|
|
|
Indian Pediatr 2011;48:
601-605 |
 |
Early Rescue Administration of Surfactant and
Nasal Continuous Positive Airway Pressure in
Preterm Infants <32 Weeks Gestation |
|
Christos Tsakalidis, Maria Kourti, Paraskevi Karagianni, Dimitris Rallis,
Maria Porpodi and Nikolaos Nikolaidis
From Second NICU and Neonatology Department, Aristotle
University of Thessaloniki, GPN Papageorgiou,
Ring Road Nea Efkarpia, 56403 Thessaloniki, Greece.
Correspondence to: Christos Tsakalidis, Lecturer of
Neonatology, 2nd NICU of Aristotle University of Thessaloniki,
Papageorgiou General Hospital, Ring Road Nea Efkarpia, 56403 Thessaloniki,
Greece.
Email: [email protected]
Received: December 29, 2009;
Initial review: January 22, 2010;
Accepted: June 28, 2010.
Published online: 2010 November 30.
PII: S097475590900898-1
|
Objective: This study reports our institutional
experience on the outcome after prophylactic and early rescue endotracheal
instillation of surfactant within 20 minutes of birth, followed by
extubation and nasal continuous positive airway pressure (NCPAP) in
preterm infants <32 weeks gestational age.
Patients and methods: A total of 142 infants were
prospectively studied (42, gestational age from 23 to 27 and 100, from 28
up to 32 weeks). All infants were electively intubated for administration
of 200mg/kg porcine isolated surfactant (Curosurf, Chiesi Farmaceutici
SPA, Parma, Italy) as soon as practicably possible (within 20 min after
birth) and NCPAP was then initiated.
Results: Extubation and switch to NCPAP at 6h was
successful in 6/42 (14.3%) infants less than 28 weeks gestational age and
75/100 (75%) infants 28-32 weeks gestational age. Out of 81 infants that
were successfully extubated, 76 (93.83%) never required re-ventilation. At
96h of age, need for continuing intubation and ventilation was required by
6/38 (15.8%) alive infants <28 weeks gestational age and 8/100 (8%)
infants 28-32 weeks gestational age. Mean duration of NCPAP post-extubation
was 38±20 hours for infants 23-27 wks and 29±15 hours for infants 28-32
wks gestational age. The mortality rate was 2.81% (4/142).
Conclusion: Implementation of prophylactic or early
rescue administration of surfactant with NCPAP in infants at high risk for
developing RDS in neonatal ICU is a safe modality of respiratory support
in preterm infants.
Key words: Greece, Management, Nasal continuous positive airway
pressure, Outcome, Prematurity, Respiratory distress syndrome, Surfactant.
|
|
Surfactant replacement therapy in
Respiratory distress syndrome (RDS)
improves lung function, decreases
mortality and also results in a better long-term neurodevelopmental
outcome [1,2]. For infants at high risk for RDS, prophylactic intubation
within 15 minutes of age for surfactant administration followed by brief
mechanical ventilation with planned extubation to nasal continuous
positive airway pressure (NCPAP) within one hour has been shown to
significantly improve survival and reduce the incidence of bronchopleural
dysplasia (BPD) or death [3-5].
We report our institutional experience on the outcome
after prophylactic and early rescue endotracheal instillation of
surfactant within 20 minutes of birth of followed by extubation to NCPAP
in preterm infants of <32 weeks gestational age.
Methods
This prospective study was conducted in a level III
neonatal intensive care unit (NICU) following approval by the local ethics
committee, between June 2006 and May 2008. All babies born between 23 and
31 weeks of gestational age were eligible for entry. Infants with
structural cyanotic congenital heart disease, severe congenital
malformations, pulmonary hypoplasia, pneumothorax and Apgar scores less
than 3 at 5 min were excluded. Infants under or equal to 27 weeks
gestation received prophylactic surfactant within 15 minutes of birth. In
infants at risk of RDS with gestational age between 28 and to 32 weeks,
surfactant was administered if a FiO 2
≥40 was needed
to reach SpO2 between 85 and
93% or they exhibited signs of moderate to severe respiratory distress at
age 20 min (early rescue surfactant treatment). Infants who were
administered surfactant either prophylactic or as early rescue treatment
were then switched to NCPAP as early as possible depending on their
respiratory condition.
After parental consent was obtained (either prenatally
or early postnatally), infants were electively intubated for
administration of 200 mg/kg porcine isolated surfactant (Curosurf, Chiesi
Farmaceutici SPA, Parma, Italy) through the tracheal tube as soon as
practicably possible (within 20 min after birth). An umbilical artery
access was gained and a chest X-ray performed. They were extubated
within one hour of birth to NCPAP. Weaning strategies for ventilation
involved a peak inspiratory pressure (PIP) ≤18cm H2O,
FiO2 <40% and rates of 10-20
breaths per minute. The NCPAP was given through nasal prongs using the
Medin Medijet NCPAP generator (Medin Innovations GmbH, Germany).
The initial pressure of CPAP was 6cm H2O
increasing up to a maximum of 8cm H2O
if required aiming to recruit the maximum number of alveoli. The NCPAP was
continued unless any of the following criteria was met (FiO2 >70%, pH<7.2, PaO2<50mmHg,
significant apnea). Echocardiography was performed in all infants at
24-72 hours of life. Cranial ultrasonography was performed within the
first 48 hours of life and repeated at 7 days.
The primary outcome in this study was the need for
mechanical ventilation at 6 hours of birth. Secondary outcomes included
the incidence of bronchopulmonary dysplasia (BPD) defined as need for
oxygen at 28 days of age, the incidence of chronic lung disease (CLD)
(need for oxygen at 36 weeks postmenstrual age), death before discharge,
inci-dence of airleak syndromes (pulmonary interstitial emphysema,
pneumothorax), intraventricular hemo-rrhage, patent ductus arteriosus
(PDA), necrotizing enterocolitis (NEC) and retinopathy of prematurity (ROP)
[6,7]. All infants were followed up for a maximum of two years.
Clinical characteristics and data are described as
median values and range, and as rates and percentages. Data were stored
and analyzed using the SPSS 11.5 statistical software (SPSS, Chicago,
Illinois).
Results
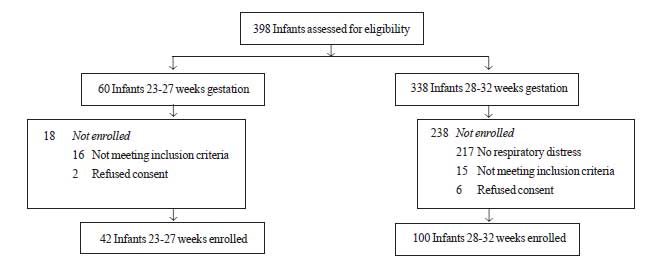
A total of 398 infants of 23-32 weeks gestation were
admitted during the study period. Of these, 256 were not eligible (Fig.
1). Remaining 142 infants were categorized into two subgroups,
gestational age from 23 to 27 weeks (n=42) and from 28 up to 32 weeks (n=100).
The demographic and clinical characteristics of all infants enrolled in the study are
depicted on Table I.
 |
|
Fig. 1 Study flow chart. |
Extubation and switch to NCPAP at 1h was successful in
3/42 (7.1%) infants less than 28 wk gestation and in 72/100 (72%) infants
28-32 wk gestational age. At 6h the proportion of extubated infants was
6/42 (14.3%) and 75/100 (75%) respectively. Out of 81 infants that were
successfully extubated at 6h, 76 (93.83%) never required re-ventilation. A
total of 5 infants required reintubation. Two infants (one 27 wks
gestational age and one 31 wks) required re-ventilation within the first
12h for recurrent apnea. Three infants >28 wks gestational age required
re-ventilation after more than 48h due to septicemia. Four extremely
premature infants (<25 wks gestational age) died within the first 48h of
life, 3 due to sepsis and 1 due to cardiopulmonary failure.
TABLE I
Clinical and Demographic Characteristics of Study Infants
|
Characteristic |
Gestational age 23-27 (n=42) |
Gestational age 28-31 (n=100) |
|
Gender, male |
20 |
52 |
|
Birthweight (g) |
950 (460-1400) |
1350 (900-2080) |
|
Gestational age (wk) |
25 |
30 |
|
Antenatal steroids given |
38 (90%) |
83 (83%) |
|
Peak inspiratory pressure (cm H20) |
18 (14-26) |
17 (15-25) |
|
Arterial blood pH at 1h |
7.34 (7.12-7.51) |
7.33 (7.2-7.46) |
|
FiO2 at study entry |
0.25 (0.21-1) |
0.5 (0.4-1) |
|
FiO2 at 6h |
0.22 (0.21-1) |
0.25 (0.21-1) |
|
FiO2 at 24h |
0.21 (0.21-1) |
0.22 (0.21-1) |
|
Oxygenation index |
7.8 (2.9-27.8) |
7.9 (3.3-26.6) |
|
Apgar at 1 min |
6 (2-9) |
7 (2-9) |
|
Apgar at 5 min |
8 (2-9) |
9 (5-10) |
|
Small for gestational age |
7 (16.7%) |
14 (14%) |
|
All values expressed as median (range). |
At 96h of age, 6/38 (15.8%) alive infants <28 wks
gestational age and 8/100 (8%) infants 28-32 wk required continuing
intubation and ventilation. Mean duration of NCPAP post-extubation was 38
± 20 hours for infants 23-27 wks and 29 ± 15 hours for infants 28-32 wks
gestational age. All infants who remained intubated at 96h had received
antenatal steroid therapy and almost half of them 6/14 (42.8%) were
exposed to chorioamnionitis. Supplemental surfactant was administered in
8/14 infants who remained intubated at 96h. Perinatal asphyxia was evident
in one 27-week-old infant who remained intubated at 96h and received
additional dose of surfactant. Neonatal sepsis was the main reason for
reintubation or death and was proved in 16/142 (11.2%) infants. Secondary
adverse outcomes for both groups are presented in Table II.
TABLE II
Primary and Secondary Outcomes in the Study Infants
| |
Gestational age |
Gestational age |
Total |
| |
23-27 wk (n=42) |
28-31 wk (n=100) |
(n=142) |
|
Extubation at 1h |
3 (7.1%) |
72 (72%) |
75 (52.8%) |
|
Extubation at 6h |
6 (14.3%) |
75 (75%) |
81 (57%) |
| Death |
4 (9.5%) |
0 |
4 (2.81%) |
| Hours
ventilated (mean) |
47.6 |
17.6 |
26.5 |
| Oxygen
requirement at 28 d |
20 (47.6%) |
4 (4%) |
24 (16.9%) |
| 36wk
post-conceptional age |
11 (26.2%) |
4 (4%) |
15 (10.6%) |
| Air leak |
1 (2.4%) |
0 |
1 (0.7%) |
| IVH>II |
3 (7.1%) |
1 (1%) |
4 (2.8%) |
| PVL |
0 |
2 (2%) |
2 (1.45) |
| ROP>II |
7 (16.7%) |
0 |
7 (4.9%) |
| PDA |
2 (4.7%) |
4(4%) |
6 (4.2%) |
| NEC |
0 |
1 (1%) |
1 (0.75) |
IVH: intraventricular hemorrhage; PVL: periventricular leucomalacia; ROP: retinopathy of prematurity;
PDA: patent ductus arteriosus; NEC: necrotizing enterocolitis; All values are presented as numbers (percentage).
|
Discussion
In this study, we implemented the INSURE (INtubate
SURfactant Extubate to CPAP) as prophylactic therapy in infants with
gestational age equal or less than 27 weeks and in preterm infants at high
risk for developing RDS as early rescue treatment. This proved to be a
safe and successful strategy since only 5 out of 81 infants that were
successfully extubated at 6h (6.17%) required reintubation. We also showed
that the number of infants remaining intubated and ventilated at 24h and
96h of age were low (19.85% and 10.14%, respectively). These results are
in agreement with those previously reported with NCPAP [8-12].
An important aspect of this study was the successful
application of INSURE treatment in very small preterm infants. It is
encouraging that a significant number of very preterm infants can benefit
from this strategy. Our results also confirm that NCPAP is a safe method
of ventilation and an important factor in the reduction of aggressive
ventilation and prolonged oxygen therapy decreasing the associated risk.
This is in concordance with earlier studies [8-10,13,14].
The incidence rate of retinopathy of prematurity (ROP)
is low in our study, confirming the reported beneficial result of the
combination of prophylactic surfactant with NCPAP on ROP [9]. Apart from
gestational age, there are other factors important in the etiology of ROP
such as fluctuations of PaO 2,
hyperoxia, pneumothorax and time spent on ventilator [15]. Prophylactic
and early administration of surfactant with NCPAP results in reduced need
for mechanical ventilation, thereby avoiding fluctuations in PaO2
and development of air leak syndromes in premature infants. Moreover, the
incidence of PDA is lower in our study compared with other studies
[8,11,16]. This can be attributed to the short duration of mechanical
ventilation and its effects, confirming the advantages of the application
of NCPAP. Similarly, the reported incidence of PVL in our study was low
and similar to earlier studies [16].
The neonatal mortality rate in our study is 2.8%, that
is in accordance with similar studies reporting on prophylactic surfactant
therapy [8-10]. This outcome might also reflect the low incidence of NEC
and III-IV grade IVH, which constitute major causes of death in premature
infants.
Our results regarding oxygenation at 6h and 24h after
the prophylactic use of surfactant indicate that there was consistently
low requirements for supple-mental oxygen and low incidence of severe RDS.
Moreover, the incidence of pneumothorax and pulmonary emphysema air leak
syndromes is very low in our study (0.7%) which is an expected result of
elimination of mechanical ventilation. These findings are in accordance
with trials reporting on improvement of gas exchange and the severity of
RDS as well as for air leak syndromes after prophylactic surfactant
compared with rescue therapy [17].
In conclusion, implementation of prophylactic or early
rescue administration of surfactant with NCPAP in infants at high risk for
developing RDS in neonatal ICU provides a significantly favorable outcome.
Contributors: All authors contributed equally to
the content of the manuscript.
Funding: None.
Competing interests: None stated.
|
What is Already Known?
•
Prophylactic or early
rescue administration of surfactant and NCPAP are beneficial in
reducing lung injury.
What This Study Adds?
•
Prophylactic or early rescue administration of surfactant and nasal
continuous positive airway pressure in preterm infants is an
effective strategy without adverse effects on outcome and can be
applied to the majority of very preterm infants.
|
References
1. Fujiwara T, Konishi M, Chida S, Okuyama K, Ogawa Y,
Takeuchi Y, et al. The Surfactant-TA Study Group. Surfactant
replacement therapy with a single post ventilatory dose of a reconstituted
bovine surfactant in preterm neonates with respiratory distress syndrome:
final analysis of a multicenter, double blind randomized trial and
comparison with similar trials. Pediatrics. 1990;86:753-64.
2. Walti H, Paris-Lado J, Egberts J, Brand R,
Bevilacqua G, Gardini F, et al. Prophylactic administration of
porcine-derived lung surfactant is a significant factor in reducing the
odds for peri-intraventricular haemorrhage in premature infants. Biol
Neonate. 2002;81:182-7.
3. Gortner L, Wauer RR, Hammer H, Stock GJ, Heitmann F,
Reiter HL, et al. Early versus late surfactant treatment in preterm
infants of 27-32 weeks’ gestational age: a multicenter controlled clinical
trial. Pediatrics 1998;102: 1153-69.
4. Yost CC, Soll RF. Early versus delayed selective
surfactant treatment for neonatal respiratory distress syndrome. Cochrane
Database System Rev. 2000; 2:CD001456.
5. Soll RF, Morley CJ. Prophylactic versus selective
use of surfactant for preventing morbidity and mortality in preterm
infants. Cochrane Database System Rev. 2002;1: CD000510.
6. Walsh MC, Kliegman RM. Necrotizing enterocolitis:
treatment based on staging criteria. Pediatr Clin North Am.
1986;33:179-201.
7. An international classification of retinopathy of
prematurity. Prepared by an International Committee. Br J Opthalmol.
1984;68:690-7.
8. Dani C, Bertini G, Pezzati M, Cecchi A, Caviglioli
C, Rubalteli FF. Early extubation and nasal continuous positive airway
pressure after surfactant treatment in preterm infants of less than 30
weeks’s gestation. Pediatrics. 2004;113:560-3.
9. Haberman B, Shankaran S, Stevenson DK, Papile LA,
Stark A, Korones S, et al. Does surfactant and immediate extubation
to nasal continuous positive airway pressure reduce use of mechanical
ventilation? Pediatric Res. 2002; 51:349A.
10. Reininger A, Khalak R, Kendig JW, Ryan RM, Stevens
TP, Reubens L, et al. Surfactant administration by transient
intubation in infants 29-35 weeks’ gestation with respiratory distress
syndrome decreases need of later mechanical ventilation: a randomised
controlled trial. J Perinatol. 2005;25:703-8.
11. The Texas Neonatal Research Group 2004. Early
surfactant for neonates with mild to moderate respiratory distress
syndrome: A multicenter randomised trial. J Pediatr. 2004; 144:804-8.
12. Tooley J, Dyke M. Randomized study of nasal
continuous positive airway pressure in the preterm infant with respiratory
distress syndrome. Acta Paediatr. 2003;92: 1170-4.
13. Merritt TA, Cochrane CG, Holcomb K, Bohl B, Hallman
M, Strayer D, et al. Elastase and alpha 1 proteinase inhibitor
aspirates during RDS. Role of inflammation in the pathogenesis of BPD. J
Clin Invest. 1983;72:656-66.
14. Payne N, LaCorte M, Karna P, Chen S, Finkelstein M,
Goldsmith J, et al. Reduction of bronchopulmonary dysplasia after
participation in the Breathsavers Group of the Vermont Oxford Network
Neonatal Intensive Care Quality Improvement Collaborative. Pediatrics.
2006;118 Suppl 2: S73-S77.
15. Flynn JT, Bancalari E, Snyder ES, Goldberg RN,
Feuer W, Cassady J, et al. A cohort study of transcutaneous oxygen
tension and the incidence and severity of retinopathy of prematurity. N
Engl J Med. 1992;326:1050-4.
16. Verder H, Robertson B, Greisen G, Ebbesen F,
Albertsen P, Lundstrøm K, et al. Surfactant therapy and nasal
continuous positive airway pressure for newborns with respiratory distress
syndrome. N Engl J Med. 1994;331: 1051-55.
17. Stevens TP, Blennow M, Myers EH, Soll R. Early
surfactant administration with brief ventilation vs selective surfactant
and continued mechanical ventilation for preterm infants with or at risk
for respiratory distress syndrome. Cohrane Database Syst Rev. 2007;4:
CD003063.
|
|
|
 |
|

