|
|
|
Indian Pediatr 2010;47: 709-718 |
 |
Efficacy and Safety of Therapeutic Nutrition
Products for Home Based Therapeutic Nutrition for Severe Acute
Malnutrition: A Systematic Review |
|
Tarun Gera
From the Department of Pediatrics, Fortis Hospital,
Shalimar Bagh, New Delhi, India.
Correspondence to: Dr Tarun Gera, B-256, Derawala
Nagar, Delhi 110 009, India.
Email: [email protected]
|
|
Abstract
Context: Severe acute malnutrition (SAM) in
children is a significant public health problem in India with associated
increased morbidity and mortality. The current WHO recommendations on
management of SAM are based on facility based treatment. Given the large
number of children with SAM in India and the involved costs to the
care-provider as well as the care-seeker, incorporation of alternative
strategies like home based management of uncomplicated SAM is important.
The present review assesses (a) the efficacy and safety of home
based management of SAM using ‘therapeutic nutrition products’ or ready
to use therapeutic foods (RUTF); and (b) efficacy of these
products in comparison with F-100 and home-based diet.
Evidence Acquisition: Electronic database
(Pubmed and Cochrane Controlled Trials Register) were scanned using
keywords ‘severe malnutrition’, ‘therapy’, ‘diet’, ‘ready to use foods’
and ‘RUTF’. Bibliographics of identified articles, reviews and books
were scanned. The information was extracted from the identified papers
and graded according to the CEBM guidelines.
Results: Eighteen published papers (2 systematic
reviews, 7 controlled trials, 7 observational trials and 2 consensus
statements) were identified. Systematic reviews and RCTs showed RUTF to
be at least as efficacious as F-100 in increasing weight (WMD=3.0
g/kg/day; 95% CI -1.70, 7.70) and more effective in comparison to home
based dietary therapies. Locally made RUTFs were as effective as
imported RUTFs (WMD=0.07 g/kg/d; 95% CI=-0.15, 0.29). Data from
observational studies showed the energy intake with RUTF to be
comparable to F-100. The pooled recovery rate, mortality and default in
treatment with RUTF was 88.3%, 0.7% and 3.6%, respectively with a mean
weight gain of 3.2 g/kg/day. The two consensus statements supported the
use of RUTF for home based management of uncomplicated SAM.
Conclusions: The use of therapeutic nutrition
products like RUTF for home based management of uncomplicated SAM
appears to be safe and efficacious. However, most of the evidence on
this promising strategy has emerged from observational studies conducted
in emergency settings in Africa. There is need to generate more robust
evidence, design similar products locally and establish their efficacy
and cost-effectiveness in a ‘non-emergency’ setting, particularly in the
Indian context.
Key words: Efficacy, Management, Severe acute malnutrition,
Therapeutic nutrition product.
|
|
Despite praiseworthy advances in economic
prosperity and in the field of medical therapeutics, malnutrition
continues to be a significant public health problem in India.
Approximately 8.1 million children under the age of 5 years (6.4%) suffer
from severe acute malnutrition (SAM) and it is one of the important
co-morbidities leading to hospital admissions in our country(1). The
mortality associated with severe acute malnutrition is also high, ranging
from 73 to 187 per 1000(2). Needless to say, control and prevention of
severe acute malnutrition should be one of the important priorities of the
health planners. The current recommendations on the management of SAM by
WHO involve initial management at a referral centre for initial
stabilization followed by home therapy(3). Given the number of severely
malnourished children in India and the state of health infrastructure in
the country, particularly in the peripheries, these strategies do not seem
to be logistically feasible. Also, given the complex interplay between
social exclusion, poverty and SAM, inpatient treatment is associated with
un-acceptable costs to the family. In such a situation, uncomplicated
malnutrition is not considered a health problem by the family leading to
delayed institution of appropriate management. This leads to seeking of
health care when the problem is associated with other co-morbidities,
leading to increased mortality.
Given the grimness of the current situation, there is
clearly a need to improve and improvise the current standard guidelines
for the management of SAM in children. One of the suggested methods has
been the use of ‘therapeutic nutrition products’ administered at home to
children with uncomplicated SAM(4). A review was planned to study the
efficacy and safety of various therapeutic nutrition products for home
based management of SAM in children and to critically review the
extendibility of this strategy to India with the following objectives:
(a) to study the efficacy and safety of home
based management of SAM using ‘therapeutic nutrition products’ in
children; and
(b) to compare the efficacy of these products
with F-100 formaulation or home based dietary therapy.
Trials: Systematic Reviews; before and after
observational studies; Individual, cluster, and quasi randomized and
non-randomized controlled trials; consensus statements.
Participants: Children with severe acute
malnutrition.
Intervention: Therapeutic nutrition product,
basically derived from F-100 formulation, which is an integral part of the
WHO Management Protocol for SAM but should have these additional
properties: (i) does not need to be prepared in any form before
consumption; (ii) resists microbial contamination; and (iii)
can be stored at ambient temperature.
Control: No intervention or alternative
intervention such as home based dietary management or facility based
standard treatment.
Outcome Measures: For efficacy: (a)Recovery
rate (as defined by the authors); (b)Weight gain (g/kg/day); and (c)
Relapse.
For Safety: (a) Morbidities like diarrhea,
malaria and respiratory infections; and (b) Mortality.
Identification of studies: An exhaustive
literature search was done in the Cochrane Library and Pubmed using the
search terms ‘severe malnutrition’, ‘therapy’, ‘diet’, ‘ready to use
foods’ and ‘RUTF’ on April 20, 2010.
Review of Evidence
A total of 4073 citations were scanned to identify
relevant studies. The bibliography of identified articles was also scanned
and lateral search strategy in Pubmed was utilised to identify any
additional trials. A total of 18 published studies(4-21) were identified
and the information extracted was graded according to the CEBM
guidelines(22) and is presented in Table I. Wherever
possible and where the data from the published studies was extractable,
the data was pooled statistically to get a precise quantitative estimate.
The pooled estimates of the weighed mean difference (WMD) of the weight
gain between the control and intervention group and the mean pooled weight
gain in observational studies were calculated by meta-analyses using
random effects model assumptions with the "metan" command in STATA
software.
Table I
Role of Therapeutic Nutrition Products in Home Based Management of Severe Acute Malnutrition
in Children: Summary of Evidence
| Author, Year of Publication, Country,
Type of Study, Age, Inclusion Criteria |
Intervention, Sample Size, Duration of
Study |
Salient Findings |
Conclusion, Grade of Evidence |
| Systematic Reviews |
| Bhutta, et al., 2008(4), Pediatric age
group |
Intervention to reduce mother and child
undernutrition and survival; Analyzed data from 21 studies on
management of SAM |
The overall case-fatality rate in 23,
511 unselected severely malnourished children treated in 21
programs of community-based therapeutic care in Malawi, Ethiopia, and
Sudan, between 2001 and 2005,was 4·1%, with a recovery rate of 79·4%
and default of 11·0%. This compares favourably with case-fatality
rates that are typically achieved with facility-based management. |
Use of preprepared balanced foods such
as spreads and ready-to-use supplementary foods is feasible in
community settings.
Grade: 2a |
| Ashworth, et al., 2006(5), Systematic
Review, Malnourished children in non-emergency situations |
Community based rehabilitation for
treatment of severe malnutrition, Analyzed data from 33 studies
of community based rehabilitation |
Eleven (33%) programs were considered
effective. Of the subsample of programs reported since 1995, 8 of 13
(62%) were effective. None of the programs operating within routine
health systems without external assistance was effective. |
When done well, rehabilitation at home
with family foods is more cost-effective than inpatient care, but the
cost effectiveness of ready-to-use therapeutic foods (RUTF) versus
family foods has not been studied. Where children have access to a
functioning primary health-care system and can be monitored, the
rehabilitation phase of treatment of severe malnutrition should take
place in the community. Grade: 2a |
| Controlled Trials
RUTF versus Standard Practice |
Gaboulaud, et al., 2007; Niger(6), 6-59
mo; Inclusion: a) WHZ < -3 z or bilateral pitting edema
b) MUAC < 11cm |
Management at therapeutic feeding centre
(TFC) versus TFC and home based care versus home based care alone
using RUTF; Total: 1937 TFC: 660; TFC and home: 937; Home based: 340 |
(Order: TFC, TFC plus home, home)
Recovery: 52.7, 83.2 and 92.7; Mortality: 18.9, 0.0, 1.7; Default:
28.1, 16.8, 5.6 Transferred: 0.3, 0, 0; Wt gain: 20.8, 10.1, 9.7
g/kg/d |
Satisfactory treatment of SAM can be
achieved using a combination of home and hospital strategies. Children
without complications and preserved appetite may be directly managed
at home. Grade: 2b |
Ciliberto, et al. 2005; Malawi(7);
Quasi-randomized controlled trial; 10-60 mo; Inclusion
a) Moderate and Severe wasting and/or kwashiorkor
b) Absence of severe edema, evidence of systemic infection, or
anorexia |
RUTF versus standard practice (WHO
guidelines) at NRU;Total = 1178; RUTF:992; Standard Therapy: follow up
till 6 mo. |
Recovery (WFH z > -2): 79% versus 46%;
Mean wt. gain:3.5 g/kg/d versus 2.0 g/kg/d; Mortality and relapse:
8.7% versus 16.7%; Lower morbidity in RUTF group |
Home-based therapy with RUTF is
associated with better outcomes for childhood malnutrition than is
standard therapy Grade: 1b |
| Diop, et al., 2003; Senegal(8);
Randomized controlled trial; 6-36 months; Inclusion: WFH < -2z without
edema or after edema had resolved |
RUTF versus F-100 (received F-75 for 1-4
days prior to enrolment); Total: 70, RUTF: 35, F-100: 35 |
Wt gain: 10.1 g/kg/d in F-100 versus 15.6
g/kg/d in RUTF group, Mean duration to recovery: 17.3 days in F-100
versus 13.4 days in RTUF |
RTUF can be used efficiently for the
rehabilitation of severely malnourished children. Grade: 1b |
| Commercial or Indigenous
Medical Nutrition Products versus Home based Foods |
Manary, et al., 2004; Malawi(9);>12
months; Inclusion: a) Children discharged from NRU after initial
treatment of infectious and metabolic problems,
b) HIV negative c) Tolerated test dose of RUTF |
RUTF versus RUTF supplement versus
maize-soy flour; Total: 282, RUTF: 69 RUTF supplement: 96 Maize soy:
117
Duration: Till recovery/death/ infection |
Recovery: 95% in RUTF versus 78% in
others: Wt Gain: 7.0 versus 4.9 g/kg/d Morbidity: 3.8% diarrhea in
RUTF versus 5.6% in others |
Home based therapy of malnutrition with
RUTF is successful. Grade: 1b |
| Simpore, et al., 2006; Burkina Faso (10);
Randomized controlled trial; 6-60 months; Inclusion: Undernourished
children after initial stabilization using NG feeds |
Spirulina, Misola (made of Millet, soya,
peanut kernel, sugar, salt) versus traditional foods; Total: 550
Spirulina: 170, Misola: 170 Spirulina+Misola: 170, Control: 40 |
All groups showed significant wt gain;
maximum in spirulina and Misola group |
Rehabilitation by Spirulina plus Misola
seems synergically favour the nutrition rehabilitation better than the
simple addition of protein and energy intake. Grade: 1b |
| Local versus Imported
Therapeutic Nutrition Products |
| Sandige, et al., 2004; Malawi(11);
Quasi-randomized controlled trials: 1-5 years; Inclusion: a) Initial
stabilization at NRU; b) WHZ < -2z for non-hospitalized subjects |
Imported RUTF (Plumpy nut) versus locally
produced RUTF; Total: 260, Local RUTF: 135; Imported RUTF: 125;
Duration: 14 weeks |
Recovery: 78%, Recovery (Local): 80%,
Recovery (imported): 75%, Wt gain: 5.2 versus 4.8 g/kg/d, Default: 5%
Failure, mortality and relapse: 11% |
Home-based therapy with RUTF was
successful. Locally produced and imported RUTF have similar efficacy.
Grade: 1b |
| Diop, et al., 2004; Senegal(12);
Randomized controlled trial; 6-59 months; Inclusion: a) Severe
malnutrition (WFH <70% and/or edema); b) Initial stabilization for 7
days at facility |
Local RUTF versus Imported RUTF; Total:
61, Individual sample sizes not mentioned |
Mean energy intake comparable:
3434.2 vs 3181.2 kJ; Mean wt gain: 7.9 vs 8.1 g/kg/d; Mean
duration of rehabilitation: 35 vs 33 days |
Home-based rehabilitation with locally
made RUTF was successful in promoting catch-up growth. Locally
produced RTUF was, at least as well accepted as the imported
version and lead to similar weight gain. Grade: 1b |
| Cohort Studies |
| Amthor, et al., 2009; Malawi(13);
Prospective cohort study; Inclusion: a) WFH< 70% or Kwashiorkor b)
Good appetite |
RUTF to provide 175 kcal/kg/d and protein
5.3g/kg/d; N = 826 Duration: 8 weeks |
Recovery (WFH 100%): 93.7% Mean wt gain:
2.7 g/kg/d Default: 3.6% Relapse: Not Mentioned |
Home-based therapy with RUTF administered
by village health aides is effective in treating mal-nutrition during
food crises in areas lacking health services Grade: 2b |
| Jilcott, et al., 2010; Uganda(14);
Evaluation study of a feeding program; 6-59 months; Inclusion: a) WFA
<3rd percentile; b) MUAC < 12 cm |
Locally produced RUTF; N=20 Duration: 5
weeks |
Energy intake: 684 kcal/day Mean wt gain:
2.5 g/kg/day |
Locally-produced RUF is a promising
strategy for community-based care of malnourished children. |
| Linemann, et al., 2007;
Malawi(15);Prospective cohort study; 6-60 months; Inclusion: a)
Moderate and severe malnutrition b) Good appetite |
Locally produced RUTF; treatment by
medical professionals versus community health aides; Duration: 8 weeks |
Recovery: 89%; Mean wt gain: 3.5g/kg/d
Default: 7%; Mortality: 1.4%; No differences in recovery rate based on
training of the staff |
Home-based therapy with RUTF yields
acceptable results without requiring formally medically trained
personnel. Grade: 2b |
| Ciliberto, et al., 2006; Malawi(16);
Prospective cohort study;1-5 years;Inclusion: a) Edematous
malnutrition, b) Good appetite, c) No complications |
Administration of RUTF at home; Total:
219; Duration: 8 weeks |
Recovery: 83%, Mortality: 5%, Mean wt
gain: 2.8g/kg/d |
Children with edematous malnutrition and
good appetite may besuccessfully treated with home-based therapy.
Grade: 2b |
| Chaiken, et al., 2006; Ethiopia(17);
Prospective cohort study; Age not mentioned; Inclusion: a) WFH < 70%
or bilateral edemaor MUAC<11 cm |
RUTF; N=5799 Followed up till recovery |
Recovery (WFH 80%) : 66% Default:
2.3%,Transferred: 8.8% Mortality 0.2% |
Recovery rates comparable with
international standards, coverage far exceeded that of traditional
center-based care. Grade: 2b |
| Collins, et al., 2002; Ethiopia(18);
Retrospective Cohort Study;6-120 months; Inclusion: a) WFH< 70% or
bilateral pitting edema |
RUTF Oral antibioticVitamin A, FA
Education; N=170 Followed up till recovery |
Recovery: 85%, Mean wt gain: 3.2 g/kg/d
Mortality: 4%; Default: 5%, Relapse: 6%; Mean time to recovery: 42
days |
Outpatient treatment exceeded
internationally accepted minimum standards for recovery, default, and
mortality rates. Time spent in the program and rates of weight gain
were not satisfactory. Outpatient care could provide a complementary
treatment strategy to therapeutic feeding centres. Grade: 2b |
| Briend, et al., 1999; Chad(19);
Prospective Cohort study; >12 mo Inclusion: a) WFH < 70% b) Gaining wt
for 3 days |
Alternative F100 feeds were replaced by
RUTF; 203 meals |
Energy intake 40·2 (SD 20·9) kcal/kg per
feed for RUTF versus 20·2 (11·5) kcal/kg per feed for F100 (p<0·001);
Total mean energy intake for the day was same |
RUTF might be useful in contaminated
environments or where residential management is not possible. Grade:
2b |
|
Consensus Statements |
| WHO, UNICEF, SCN informal consultation on
community based management of SAM, 2006 (20) |
-
It is highly desirable to manage the treatment of
severely malnourished children with no complications at home without
an inpatient phase.
-
RUTFs are useful to treat severe malnutrition
without complications in communities with limited access to
appropriate local diets for nutritional rehabilitation.
-
When families have access to nutrient-dense
foods, severe malnutrition without complications can be managed in
the community without RUTF by carefully designed diets using
low-cost family foods, provided appropriate minerals and vitamins
are given.
-
Treatment of young children should include
support for breastfeeding and messages on appropriate feeding
practices for infants and young children. Children under 6 months of
age should not receive RUTF or solid family foods. These children
need milk-based diets, and their mothers need support to reestablish
breastfeeding. They should not be treated at home.
Grade of Evidence: 5 |
| National Workshop on Development of
Guidelines for Home Based Care and Standard Treatment of Children
suffering from Severe Acute Malnutrition, 2006(21) |
-
Home based management could be feasible,
acceptable, and cost effective option for those children categorized
as “uncomplicated”.
-
Experience indicates that home management of SAMN
is likely to be successful in closely monitored conditions with
protocols, motivated staff and parents. An effective home based care
and treatment program should be comprehensive and simultaneously
address nutritional, medical, social, and economical aspects.
-
Energy dense therapeutic diets with low bulk are
essential in the initial phase of management. However, these should
be economical, available, and acceptable. These diets could be (i)
home based (prepared/modified from the family pot) or (ii)
ready to use therapeutic food (RUTF). Feeding should be frequent (6
to 8 times per 24 hours), active, and hygienic.
-
Commercially available international RUTF may not
be suitable (acceptable, cost effective and sustainable) for Indian
settings.
-
Multiple micronutrient and mineral
supplementation should be provided orally as per the WHO guidelines
for inpatient management of SAMN children.
Grade of Evidence: 5 |
Systematic Reviews
A 2008 systematic review(4) on severe malnutrition
identified 276 articles on management of SAM, of which 21 were eventually
included in the final analyses. Of these, nine studies evaluated the
efficacy of WHO guidelines for facility based management of severe acute
malnutrition; pooled data from these trials showed a reduction in
mortality (Risk Ratio 0.45; 95% CI 0.32, 0.62). The authors could not
identify any randomized controlled trials studying the effect of RUTF on
mortality. However, obtaining the observational data collected from 21
field programs on 23,511 children on community based management of SAM,
the authors showed the case fatality rate to be 4.1%, recovery rate was
79.4% and default was 11%; figures which were noted to be comparable to
data from facility based trials. The authors also conducted two
meta-analyses of RCTs conducted in children recovering from SAM as part of
this review. The first one compared the use of RUTF with F-100, and
revealed an advantage of weight gain of 3.0 g/kg/day (WMD = 3.0; 95% CI=
–1.70, 7.70) in favour of RUTF; however, the results were not
statistically significant (P=0.21). Meta-analyses comparing RUTF
with maize/soy flour included only one study(9) and found significantly
increased weight gain (WMD= 2.10 g/kg/day; 95% CI= 1.97, 2.23; P<0.001).
Another review, conducted by Ashworth, et al.(5),
studied the effectiveness of rehabilitating severely malnourished children
in community settings. Effectiveness was defined as mortality of less than
5% or weight gain of more than 5 g/kg/day. 16 trials of home based
management of SAM children were identified; of these, seven were
considered to be effective. Amongst these, two programs were home based
programs where no food was distributed, while 5 trials utilised RUTF. The
authors noted that all successful programs aimed at providing the child
with high protein, high energy diet at frequent intervals. None of the
programs within the existing health systems was effective without external
assistance. Home based treatment with nutrition education was shown to be
effective in Bangladesh, even without the provision of RUTF or any other
food. However, this involved considerable effort in educating the mothers.
Controlled Trials
A total of seven controlled trials were identified.
Three trials compared home based management of RUTF with the standard
practise using F-100 formula at therapeutic centres. Of these, two studies
started home therapy after initial stabilization at a facility(6-8). A
previously conducted meta-analysis showed an advantage of weight gain of
3.0 g/kg/day (WMD = 3.0; 95% CI= –1.70, 7.70) in favour of RUTF against
F-100; however, the results were statistically not significant(4). The
third study(8) in this group followed a purposive selection method, where
more sick patients and those with complications were referred to a
facility; subjects without complications and with good appetite were
selected for home based management using RUTF. Expectedly, the mortality
in the F-100 group was much higher (18.9% versus 92.7%) because of the
unequal baseline status between the two groups.
Two studies were identified that compared the efficacy
of therapeutic nutrition products with traditionally available foods at
home. Manary, et al.(9) compared RUTF with maize soy flour and
observed higher weight gain and recovery, and lower morbidity in RUTF
group, in comparison to home based foods. The study had been included in
the systematic review mentioned above and details are given in that
section. The second study(10) used Misola (a local product made
from millet, soya, peanut kernal, sugar and salt) that supplies energy
almost equivalent to conventional RUTFs. The authors found that Misola
fortified with Spirulina led to higher weight gain, in comparison to
use of traditional foods.
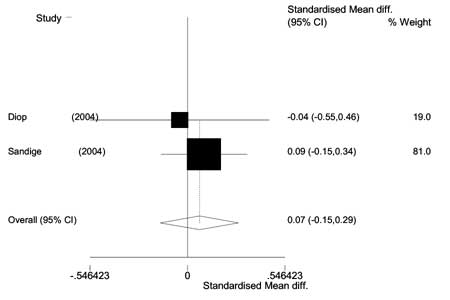
Two trials(11,12) compared the efficacy of a locally
made RUTF with imported RUTF. A meta-analysis was done from the data
derived from the two studies doing a comparative assessment of the impact
of locally made RUTF and imported RUTF. The pooled data from the two
studies done amongst 321 subjects, of whom 165 received locally made RUTF
and 156 received imported RUTF, showed no difference in the weight gain
between the two groups (WMD = 0.07 g/kg/d; 95% CI = -0.15, 0.29, 1.244,
P=0.15) (Fig 1).
 |
|
Fig. 1 Forest Plot showing the
effectiveness of imported RUTF in comparison with local RUTF in
weight gain of severe malnourished children. |
Observational Trials
A total of 7 observational trials(13-19) were
identified. Of these, one trial(19) estimated the adequacy of energy
intake with ready to use foods in comparison to F-100 and found them to be
comparable. Most of the trials (4 out of 5) reported a recovery rate
(recovery variably defined by the authors) of more than 80%.
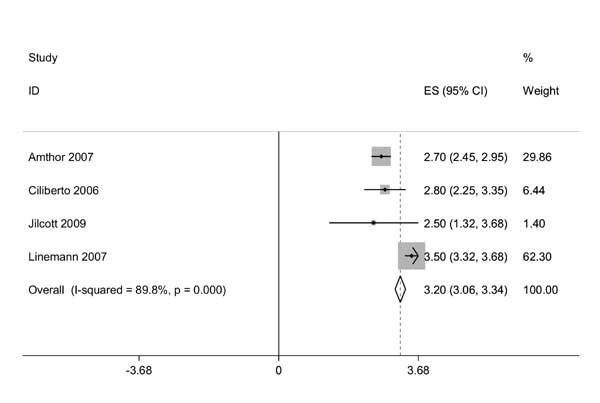
A pooled analysis of data from 5 studies (giving
information on 9145 severely malnourished children) reveals a recovery
rate of 88.3%, mortality of 0.7%, default rate of 3.6% and 6.7% babies had
failure of treatment or needed referral to a facility. Using meta-analytic
methods the pooled mean weight gain with the use of RUTF was 3.2 g/kg/day
(95% CI 3.06, 3.34 g/kg/d) (Fig 2). Of these trials, one(14)
used a locally designed RUTF and found weight gain comparable, as with the
use of commercially available RUTFs in other trials.
 |
|
Fig. 2 Forest Plot showing the
pooled estimates for weight gain in severe malnourished children
using RUTF. |
Consensus Statements
Two consensus statements(20,21) were identified from
published literature. Both the statements emphasized the need to treat
uncomplicated severely malnourished children at home, and on the efficacy
of therapeutic nutrition products like RUTF for this purpose. They also
stated the need for micronutrient supplementation as per WHO guidelines,
exclusive breastfeeding in the first 6 months of life, monitoring of the
children to ensure compliance and adequate response to treatment and need
to develop local products to increase acceptability and decrease cost.
Discussion
Review of presently available published peer reviewed
literature shows that the use of ‘therapeutic nutrition products’ like
RUTF are efficacious in treating children with severe acute malnutrition,
who do not have any associated complications, and during the
rehabilitation phase when prolonged hospitalization may not be desirable.
Systematic reviews and randomized controlled trials on the topic show that
this modality of treatment may be as efficacious as standard (WHO)
treatment using F-100. Furthermore, these products are more effective than
home based foods with lower energy density in treating SAM. Locally
designed ready to use foods are as effective as the commercially available
products. The overall recovery rate with the use of RUTF is more than 85%
with a mortality of less than 1%.
However, the currently available level of evidence does
have some drawbacks that preclude the direct incorporation of such a
strategy into a program or a policy, and even its extendibility to India.
First is the fact that there is paucity of data, that too of robust
quality, available on the topic. Most of the information is available from
observational studies conducted in disaster situations, where no other
alternative strategy was feasible. The other noteworthy issue is the fact
that all the studies available so far were conducted in Africa. The
results of extending it to countries like India, in non-emergency
situations, with unknown efficacy and acceptability, are at present
unpredictable.
A number of studies, especially the controlled trials
which constitute a higher level of evidence are conducted in controlled
situations, under the supervision and monitoring of health care workers.
No doubt, this enables early identification of complications and
institution of early treatment, wherever indicated but digresses from the
basic rationale of using this strategy in areas where the health
infrastructure is poor or non-existent. Such supervised management also
increases the cost of management of SAM children. Based on the cost of
RUTF alone, Ashworth, et al.(5) estimated the cost to rehabilitate
a SAM child to be $55; for a HIV positive child it would double to $110.
To put it in perspective, in 2006, the per capita health care cost spent
by India was $39(23). These are substantial costs for the health system of
any developing country to absorb and emphasize the need for product
innovation at a local level.
The use of home treatment, using medical nutrition
products, as a public health strategy, therefore, should be treated as a
possibility in infancy, with its need to study its feasibility and cost
effectiveness in the Indian setting in an operational research format,
before suggesting its integration into the current health programs. The
effectiveness of cheaper locally designed ready to use foods is
encouraging, and should stimulate the scientific community to design
appropriate food(s) which are culturally acceptable in various parts of
our large country, as well as cost-effective.
Most important is the need to communicate to the policy
planners the urgency to address the problem of severe acute malnutrition.
Despite the fact that severe malnutrition is often a co-morbidity in large
proportion of avoidable child mortality, it does not get the attention it
deserves. It should be emphasized that the treatment of SAM is cost
effective – in fact, even hospital based management of SAM is more cost
effective in reducing mortality than many other child survival
intervention programs including the extremely visible vitamin A
supplementation program(24,25). The availability of alternative strategies
like home based management using locally made therapeutic nutrition
products is likely to add to the cost effectiveness. India needs
multi-pronged strategies to address the problem of severe malnutrition,
given the geo-graphic, cultural and financial barriers that exist across
this large country; home based management is likely to be one of them.
Funding: None.
Competing Interests: None stated.
|
EURECA Conclusion in the Indian Context
•
The presently available evidence, drawn from limited number of
studies, all conducted in Africa, on home based management of
severe acute malnutrition using therapeutic nutrition products
suggests that it is safe and efficacious.
•
There is need for further
research, particularly in product innovation and operational
issues to establish its efficacy and cost effectiveness in the
Indian context.
|
References
1. International Institute for Population Sciences.
National Family Health Survey 3, 2005-2006. Mumbai, India: IIPS; 2006.
2. Pelletier DL. The relationship between child
anthropometry and mortality in developing countries: implications for
policy, programs and future research. J Nutr 1994; 124 (suppl):
2047S–2081S.
3. Collins S, Dent N, Binns P, Bahwere P, Sadler K, and
Hallam A. Management of severe acute malnutrition in children. Lancet
2006; 368: 1992-2000.
4. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K,
et al. What works? Interventions for maternal and child undernutrition
and survival. Lancet 2008; 371: 417-440.
5. Ashworth A. Efficacy and effectiveness of
community-based treatment of severe malnutrition. Food Nutr Bull 2006 Sep;
27(3 Suppl): S24-48.
6. Gaboulaud V, Dan-Bouzoua N, Brasher C, Fedida G,
Gergonne B, Brown V. Could nutritional rehabilitation at home complement
or replace centre-based therapeutic feeding programmes for severe
malnutrition?J Trop Pediatr 2007; 53: 49-51.
7. Ciliberto MA, Sandige H, Ndekha MJ, Ashorn P,Briend
A, et al. Comparison of home-based therapy with ready-to-use
therapeutic food with standard therapy in the treatment of malnourished
Malawian children: a controlled, clinical effectiveness trial. Am J Clin
Nutr 2005; 81: 864 -870.
8. Diop EHI, Dossou NI, Ndour MM, Briend A, Wade S.
Comparison of the efficacy of a solid ready-to-use food and a liquid,
milk-based diet for the rehabilitation of severely malnourished children:
a randomized trial. Am. J. Clin, Nutr. 78: 302-307.
9. Manary MJ, Ndkeha MJ, Ashorn P, Maleta K, Briend A.
Home based therapy for severe malnutrition with ready to use food. Arch.
Dis. Child. 2004;89;557-561.
10. Simpore J, Kabore F, Zongo F, Dansou D, Bere A,
Pignatelli S, et al. Nutrition rehabilitation of undernourished
children utilizing Spiruline and Misola. Nutr J. 2006 Jan 23; 5: 3.
11. Sandige H, Ndekha MJ, Briend A, Ashorn P, Manary MJ.
Home-based treatment of malnourished malawian children with locally
produced or imported ready-to-use food. JPGN 2004; 39: 141–146.
12. Diop EI, Dossou N, Briend A, Yaya NA, Ndour MM,
Wade S. Home-based rehabilitation for severely malnourished children using
locally made ready-to-use therapeutic food (RTUF). Pediatr
Gastroenterology, Hepatology and Nutrition: Second World Congress, Paris,
France, 2004.
13. Amthor RE, Cole SM, Manary MJ. The use of home
based therapy with ready to use therapeutic food to treat malnutrition in
a rural area during a food crisis. J Am Diet Assoc 2009; 109: 464-467.
14. Jilcott SB, Ickes SB, Ammerman AS, Myhre JA.
Iterative design, implementation and evaluation of a supplemental feeding
program for underweight children ages 6-59 months in Western Uganda.
Matern Child Health J. 2010; 14: 299-306.
15. Linemann Z, Matilsky D, Ndekha M, Manary M, Maleta
K, Manary MJ. A large scale operational of home based therapy with ready
to use therapeutic food in childhood malnutrition in Malawi. Mat Child
Nutr 2007; 3: 206-215.
16. Ciliberto MA, Manary MJ, Ndekha MJ, Briend A,
Ashorn P. Home-based therapy for oedematous malnutrition with ready-to-use
therapeutic food. Acta Paediatr. 2006; 95: 1012-1015.
17. Chaiken MS, Deconinck H, Degefie T. The promise of
a community-based approach to managing severe malnutrition: A case study
from Ethiopia. Food Nutr Bull 2006 Jun; 27: 95-104.
18. Collins S, Sadler K. Outpatient care for severely
malnourished children in emergency relief programmes: a retrospective
cohort study. Lancet. 2002; 360 : 1824-1830.
19. Briend A, Lacsala R, Prudhon C, Mounier B, Grellety
Y, Golden MHN. Ready-to-use therapeutic food for treatment of marasmus.
Lancet 1999; 353: 1767-1768.
20. Prudhon C, Prinzo ZW, Briend A, Daelmans BMEG,
Mason JB. Proceedings of the WHO, UNICEF, and SCN Informal Consultation on
Community-Based Management of Severe Malnutrition in Children. Food Nutr
Bull 2006; 27(Suppl 3): S99-S108.
21. National Workshop on "Development of Guidelines for
Effective Home Based Care and Treatment of Children Suffering from Severe
Acute Malnutrition" Indian Pediatr 2006; 43: 131-139.
22. CEBM Centre for Evidence Based Medicine. Oxford
Centre for Evidence Based Medicine – Levels of Medicine (March 2009).
Available at: http://www.cebm.net/index.aspx?o=1025. Accessed on May 15,
2010.
23. WHO Statistical Information System. Available at:
http://apps.who.int/whosis/data/Search.jsp. Accessed on May 18 th,
2010.
24. Jha P, Bangoura O, Ranson K. The cost-eff
ectiveness of forty health interventions in Guinea. Health Policy Plan
1998; 13: 249-262.
25. Tectonidis M. Crisis in Niger-outpatient care for severe acute
malnutrition. N Engl J Med 2006; 354: 224-227.
|
|
|
 |
|

