|
Leni Grace Mathew
Thomas Cherian
Vivi M. Srivastava
P. Raghupathy
From
the Department of Child Health and Department of Pathology, Christian Medical College and Hospital, Vellore, TamiInadu, India.
Reprint requests: Dr. Thomas Cherian, Professor, Department of Child Health, Christian Medical College and Hospital, Vellore, Tamilnadu, India.
Manuscript Received: October 7,1997; Initial review completed: December 19, 1997;
Revision Accepted: February 11, 1998
Kikuchi-Fujimoto Disease (KFD) is a rare entity of uncertain etiology, which commonly presents as fever and lymphadenopathy and is unresponsive to antibiotic
therapy(1). Although it usually follows a benign course, KFD has been repeatedly
misdiagnosed as malignant Iymphoma(2). Its association with SLE has also been described in the literature(I,3). However, KFD presenting as aseptic meningitis is rare, with only two previous reports from Japan(4,5) and one from the USA(6). We report here a 12-year-old girl with Kikuchi disease and aseptic meningitis.
Case Report
A twelve-year-old girl presented in April 1996 with high-grade intermittent fever for 25 days, headache for 10 days and projectile vomiting for one day. There was
no history of rash or joint pain. On physical examination, she was febrile and
fully conscious. She had no pallor, icterus or rash. Her BP was 100/60 mm Hg, pulse rate 88/ min and respiratory rate 52/min. The left posterior cervical (n
=
2) and left supraclavicular (n
=
1) lymph nodes were enlarged 1.5 cm in diameter and were tender. Examination of throat and ears was normal. Neurological examination revealed bilateral papilloedema and a positive Kernig's sign. Examination of other systems was normal. The diagnoses considered were tuberculous meningitis, viral meningitis or a collagen vascular disease.
Investigations revealed ESR of 105 mm in the first hour, total leukocyte count of 5800/cu mm, differential count of neutrophil 90%, lymphocytes 8%, monocytes 1%, and Platelet count 313,OOO/cu mm. Bone marrow smear was normal. WidaI, Paul Bunnell and Weil-Felix tests were negative. CSF analysis showed 100 leukocytes/cu mm (all lymphocytes), RBC-5/cu mm, glucose-55 mg/dl and protein 24 mg/dl. Immunofluorescent staining of the. CSF smear for cryptococcus was negative. Bacterial, viral, fungal and AFB cultures of the CSF were sterile. CSF ELISA for M. tuberculosis
antibody was negative. ANA and LE
cell preparation were negative. CT scan of the brain did not show any abnormality.
The patient was treated with ten days of intravenous cefotaxime following which
she became asymptomatic and hence was discharged. However, she returned 15 days
later with one-week history of high-grade intermittent fever and persistent
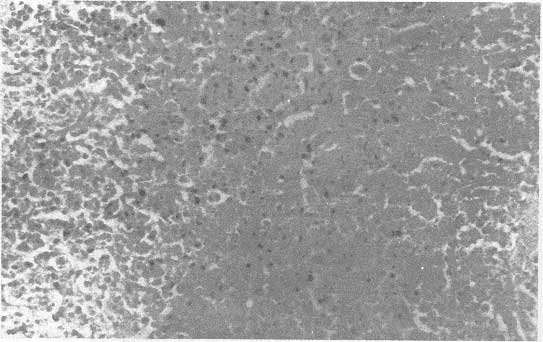
tender cervical lymphadenitis. Lymph node biopsy was performed which showed histiocytic necrotizing lymphadenitis without
granulocytic infiltration, consistent with Kikuchi's disease (Fig. 1).
The patient was given a short course of prednisolone at a dose 1 mg/kg for two weeks, which was then tapered over the next two weeks. She became afebrile within five days after starting prednisolone and lymphadenopathy subsided within 10 days. She was followed up closely for any symptoms and signs of SLE. At follow up 14 months later, she had been asymptomatic except for one episode of a non- specific febrile illness in May 1997.
Discussion
KFD was originally described in Japan in 1972(7,8). The disease preferentially affects young women under the age of 30
years(1). The etiology of KFD is unknown(1). The disease usually runs a benign
course with fever and lymphadenopathy, resolving spontaneously after 4-6 months. Less frequent manifestations include generalized lymphadenopathy, hepatosplenomegaly, nausea, vomiting, weight loss and night
sweats(1). There is one case report of fatal Kikuchi's disease. Death was due to cardiac failure which was attributed to cytokine mediated myocardial damage(9). The presentation of KFD with aseptic meningitis is very unusual. There are only three reported cases in the world literature(4,5,6). In two of these, which are reported in the Japanese literature the cause of aseptic meningitis is not clear(4,5). In the remaining case, aseptic meningitis was thought to be an autoimmune phenomenon(6). The patient had KFD with autoimmune phenomena and meningitis. KFD has been reported to occur in patients with preexisting SLE and also been known to evolve into SLE(1,3,10). It is therefore
recommended that patients be closely followed up far signs of SLE for several years after developing KFD.
CNS lupus presenting with headache and aseptic meningitis is well known. Since our patient presented with the above features, she was investigated
to rule out SLE; all the screening tests far SLE were negative. During a follow up for a period of one year after the onset of disease, she did not have any
other manifestatians of SLE. Therefore, in her the pathogenesis of aseptic meningitis remains uncertain, though continued follow up far manifestatians for SLE are required.
 |
|
Fig. 1.
The lymph
node
contained foci of necrosis in the paracortex associated with karyorrhectic debris and all
infiltrate of histiocytes and lymphocytes. There was a paucity of neutrophils
and plasma cells.
(H&E
x 200). |
There are very few other conditions which would mimic this presentation of KFD. Granulomatous lymphadenitis and neurologic manifestatian have been described in Cat scratch disease (CSD). However, the histopathology of the lymphnodes in CSD is quite distinct from KFD(11). Lymphnode biopsy in our patient did not show any granulomatous inflammation
to suggest CSD.
KFD is generally a self-limiting disease and no specific treatment is recommended. Since our patient had persistent fever and lymphadenopathy lasting far 50 days and because of our concern about autoimmune disease, a trial of prednisolone was given. She had a dramatic response
to this treatment with resolution of fever and
lymphadenopothy within one week. The symptoms did not recur even though the dose of prednisolone was tapered after
two weeks and the medication stopped after another two weeks. Thus our patient showed good response
to steroid therapy. Further trials are required to evaluate the efficacy of short courses of prednisolone in the treatment of KFD.
|
1.
Dorfman RF, Berry GJ. Kikuchi's histiocytic necrotizing lymphadenitis: An analysis .of 108 cases with emphasis an differential diagnosis. Semin Diagn
PathaI 1988; 5: 329-345.
2.
Chamulak GA, Brynes RK, Nathwani BN. Kikuchi-Fujimoto disease mimicking malignant lymphoma. Am
J
Surg Pathal
1990; 14: 514-523.
3.
Ramahi KM, Karra A, Ali MA. Kikuchi disease and its association with systemic lupus erythematosus. Lupus 1994; 3: 409- 411.
4.
Yamsaki Y, Chiba S, Misago M, Tsuda T, Oda S, Oda E, et al. A case of subacute necrotizing lymphadenitis associated with
aseptic meningitis. Jpn Sac Intern Med. 1986; 75: 687-690.
5.
Maeda T, Ashie T, Ishiyama N, Kikuri K.
A
case
of necrotizing lymphadenitis associated with aseptic meningitis. Jpn Sac Intern Med. 1987; 76: 1073-1077.
6.
Debley JS, Rozansky DJ, Miller ML, Katz BZ. Histiocytic necrotizing lymphadenitis with autoimmune phenomena
and meningitis in a 14 year old girl. Pediatrics 1996; 98: 130-133.
7.
Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes: A clinicopathological study. Nippon Ketsucki Gakkai
Zassho 1972; 35: 379-380.
8.
Fujimata Y, Kajima Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis. Naika 1972; 30: 920-927.
9.
Chan JKC, Wang KC, Chi-sing NG. A fatal case of multicentric Kikuchi's histiocytic necrotizing lymphadenitis. Cancer 1989;63:1856-1862.
10.
Hoffman A, Kirn E, Kuerten A. Active human herpes virus-6 infection associated with Kikuci-Fujimoto's
disease and systemic lupus erythematosus. In Vivo 1991; 5: 265-269.
11.
Mafgileth AM. Catoscratch Disease. Adv Pediatr Infect Dis 1993; 8: 1-21.
|
