, and
socio-economic status. MOI occurred during a visit for an acute illness in
80.5% of cases, for a chronic disease in 18.8% and a well child visit in
0.7%. The type of health facility visited was general practice (45.5%),
medical college (23%), practicing pediatrician (15.4%), public health
facility (6%), private institution (8.6%) and an alternative medical
practice (1.5%). The qualification of the health care provider was MBBS
(50.4%), post-graduate degree in Pediatrics (43.6%), degree in alternative
medicine (3.4%) and super-specialty or non-Pediatric degree (2.6%). The
reasons for MOI were immunization history not reviewed (94%), false
contraindication (2.2%), wrong immunization history (1.5%), physician not
advising immunization (1.1%), unavailability of immunization card (0.7%),
and visit not on ‘immunization day’ (0.5%).
MOI occurred significantly more often with home
delivery, incomplete or incorrect maternal knowledge of immunization, and
general practice and non-Pediatric/ non-Medical college based practice
[odds ratios: 5.1 (95% CI 2.3, 11.0), 4.8 (95% CI 1.2, 18.5) and 4.0 (95%
CI 1.9, 8.3), respectively]. Testing with Hosmer and Lemeshow goodness of
fit test indicated fitness of data in the model.
Discussion
The present study documents that 80% of
under-vaccination and 93% of under-vaccination time was due to MOI,
occurring during acute illness visits. Almost all MOI were unacknowledged,
attributable to oversight on the part of the health care provider in
obtaining history of immunization in 94% of cases. This underscores the
necessity of implementing interventions in office practice to reduce MOI
including screening a child for eligibility at every preventive or
curative visit, a tracking system to alert the physician when immunization
is due, recording dates of immunization, and ensuring caregivers carry the
immunization card at every visit [2]. Similarly, every hospital admission
must be exploited as an opportunity to immunize the eligible or advise the
due vaccine at discharge.
Previous studies have implicated provider
misconceptions like avoiding immunization during minor illness as a
significant predictor for MOI [6]. Though illness characteristic was not
significantly predictive of MOI in this study, the likelihood of MOI was
higher with visits to non-Pediatric/non-Medical college based practice
including General Practitioners. This is relevant as a large proportion of
health care delivery in India is by General Practitioner, who often are
the first and only contact for patients [7, 8]. Their correct compliance
with the National vaccination policy is critical for its success. Our
study draws attention to the urgency of corrective measures to encourage
desirable immunization practices such as simultaneous vaccination, safety
of vaccination during mild acute illness and knowledge of true
contraindications amongst other practitioners [2].
Earlier studies have documented that maternal knowledge
about vaccines and contraindications for immunization was sub-optimal
[9-11]. Many harbored erroneous beliefs and misconceptions, especially
about vaccinating during acute illness [6, 9-14]. However, maternal
acceptability of immunization was documented to be high in those with MOI
[3]. Therefore education about the diseases being targeted, nature and
timing of vaccines, their benefits and adverse effects, and acceptance of
immunization during minor febrile illnesses will be critical to empower
mothers to demand vaccination and reduce drop-out [6,11-13,15].
In conclusion, MOI can be tackled by accomplishing the
National population policy target of 80% institutional deliveries [16],
empowering mothers to demand immunization [6,9,17] and ensuring optimum
immunization delivery by general practitioners. Periodic surveys for MOI
should be a performance indicator for delivery and utilization of
immunization services in the country [2,19].
Acknowledgment: The authors thank Dr Sanjay Oak,
Director (Medical Educations and Major Hospitals, Municipal Corporation of
Greater Mumbai) and Dean of Seth GS Medical College and KEM Hospital for
granting permission to publish the paper.
Contributors: MNM designed the study, supervised
the data collection and analysis, and wrote the manuscript. MNM will act
as guarantor of the paper. CM collected and analyzed the data and prepared
the draft. AP performed the statistical analysis and helped in drafting
the manuscript.
Funding: None.
Competing interests: None stated.
|
What This Study Adds?
• Missed opportunities for immunization with a
magnitude of 19.2% was responsible for 80% of under-vaccination and
93% of under-vaccination time.
• Home delivery, incomplete or incorrect maternal
knowledge of immunization and general practice and non-Pediatric/
non-Medical college based practice were highly predictive of missed
opportunities of immunization.
|
References
1. Deivanayagam N, Nedunchelian F, Mala N, Ashok TP,
Rathnam SR, Ahmed SS. Missed opportunities for immunization in children
under 2 years attending an urban teaching hospital. Indian Pediatr.
1995;32:51-7.
2. Hutchins SS, Jansen HAFM, Robertson SE, Evans P,
Kim-Farley RJ. Studies of missed opportunities for immunization in
developing and industrialized countries. WHO Bullet OMS. 1993;71:549-60.
3. Nirupama S, Chandra R, Srivastava VM. A survey of
missed opportunities for immunization in Lucknow. Indian Pediatr.
1992;29:29-32.
4. Mitra J, Manna A. An assessment of missed
opportunities for immunization in children and pregnant women attending
different health facilities of a state hospital. Indian J Public Health.
1997;41:312.
5. Grant JP. The State of the World’s Children 1990.
UNICEF. Oxfordshire: Oxford University Press; 1990.
6. Wood D, Schuster M, Donald-Sherbourne C, Duan N,
Mazel R, Halfen N. Reducing missed opportunities to vaccinate during child
health visits. Arch Pediatr Adolesc Med. 1998:152:238-43.
7. Goyal RC, Sachdeva NL, Role of general practioners
in primary health care. J Indian Med Assoc.1996;94:60-1.
8. Chansoria M, Taluja RK, Mukerjee B, Kaul KK. A study
of immunization status of children in a defined urban population. Indian
Pediatr. 1975;12: 879-88.
9. Kekre MM, Mohammad AS, Pruthvish S, Misquith D.
Speeding up universal immunization programme. Indian Pediatr.
1988;25:636-41.
10. Manjunath U, Pareek RP. Maternal knowledge and
perceptions about the routine immunization programme – a study in a
semi-urban area in Rajasthan. Indian J Med Sci. 2003;57:158-63.
11. Murthy GVS, Kumar S. Knowledge of mothers regarding
immunization in a high coverage area-need for strengthening health
education. Indian Pediatr. 1989;26: 1219-22.
12. Smith PJ, Chu SY, Barker LE. Children who have
received no vaccines: Who are they and where do they live? Pediatrics.
2004;114:187-95.
13. Bhandari B, Mandowara SL, Gupta GK. Evaluation of
vaccination coverage. Indian J Pediatr. 1990;57:197-202.
14. Bates AN, Wolinsky FD. Personal, financial, and
structural barriers to immunization in socioeconomically disadvantaged
urban children. Pediatrics. 1998;101:591-6.
15. Agarwal S, Bhanot A, Goindi G. Understanding and
addressing childhood immunization coverage in urban slums. Indian Pediatr.
2005;42:653-63.
16. National Population Policy 2000. New Delhi.
Ministry of Health and Family Welfare, Government of India. 2000.
17. Kim SS, Frimpong JA, Rivers PA, Kronenfeld JJ.
Effects of maternal and provider characteristics on up-to-date
immunization status of children aged 19 to 35 months. Am J Public Health.
2007;97:1-8.
|
|
|
 |
|

