|
|
|
Indian Pediatr 2011;48:
607-611 |
 |
Early Neonatal Morbidities in Late Preterm
Infants |
|
Ashish Jaiswal, Srinivas Murki, Pramod Gaddam and Anupama Reddy
From Fernandez Hospital, Hyderabad.
Correspondence to: Dr Srinivas Murki, Consultant
Neonatologist, Fernandez Hospital,
Hyderabad, Andhra Pradesh 503 001, India.
Email:
[email protected]
Received: February 05, 2010;
Initial review: March 03, 2010;
Accepted: June 28, 2010.
Published online: 2010
November 30.
PII: S097475591000124-1
|
Objectives: To compare early neonatal morbidity (within first 7 days
of life) in late preterm infants with term infants.
Study design: Prospective cohort study.
Subjects: All live inborn late preterm infants (34
0/7 to 36 6/7 weeks) and term infants (37 0/7 to 41 6/7 weeks).
Outcome: Any of the predefined medical conditions
listed in the study, resulting in post- delivery inpatient hospital
observation, admission, or readmission in first 7 days of life.
Results: 363 late preterm infants and 2707 term
infants were included in study. Two hundred fifty seven (70.8 %) of late
preterm and 788 (29.1%) of term infants had at least one of the predefined
neonatal conditions. Late preterm infants were at significantly higher
risk for overall morbidity due to any cause (P<0.001; adjusted Odds
Ratio (OR): 5.5; 95% CI: 4.2-7.1), respiratory morbidity (P<0.001;
adjusted OR: 7.5; 95% CI: 4.2-12.3), any ventilation (non invasive or
invasive) (P=0.001; adjusted OR: 4.2; 95% CI: 2-8.9), jaundice (P<0.001;
adjusted OR: 3.4; 95% CI: 2.7-4.4), hypoglycemia (P<0.001; adjusted
OR: 4.5; 95% CI: 2.6-7.7), and probable sepsis (P<0.001; adjusted
OR: 3.2; 95% CI: 1.6-6.5). The incidence of morbidities increased from 23%
at 40 weeks to 30%, 39.7%, 67.5%, 89% and 87.9% at 38, 37, 36, 35 and 34
weeks, respectively (P<0.001).
Conclusion: Compared with term infants, late
preterm infants are at high risk for respiratory morbidity, need of
ventilation (non invasive or invasive), jaundice, hypoglycemia, sepsis,
and probable sepsis. All gestations except 39 weeks were at significantly
higher risk for morbidity with 40 weeks as reference term.
Key words: India, Late preterm infants, Neonatal morbidity,
Outcome.
|
|
L
ate preterm infants (34 0/7 through
36 6/7 weeks of gestation) are physiologically less mature and have
limited compensatory responses to the extra-uterine environment, compared
with term infants. Although late preterm infants are the largest subgroup
of preterm infants, there has been little research on this group until
recently. This is mainly because of labeling them as ‘‘near-term’’, thus
being looked upon as ‘‘almost mature,’’ with little need to be concerned.
However, recent research has revealed a contrary trend [1-4]. While
serious morbidities are rare, the late preterm group has 2 to 3 fold
increased rates for mild to moderate morbidities, such as hypothermia,
hypoglycemia, delayed lung fluid clearance and respiratory distress, poor
feeding, jaundice, infection, and readmission rates after initial hospital
discharge [1]. As the late preterm subgroup accounts for nearly 10% of all
births, even a modest increase in any morbidity will have a huge impact on
the overall health care resources. Thus, it is not surprising that the
absolute number of late preterm infant being admitted to NICUs has been
increasing worldwide. Only few studies have been conducted to assess the
neonatal morbidity and mortality in late preterm infants [1-4]. These were
done in developed countries and were retrospective in nature.
Understanding morbidity risk among late-preterm infants
is not only important for helping newborn care providers to anticipate and
to manage potential morbidity during the birth hospitalization and earlier
follow-up after hospital discharge, but also may possibly assist in
guiding non-emergency obstetric intervention decisions. The present study
is an attempt to obtain actual data on incidence, pattern of early
neonatal morbidities, and to compare it with term infants.
Methods
This hospital-based prospective cohort study was
conducted at the Fernandez Hospital, Hyderabad, an urban private tertiary
care women and newborn hospital. The study was approved by the hospital
ethics committee. All live inborn late preterm infants (34 0/7 to 36 6/7
weeks) and term infants (37 0/7 to 41 6/7 weeks) [5] born between February
2009 to September 2009 were eligible for enrollment in the study. Informed
parental consent was obtained prior to enrolment in the study. Infants
with major congenital anomalies and those with clinically identified
chromosomal syndromes were excluded. Gestational age was assessed by
maternal last menstrual period and by first trimester ultrasound scan.
A suitable case reporting form (CRF) mentioning
infant’s particulars, risk factors, and neonatal morbidity was developed
for the study. It was pre-tested on 25 infants and modified. All infants
enrolled in study were followed daily till first 7 days of life for any
morbidity by clinical evaluation and reviewing hospital records. Infants
who were discharged before 7 days were called for mandatory follow up
evaluation in the outpatient clinic on 5 th
and 7th day of life. Infants who did not come for follow up were called on
telephone and status of the baby was enquired.
Outcome
Any of the following predefined medical condition
resulting in post delivery inpatient hospital observation, admission or
readmission in first 7 days of life: (i) Post Resuscitation care:
Requirement of post-resuscitation care as per NRP 2005 guidelines. (ii)
Hypoglycemia: Blood glucose of less than 40 mg/dL. Blood sugars were
monitored at 12 hourly intervals in all late preterm, IUGR (intrauterine
growth restriction), IDM (Infant of diabetic mother) and LGA (Large for
gestation, birth weight >2SD) infants. Random blood sugar estimation was
also done in all symptomatic infants as per the clinician’s discretion. (iii)
Jaundice: Clinically visible jaundice requiring phototherapy/exchange
transfusion as per hour specific total serum biluribin (TSB) nomogram (AAP
chart). Criteria for 35 weeks were used for infants with 34 weeks
gestation. (iv) Respiratory distress: Presence of at least 2 of the
following criteria: Respiratory rate >60/min, Subcostal/intercostal
recessions, Expiratory grunt/groaning, and requiring oxygen therapy. (v)
Sepsis: Probable sepsis: Positive septic screen (two of the five
parameters namely, TLC <5000/mm 3
or >15000/mm3, band to total polymorph ratio of >0.2, absolute
neutrophil count less than 1800/mm3 or >7200/mm3, C
reactive protein >0.5mg/dL, platelets <1 lakh/mm3); or Proven
sepsis: Isolation of pathogens from Blood or CSF or Urine. (vi)
Weight loss: If weight loss >10% of birth weight. (vii)
Readmission: Any readmission after post-delivery discharge from hospital.
Statistical analysis
Assuming 5% prevalence of morbidities in term infants
with relative risk of 2 times in late preterm compared with term infants
and allowing standard
a (0.05) and
b
(0.2) error, 275 late preterm infants were to be recruited. Expecting 30%
lost to follow up, 363 infants were enrolled in the study. All data thus
collected were than analyzed using SPSS software. Neonatal morbidities
were compared between late preterm and term infants. Chi-square test and
student ‘t’ test were used for discrete and continuous variables,
respectively. Logistic regression analysis was done with neonatal
morbidity as the dependent variable, and late preterm, mode of delivery,
IUGR and multiple pregnancy status as the covariates. P value <0.05
was considered significant. Chi-square for trends was done for comparing
morbidities across gestational age groups.
Results
There were 3300 live births in hospital during study
period. Of these, 371 (11.24%) were late preterm and 2725 (82.58%) were
term births. Three hundred sixty three (98.65%) of late preterm infants
and 2707 (99.33%) of term infants were included in the study. Twenty two
infants were excluded due to congenital anomalies and in 4 cases parental
consent was refused. All included infants were followed for 7 days of life
for outcomes. On comparing the two groups, there was significant
difference in mean gestation, mean birthweight, weight for gestation, mean
Apgar score, mode of delivery, and multiple pregnancy status (Table
I).
TABLE I
Baseline Variables of The Study Population
|
Variable |
Late preterm (n = 363) |
Term (n = 2707) |
P value |
|
Gestation (wks) mean (SD) |
35.39 (±0.78) |
38.64 (±1.11) |
|
|
Birth weight (Kg) mean (SD) |
2.35 (±0.48) |
3.04 (±0.43) |
|
|
Female sex |
165 (45.5) |
1325 (48.9) |
0.116 |
|
Weight for Gestation
AGA |
304 (83.7) |
2305 (85.1) |
|
|
SGA |
37 (10.2) |
132 (4.9) |
|
|
LGA |
22 (6.1) |
270 (10) |
|
|
Mode of delivery
Vaginal |
117 (32.2) |
1554 (57.4) |
<0.001 |
|
Cesarean |
246 (67.8) |
1153 (42.6) |
|
|
Singleton pregnancy |
297 (81.8) |
2693 (99.5) |
|
|
APGAR at 1 min |
7.43 (±0.8) |
7.72 (±0.7) |
<0.001 |
|
APGAR at 5 min |
8.49 (±0.6) |
8.77 (±0.5) |
<0.001 |
|
AGA: appropriate
for gestational age; SGA: small for gestational age; LGA: large for
gestational age. |
257 (70.8%) of late preterm and 788 (29.1%) of term
infants had atleast one of the neonatal morbidities requiring inpatient
hospital observation, admission or readmission during the first 7 days of
life. On comparing the neonatal morbidity after adjusting for mode of
delivery, intrauterine growth, and multiple pregnancy status; late preterm
infants were at significantly higher risk for overall morbidity due to any
cause, respiratory morbidity, any ventilation (non invasive or invasive),
jaundice, hypoglycemia, probable sepsis, and confirmed sepsis (Table
II). Thirty six (9.9%) late preterm infants and 199 (7.4%) term
infants required readmission in the first 7 days of life (Table
III). As 40 weeks is considered an ideal gestation age for delivery,
neonatal morbidities at each of the lower gestations was compared with
morbidities of neonates born at 40 weeks. The incidence of morbidities
increased from 23% at 40 weeks to 30%, 39.7%, 67.5%, 89% and 87.9% at 38,
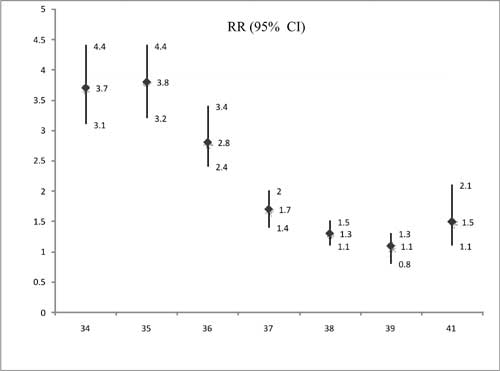
37, 36, 35 and 34 weeks, respectively(Fig. 1).
TABLE II
Comparison of Morbidity in Late Preterm and Term Infants
| Variable |
Late preterm |
Term |
P value |
Adjusted OR |
| |
(n= 363) (%) |
(n= 2707) (%) |
|
(95%CI) |
| Any morbidity |
257 (70.8) |
788 (29.1) |
<0.001 |
5.5 (4.2-7.1) |
| Readmission |
36 (9.9) |
199 (7.4) |
0.056 |
1.9 (1.2-2.8) |
| Hypoglycemia |
32 (8.8) |
39 (1.4) |
<0.001 |
4.5 (2.6-7.7) |
| Respiratory morbidity |
38 (10.5) |
41 (1.5) |
<0.001 |
7.5 (4.2-12.3) |
| Ventilation |
| Any |
11 (3) |
23 (0.8) |
0.001 |
4.2 (2-8.9) |
| CPAP |
9 (2.5) |
15 (0.5) |
|
|
| IPPV |
2 (0.5) |
8 (0.3) |
|
|
| Jaundice |
200 (55.1) |
671 (24.8) |
<0.001 |
3.4 (2.7-4.4) |
| Probable sepsis |
15 (4.1) |
30 (1.1) |
<0.001 |
3.2 (1.6-6.5) |
| Confirmed sepsis |
4 (1.1) |
1 (0.04) |
0.001 |
|
TABLE III
Neonatal Morbidity in the Readmission Group
|
Variable |
Late preterm |
Term |
| |
n=36 (9.9%) |
n=199 |
| Mean age at readmission (d) |
5.53 ± (1.4) |
4.7 ± (1.2) |
| Hypoglycemia |
2 (5.5%) |
7 (3.5%) |
| Respiratory morbidity |
2 (5.5%) |
5 (2.5%) |
| Weight loss >10% |
4 (11%) |
21(10.5%) |
| Jaundice |
32 (88.8%) |
160 (80.4%) |
| Probable sepsis |
5 (13.8%) |
12 (6%) |
 |
|
Fig. 1 Neonatal morbidity: Individual gestation vs reference
term (40 weeks).
|
Discussion
In the present study, 70.8% of late preterm and 29.1%
of term infants had at least one neonatal morbidity requiring inpatient
hospital observation, admission or readmission during the first 7 days of
life. Neonatal jaundice requiring phototherapy (55.1%) followed by
respiratory morbidity (10.5%) and hypoglycemia (8.8%) were the frequently
identified morbidities in late preterm infants while neonatal jaundice
(24.8%) was the most frequently identified morbidity in term infants.
Cesarean delivery, IUGR and multiple pregnancy status significantly
contribute to neonatal morbidities. Compared with term infants, these
variables are more common in late preterm infants. In order to neutralize
the influence of these variables on the outcomes evaluated, adjusted odds
ratios were calculated and were significantly higher in late preterm
group. Compared with term infants, late preterm infants were at 5.5 times
higher risk for overall morbidity due to any cause, 7.5 times higher risk
for respiratory morbidity, 4.2 times higher risk for ventilation (non
invasive or invasive), 3.4 times higher risk for jaundice, and 4.5 times
and 3.2 times higher risk for hypoglycemia and probable sepsis,
respectively.
Similar to our findings, in a retrospective study by
Wang, et al.[1], 77.8% near term infants compared with 45.3%
of term infants had at least one clinical problem and nearly all clinical
outcomes differed significantly between near-term and full-term neonate
viz. temperature instability, hypoglycemia, respiratory distress, and
jaundice. They found that during the initial birth hospitalization, late
preterm infants were 4 times more likely than term infants to have at
least one medical condition diagnosed and 3.5 times more likely to have
two or more conditions diagnosed [1]. Melamed, et al. [6] also
found that compared with full-term infants, spontaneous late preterm
delivery was independently associated with an increased risk of neonatal
morbidity, including respiratory distress syndrome, sepsis,
intraventricular hemorrhage, hypoglycemia, and jaundice requiring
phototherapy. Another study Tomashek, et al. [7] found that late
preterm infants were 1.5 times more likely to require hospital-related
care and 1.8 times more likely to be readmitted than term infants. In
another study, newborn morbidity was 7 times more likely in late preterm
compared with term infants (22% vs 3%) [8]. The higher risk for
neonatal morbidity in our study may be attributed to the inclusion of
neonates of 34 weeks gestation in our data, difference in definition of
morbidities, and a more precise follow-up due to it being a hospital based
prospective study than previous studies, which are either retrospective or
were based on population data.
The incidence of morbidity increased from 24% at 40
weeks to 90% at 34-35 weeks showing an inverse relationship with
gestational age. There was a 10% increase from 38 weeks to 37 weeks, 20%
increase from 37 weeks to 36 weeks and 30% from 36 weeks to 35 weeks. With
40 weeks as reference standard, all gestations except 39 weeks were at
significantly higher risk for morbidity. Bradley, et al. [9]
concluded previously that clinically significant respiratory morbidities
are least common at 39-40 weeks. Roberta De Luca, et al. [10]
similarly found that mortality and morbidities had a strong GA-related
trend with the lowest incidences consistently found between 38 and 40
weeks of gestation. Shapiro-Mendoza, et al. [8] found that the
newborn morbidity rate doubled in infants for each gestational week
earlier than 38 weeks.
The present study is one of the first attempts to
obtain actual data on late preterm births and associated neonatal
morbidities from India. A major limitation of present study is inability
to assess feeding difficulties and breastfeeding status. This was because
of existing policy of the unit to give supplementary feeding to all at
risk infants. As the present study was designed to asses early neonatal
morbidities, it did not address morbidities after 7 days of life, and also
whether outcomes studied had long-term implications. Among the neonatal
units, often there is as a wide variation in antenatal use of steroids,
intrapartum monitoring, feeding policy, asepsis protocols and management
of jaundice/ respiratory distress and hence the results of this study may
be more applicable to settings similar to ours and may not be
generalizable.
The results show that late preterm infants have 5.5
times higher risk for overall morbidity due to any cause relative to term
infants. All gestations except 39 weeks were at significantly higher risk
for morbidity with 40 weeks as reference term.
Contributors: SM designed and supervised the study.
AJ collected and analyzed the data. All the authors contributed in
preparation and approved final manuscript.
Funding: None.
Competing interests: None stated.
|
What is Already Known?
• Late preterm infants are physiologically less
mature than term infants.
What This Study Adds?
• In comparison with term infants, late preterm
infants are at high risk for early neonatal morbidities especially
respiratory morbidity, need of ventilation, jaundice, hypoglycemia
and probable sepsis.
|
References
1. Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical
outcomes of near-term infants. Pediatrics. 2004;114:372-6.
2. Khashu M, Narayanan M, Bhargava S, Osiovich H.
Perinatal outcomes associated with preterm birth at 33 to 36 weeks’
gestation: a population-based cohort study. Pediatrics. 2009;123:
109-13.
3. Mc Intire DD, Leveno KJ. Neonatal mortality and
morbidity rates in late preterm births compared with births at term.
Obstet Gynecol. 2008;111:35-41.
4. Young PC, Glasgow TS, Xi Li, Guest-Warnick G,
Stoddard GJ. Mortality of late-preterm (near-term) newborns in Utah.
Pediatrics. 2007;119:659-65.
5. Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing
care and outcome for late-preterm (near-term) gestations and for
late-preterm infants: a summary of the workshop sponsored by the National
Institutes of Health and Human Development. Pediatrics. 2006;118:1207-14.
6. Melamed N, Klinger G, Tenenbaum-Gavish K, Herscovici
T, Linder N, Hod M, et al. Short term neonatal outcome in low risk,
spontaneous, singleton, late preterm deliveries. Obstet Gynecol.
2009;114:253-60.
7. Tomashek KM, Shapiro-Mendoza CK, Weiss J, Kotelchuck
M, Barfield W, Evans S, et al. Early discharge among late preterm
and term newborns and risk of neonatal mortality. Semin Perinatol.
2006;30:61-8.
8. Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M,
Barfield W, Weiss J, Nannini A, et al. Effect of late-preterm birth
and maternal medical conditions on newborn morbidity risk.
Pediatrics.2008; 121:223-32.
9. Yoder BA, Gordon MC, Barth WH. Late-preterm birth:
Does the changing obstetric paradigm alter the epidemiology of respiratory
complications? Obstet Gynecol. 2008;111:814-22.
10. Luca RD, Boulvain M, Irion O, Berner M, Pfister RE.
Incidence of early neonatal mortality and morbidity after late-preterm and
term cesarean delivery. Pediatrics.2009;123:1064-71.
|
|
|
 |
|

